Eczema is a tricky condition that affects an estimated 10-20% of infants in the U.S. And, though it’s less common in adults (only about 3% of American adults have eczema), chances are we’ve all met someone with this condition.
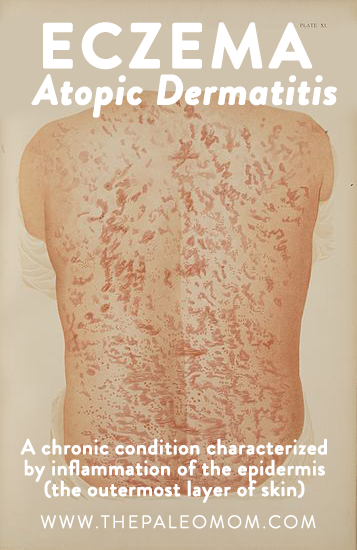 Eczema, also called atopic dermatitis, is a chronic condition characterized by inflammation of the epidermis (the outermost layer of skin). This inflammation, at its heart an immune reaction, can present itself in the form of a multitude of symptoms, including: redness, swelling, itching, dryness, crusting, flaking, blistering, cracking, oozing, or bleeding. Someone with eczema might experience it on any place in the body, and it can manifest as almost any size on the skin.
Eczema, also called atopic dermatitis, is a chronic condition characterized by inflammation of the epidermis (the outermost layer of skin). This inflammation, at its heart an immune reaction, can present itself in the form of a multitude of symptoms, including: redness, swelling, itching, dryness, crusting, flaking, blistering, cracking, oozing, or bleeding. Someone with eczema might experience it on any place in the body, and it can manifest as almost any size on the skin.
What do we know of the mechanism underlying eczema? Scientists used to believe that it was an immune system disorder that featured overactive T cells, but now we know that eczema is actually a result of a structural defect in the epidermis: abnormalities in the outermost layer make it more permeable to toxins and antigens. Even more specifically, the defect is the result of improperly formed proteins called filaggrins (more on that later!). Once irritants from the environment have permeated the outermost layer and bypassed the filaggrins, keratinocytes (a specialized kind of skin cell) produce cytokines to inform the immune system that there is an intruder. Then, immune system cells travel to the skin and induce an immune reaction, which includes the release of IgE antibodies and in turn promotes more of an inflammatory reaction! Yes, eczema can be a pretty vicious immune cycle; and although it’s not autoimmune, it is a condition that can benefit from the autoimmune protocol. However, there are simple tweaks to your lifestyle, nutrition, and skincare routine that can make all the difference!
1. Up Your Sun Exposure (AKA Vitamin D!)
 One of the easiest ways to improve eczema is to get outside and get some sunshine. Scientific studies have shown that people with eczema are more likely to be deficient in vitamin D, an incredibly potent fat-soluble vitamin that I’ve written about many times on the blog (see Why Sun Exposure Is So Important) and extensively in my Go to Bed e-book. Vitamin D is a steroid hormone that regulates the expression of over 200 genes, plays a key role in mineral metabolism, is essential for bone mineralization, and is a key regulator of the immune system. It also regulates cell growth, including the epithelial cells that make up the epidermis. So, vitamin D works at two key places that are affected in eczema: the immune system, which is likely going haywire at the surface of the skin, and the skin itself!
One of the easiest ways to improve eczema is to get outside and get some sunshine. Scientific studies have shown that people with eczema are more likely to be deficient in vitamin D, an incredibly potent fat-soluble vitamin that I’ve written about many times on the blog (see Why Sun Exposure Is So Important) and extensively in my Go to Bed e-book. Vitamin D is a steroid hormone that regulates the expression of over 200 genes, plays a key role in mineral metabolism, is essential for bone mineralization, and is a key regulator of the immune system. It also regulates cell growth, including the epithelial cells that make up the epidermis. So, vitamin D works at two key places that are affected in eczema: the immune system, which is likely going haywire at the surface of the skin, and the skin itself!
Save 80% Off the Foundations of Health
Expand your health knowledge on a wide range of topics relevant to you, from how to evaluate scientific studies, to therapeutic diet and lifestyle, to leaky gut and gut microbiome health, to sustainable weight loss, and much more!!!

Why is it important to get your vitamin D from sun exposure for eczema (as opposed to taking it orally)? There is one pretty big reason: since vitamin D is actually made inside skin cells, it’s like giving the inflamed skin a little dose of just the medicine it needs, right at the source. This notion is supported by the fact that dermatologists will even use phototherapy (exposure to certain wavelengths of light that promote vitamin D synthesis) on patches of eczema to treat it, and this method is quite effective.
So, getting outside and exposing the inflamed areas to the sun could be a very simple lifestyle change that could make a big difference! For people with fair skin, just 10 minutes of sun exposure is enough to get the recommended 10,000 international units (IUs) per day (and the logic follows such that people with darker skin need incrementally more according to their skin type). We know that a safe amount of sun exposure is great for our health; the aging and cancer-causing aspect comes from sunburn, which ends up damaging our DNA, not in the relatively brief sun exposure discussed here. If unable to get outside (or faced with a particularly brutal winter or working a night shift), taking vitamin D3 is still a good alternative. In fact, scientific studies have shown that doses of vitamin D3 of as little as 1600 IU per day is effective at alleviating eczema symptoms. I recommend getting a vitamin D3 supplement that contains the vitamin in a healthy oil (since it is fat-soluble, after all) and making sure to re-check levels at least every few months since too much vitamin D can also be a problem. We can also get vitamin D from some of the most nutrient-dense Paleo foods, including liver, egg yolks, and fatty fish.
2. Make Glycine Your Favorite Amino Acid
 Amino acids are the building blocks of proteins, which are the essential for every single cellular unit in our body. And while certainly, an optimal human diet includes ample of all twenty of the amino acids we need to make proteins, altering our diet to increase the amount of specific amino acids has been shown in the literature to help with targeted concerns, such as injury recovery or gut healing, because it gives our bodies the exact tools they need to accomplish the task of building new proteins.
Amino acids are the building blocks of proteins, which are the essential for every single cellular unit in our body. And while certainly, an optimal human diet includes ample of all twenty of the amino acids we need to make proteins, altering our diet to increase the amount of specific amino acids has been shown in the literature to help with targeted concerns, such as injury recovery or gut healing, because it gives our bodies the exact tools they need to accomplish the task of building new proteins.
Glycine is the smallest amino acid of them all, making it completely necessary for health. While it isn’t strictly an essential amino acid according to the biochemistry (meaning that we can make our own glycine if we need to), it’s better to eat complete protein sources that contain glycine to ease the metabolic burden of generating our own amino acids (meaning, our bodies just can’t keep up with demand if we don’t get enough from our diets).

In the case of eczema, a deficiency in glycine might be just one of the reasons that the epidermis is compromised; scientific studies have shown that filaggrin proteins are rich in glycine, plus we know that glycine is absolutely critical for properly-structured connective tissues (like skin!) in that it helps to bind together the unique proteins of the extracellular matrix.
Eating a diet rich in glycine is easy to accomplish within a Paleo lifestyle, because certain high-profile foods are super-rich in this little amino acid! I’m thinking of one in particular: bone broth! Since bone broth is made from connective tissues of animals, it is incredibly rich in glycine. There is even more information about this in my post, Why Broth is Awesome.
If you need more convenience, try supplementing with Paleovalley Bone Broth Protein!
3. Opt for Seafood
 Focusing on glycine isn’t the only way to tweak the diet in order to potentially improve eczema symptoms. Another method is to reduce our inflammatory signaling by focusing on getting more omega-3s in our diet (and this really goes for anyone, even those of us not dealing with eczema!). Omega-3 fatty acids are polyunsaturated fatty acids with a double bond structure that is unique. This particularly class of fatty acids are incredibly important for immune system signaling, because they are used to reduce immune responses in the body. These fatty acids are stored in cellular membranes, where they compete for space with omega-6 fatty acids. Both omega-6s and omega-3s are then converted into signaling molecules that instruct the immune system, omega-6s make signaling molecules that ramp up the immune system and inflammation whereas omega-3s make signaling molecules that are very weak stimulators of inflammation . Omega-6s are kind of like the angry cousins of omega-3s: they aggravate the immune system and exaggerate inflammatory responses, but they are still necessary for a healthy immune response. So, having a balance of omega-3s and omega-6s is essential for a well-tuned immune system, and making sure that our intake is as close to a ratio of 1:2 as possible is a really good idea, especially for anyone struggling with eczema.
Focusing on glycine isn’t the only way to tweak the diet in order to potentially improve eczema symptoms. Another method is to reduce our inflammatory signaling by focusing on getting more omega-3s in our diet (and this really goes for anyone, even those of us not dealing with eczema!). Omega-3 fatty acids are polyunsaturated fatty acids with a double bond structure that is unique. This particularly class of fatty acids are incredibly important for immune system signaling, because they are used to reduce immune responses in the body. These fatty acids are stored in cellular membranes, where they compete for space with omega-6 fatty acids. Both omega-6s and omega-3s are then converted into signaling molecules that instruct the immune system, omega-6s make signaling molecules that ramp up the immune system and inflammation whereas omega-3s make signaling molecules that are very weak stimulators of inflammation . Omega-6s are kind of like the angry cousins of omega-3s: they aggravate the immune system and exaggerate inflammatory responses, but they are still necessary for a healthy immune response. So, having a balance of omega-3s and omega-6s is essential for a well-tuned immune system, and making sure that our intake is as close to a ratio of 1:2 as possible is a really good idea, especially for anyone struggling with eczema.
The good news is that we can get our omega-3s from our food! But, it’s important to note the different types of omega-3s. There are, in fact, three types of omega-3s: ALA, EPA, and DHA. ALA is commonly found in plant oils such as flaxseed oil and canola oil, but, despite some media attention, ALA isn’t a particularly useful form of omega-3 (our bodies need to convert these fatty acids to either EPA or DHA anyways, and the conversion rate isn’t very good). So, it’s better to go ahead and choose fat sources that are rich in EPA and DHA when we can. Some of the best sources are wild-caught, fatty fish; grass-fed beef; and pasture-raised eggs.
4. Choose a Healing Skin Cream
 Okay, there is another (kind of obvious) option for eczema: use something topically! Since eczema can be tricky due to its “leaky skin” etiology, it’s absolutely critical that someone struggling with eczema be utilizing healing, anti-inflammatory skincare. Since eczema is related to both skin cell integrity and immune system function, choosing a topical product that nourishes without potentially triggering any additional immune reactions is extremely critical.
Okay, there is another (kind of obvious) option for eczema: use something topically! Since eczema can be tricky due to its “leaky skin” etiology, it’s absolutely critical that someone struggling with eczema be utilizing healing, anti-inflammatory skincare. Since eczema is related to both skin cell integrity and immune system function, choosing a topical product that nourishes without potentially triggering any additional immune reactions is extremely critical.
YoRo Naturals is a brand I trust that accomplishes just this balance. Their Organic Manuka Skin Soothing Cream is luxuriously creamy yet very soothing for the skin, and it was created with high quality ingredients known to help with eczema. Their spotlight ingredient, manuka honey, is honey from bees that pollinate the manuka tree of New Zealand, which is a relative of tee tree (another well-known anti-inflammatory plant known for its notoriously pungent smell – something that is completely absent in manuka oil!).  Manuka honey is known to be amazing for skin conditions due to its remarkably high methylgyoxal content. Methylglyoxal is an enzyme that produces hydrogen peroxide. This compound is incredibly potent in eliminating bacterial growth, and, since we know that eczema is at least in part a response to bacterial antigens entering through the skin, manuka honey can be very therapeutic for acute eczema! In this organic skin cream, there is both manuka honey AND manuka oil, which is even more anti-inflammatory than tea tree oil. There is even specific clinical evidence for using manuka honey blends on eczema: a previous study examined a combination of manuka honey, beeswax, and olive oil and found that symptoms were significantly improved within 2 weeks in 80% of patients. The Eczema Company’s formula includes all of those healing ingredients!
Manuka honey is known to be amazing for skin conditions due to its remarkably high methylgyoxal content. Methylglyoxal is an enzyme that produces hydrogen peroxide. This compound is incredibly potent in eliminating bacterial growth, and, since we know that eczema is at least in part a response to bacterial antigens entering through the skin, manuka honey can be very therapeutic for acute eczema! In this organic skin cream, there is both manuka honey AND manuka oil, which is even more anti-inflammatory than tea tree oil. There is even specific clinical evidence for using manuka honey blends on eczema: a previous study examined a combination of manuka honey, beeswax, and olive oil and found that symptoms were significantly improved within 2 weeks in 80% of patients. The Eczema Company’s formula includes all of those healing ingredients!
 Like most conditions involving the immune system, there are a lot of ways that behaviors and choices can help or hinder our healing. Utilizing these nutritional strategies and getting enough sun exposure can be very useful in attempting to manage eczema in infants, children, and adults; adding in the right topical treatment, especially one that is backed by scientific research, adds even more potency to this anti-eczema plan. With some trial and error (as well as some patience!), consider eczema symptoms combated! For more information about regulating and improving immune system function and how the Paleo diet accomplishes this, see my book, The Paleo Approach.
Like most conditions involving the immune system, there are a lot of ways that behaviors and choices can help or hinder our healing. Utilizing these nutritional strategies and getting enough sun exposure can be very useful in attempting to manage eczema in infants, children, and adults; adding in the right topical treatment, especially one that is backed by scientific research, adds even more potency to this anti-eczema plan. With some trial and error (as well as some patience!), consider eczema symptoms combated! For more information about regulating and improving immune system function and how the Paleo diet accomplishes this, see my book, The Paleo Approach.
Citations
Al-waili NS. Topical application of natural honey, beeswax and olive oil mixture for atopic dermatitis or psoriasis: partially controlled, single-blinded study. Complement Ther Med. 2003;11(4):226-34.
Boguniewicz M. Atopic dermatitis: beyond the itch that rashes. Immunol Allergy Clin North Am. 2005 May;25(2):333-51.
Elias PM and Steinhoff M “Outside-to-Inside” (and Now Back to “Outside”) Pathogenic Mechanisms in Atopic Dermatitis. J Invest Dermatol. 2008 May; 128(5): 1067–1070.
Gethin GT, Cowman S, Conroy RM. The impact of Manuka honey dressings on the surface pH of chronic wounds. Int Wound J. 2008;5(2):185-94.
Javanbakht MH, Keshavarz SA, Djalali M, et al. Randomized controlled trial using vitamins E and D supplementation in atopic dermatitis. J Dermatolog Treat. 2011;22(3):144-50.
Lee SA, Hong S, Kim HJ, Lee SH, Yum HY. Correlation between serum vitamin d level and the severity of atopic dermatitis associated with food sensitization. Allergy Asthma Immunol Res. 2013;5(4):207-10.
Mesquita Kde C, Igreja AC, Costa IM. Atopic dermatitis and vitamin D: facts and controversies. An Bras Dermatol. 2013;88(6):945-53.
Pike MG et. al. Increased intestinal permeability in atopic eczema. J Invest Dermatol. 1986 Feb;86(2):101-4.
Tomblin V, Ferguson LR, Han DY, Murray P, Schlothauer R. Potential pathway of anti-inflammatory effect by New Zealand honeys. Int J Gen Med. 2014;7:1