A new study in the journal Pediatrics has the gluten-free/celiac disease world buzzing (this article has been published on dozens of websites). The study concludes that early introduction of small amounts of gluten while still breastfeeding reduces the risk of celiac disease.
The study looked at two cohorts of Swedish 12-year olds, the first were a group born in 1993 during an epidemic of celiac disease (during the epidemic, the incidence of celiac disease increased from 1 in 100 to 3.3 in 100, believed attributable to changes in government recommendations for the age of gluten introduction to 6 months old, combined with a concurrent increase in the gluten content of baby foods) and the second were a group born in 1997 after the epidemic (after the government revised their guidelines to lower the age of gluten introduction to 4 months and the amount of gluten in baby foods was reduced). The study sought to determine the impact of breastfeeding in relation to gluten introduction on the future development of celiac disease.
The hypothesis of the study is well summarized in this statement from the discussion section.
“Oral tolerance to an antigen develops early in life, and celiac disease can be viewed as a failure to develop oral tolerance to gluten, or a later loss of this tolerance. The development of oral tolerance is a complex immunologic process involving interactions between genetic factors and environmental and lifestyle exposures, such as bacterial gut colonization and infant feeding.”
And this idea is what has my inbox flooded with questions. If oral tolerance for gluten develops early in life and breastfeeding helps with the development of oral tolerance, is it better to give our Paleo babies some gluten now? Will that help prevent celiac disease and other autoimmune diseases?
To answer this question, let me first summarize exactly what this paper shows about the relation between breastfeeding, gluten introduction and celiac disease. Over 13000 children were enrolled in the study. The incidence of celiac disease was 2.8 in 100 in the 1993 cohort versus 2.2 in 100 in the 1997 cohort. The median age of gluten introduction was the same (5 months old) between both cohorts. But, the infants in the 1997 cohort were breastfed an average of 2 months longer than the 1993 cohort (age of weaning increased from an average of 7 months to an average of 9 months between 1993 and 1997). What this means is that the number of babies who were breastfed during and beyond gluten introduction was significantly larger in the 1997 cohort (number of babies breastfed beyond gluten introduction was 70% vs 78% in the 1993 and 1997 cohorts, respectively). From this, the authors conclude that introducing gluten before weaning reduces the risk of celiac disease.
 This is an interesting observation and I think that this Op Ed piece in the NY Times provides a possible explanation for the result that is not thoroughly discussed in the original paper: it’s all about the gut microbiota.
This is an interesting observation and I think that this Op Ed piece in the NY Times provides a possible explanation for the result that is not thoroughly discussed in the original paper: it’s all about the gut microbiota.
The most current understanding of celiac disease (well summarized in this paper, which sadly requires a subscription to view) is that the development of celiac disease (and indeed all autoimmune diseases) relies on three factors:
- Genetic predisposition
- Environmental trigger (in the case of celiac disease, that trigger is gluten)
- A leaky gut and/or gut dysbiosis
All three of these factors work together to develop autoimmune disease. In terms of celiac disease, the genetic predisposition is at least partially understood: 90% of celiacs have one of two variants of the HLA gene (either DQ8 or DQ2). What you need to know about the HLA gene is that it (or more specifically the protein in encodes) is involved in antigen presentation to the adaptive immune system, and defects in this process seem to be permissive for autoantibody formation. But, approximately 30% of us have one of these gene variants and only 1% of us develop celiac disease (it should be noted that these gene variants are linked to other autoimmune diseases as well as non-celiac gluten sensitivity, so it’s not like the other 29% of us are getting off easy). The environmental trigger for celiac disease is dietary gluten (or more specifically the protein fraction of gluten, called gliadin). So, what’s the wild card? A leaky gut. And the development of a leaky gut may be what determines the age of disease onset, which is highly variable. Chance (or maybe previous infections or maybe gut dysbiosis, i.e., the wrong types of bacteria growing in the wrong numbers in the wrong part of the gut) may be what determines whether a person develops celiac disease versus another autoimmune disease versus other health problems linked to gluten.
A leaky gut can be caused by a wide variety of factors, including: diets rich in some types of lectin (like gluten) and saponins (especially glycoalkaloids), stress, and gut dysbiosis (especially bacterial overgrowths). Gut dysbiosis itself can be caused by diets rich in processed foods, refined carbohydrates, some types of lectins (especially prolamins like gluten and agglutinins like wheat germ agglutinin) and saponins (especially glycoalkaloids), by some medications (such as PPIs and antibiotics) and by stress. A leaky gut and gut dysbiosis go hand in hand and it is not known which comes first.
So, what is the link between breastfeeding and a leaky gut? The link is really to gut dysbiosis (or lack thereof). Studies show that breastfeeding is important for the establishment and growth of normal gut microorganisms. In particular, breastmilk contains probiotics (from strains shown to be deficient in the guts of those with celiac disease) and for the duration of breastfeeding, the guts of babies are being constantly inoculated with these beneficial bacteria. It is becoming increasingly recognized that the healthy diversity and relative amounts of gut microorganisms are intricately linked your health. So, it’s no surprise that whatever factors contribute to healthy gut microorganisms in babies will protect them from disease.
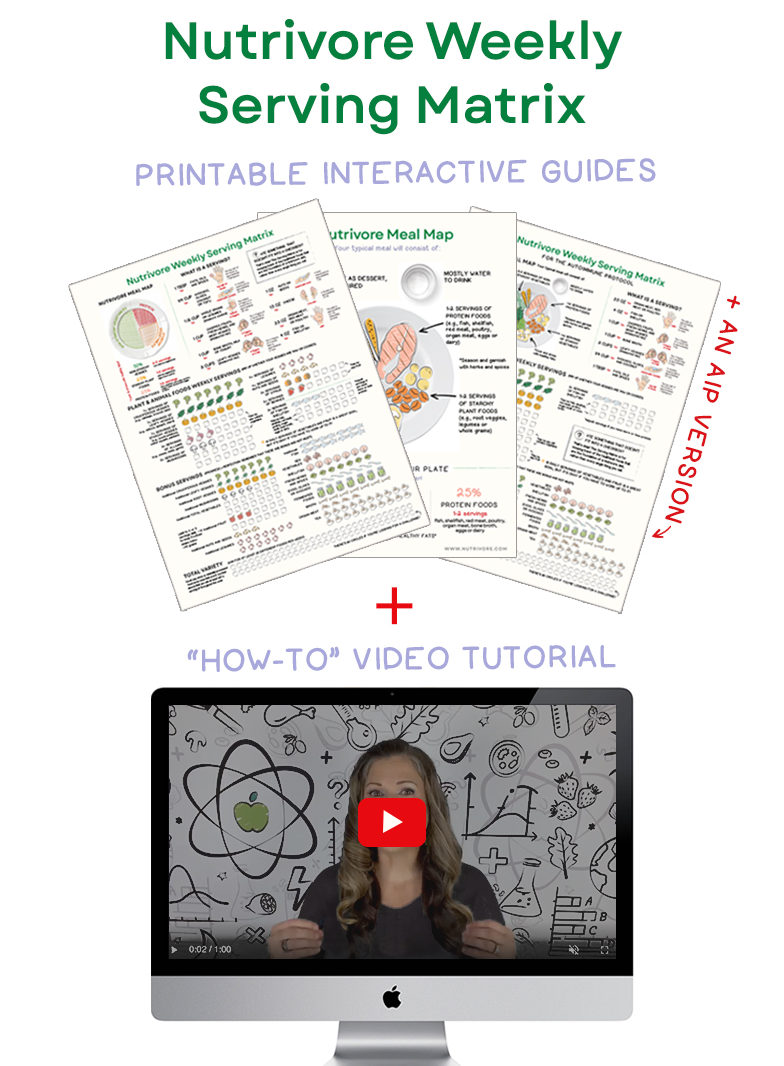
Nutrivore Weekly Serving Matrix
An easy-to-use and flexible weekly checklist
to help you maximize nutrient-density.
The Weekly Serving Matrix is very helpful! I’ve been eating along these lines but this really helps me know where to focus vs. which foods serve a more secondary role. It’s super helpful and has taken a lot of worry out of my meal planning. Thanks!
Jan
So, let’s get back to the study. It has one very big limitation relevant to this discussion. It cannot separate whether the exact age of gluten introduction in babies who were breastfed longer has any effect on celiac risk. This study definitely shows that breastfeeding longer decreases celiac risk. But, the idea that this is because breastfeeding occurred during and beyond gluten introduction is speculative. It certainly makes sense given other research on the link between gut microorganisms and disease risk that a healthy gut is important in celiac disease risk and that breastfeeding longer improves the health of the gut microorganisms. But, this study just can’t tell you whether introduction of gluten early (and before weaning) is important. If the reason breastfeeding is protective is because of its probiotic effects (it’s nutrient value would be another good reason), then it could be that it doesn’t matter when gluten is introduced (if ever) as long as the gut is healthy when you do.
From birth through adulthood, diet has a profound effect on the composition and relative quantities of your gut microorganisms (I explain this is detail in my book). And healthy gut microorganisms have a profound protective effect on the integrity of the gut barrier and are essential modulators of the immune system (yes, I explain this in detail in my book as well). The optimal diet in terms of gut and gut microorganism health seems to be a hunter/gatherer/gardener type diet, rich in plants (but not grains or legumes and nothing processed or refined) and wild or pastured meat and/or wild-caught fish (no surprise to us in the Paleo community). What is healthy nutrient-dense food for you just happens to be healthy food for your gut microorganisms. And, while this is an oversimplification, if you feed your gut bacteria good food, they are healthy, and therefore you are healthy.
So, getting back to the question that is flooding my inbox: does this paper mean you should feed your Paleo babies a little gluten now so that they will develop immune tolerance? This study does not allow us to conclusively say yes or no. Certainly, this study does not prove its assertion that introducing small amounts of gluten into the diet very early and prior to weaning will increase immune tolerance and therefore protect your baby against ever developing celiac disease (although you can add this study to the bounty of scientific studies showing that breastfeeding is beneficial for your baby). It should also be noted that the health of the mother greatly affects the probiotic and nutrient content of the breastmilk. It is unknown whether breastmilk is still protective in the context of obese mothers or mothers with chronic health conditions.
I believe that the best thing that you can do for your baby’s long term health (besides love and cherish them) is feed them nutrient-dense, nourishing foods that will help them have healthy guts and healthy gut microorganisms. I do not believe that gluten consumption promotes a healthy gut or healthy gut microorganisms (and the science backs me up on this one—I reference a few hundred studies on this topic in my book). But, I also don’t know whether, if you wait “too long” to introduce gluten, if some magical window of opportunity to develop immune tolerance against gluten will be missed (or how much gluten you would need to keep in the diet to maintain immune tolerance). I also don’t know whether having immune tolerance against gluten is even a good thing in terms of overall long term health. Science does not yet provide a clear answer. So, with all of these ideas in mind, the decision will have to be yours and will have to be based on your own risk assessment.
Bengmark S. Gut microbiota, immune development and function. Pharmacol Res. 2013 Mar;69(1):87-113. doi: 10.1016/j.phrs.2012.09.002. Epub 2012 Sep 16.
Fasano A. Leaky gut and autoimmune diseases. Clin Rev Allergy Immunol. 2012 Feb;42(1):71-8. doi: 10.1007/s12016-011-8291-x.
Groschwitz KR and Hogan SP. Intestinal barrier function: molecular regulation and disease pathogenesis. J Allergy Clin Immunol. 2009 Jul;124(1):3-20; quiz 21-2. doi: 10.1016/j.jaci.2009.05.038.
Hascoët JM et al. Effect of formula composition on the development of infant gut microbiota. J Pediatr Gastroenterol Nutr. 2011 Jun;52(6):756-62. doi: 10.1097/MPG.0b013e3182105850.
Ivarsson A et al Epidemic of coeliac disease in Swedish children. Acta Paediatr. 2000 Feb;89(2):165-71.
Ivarsson A, Prevalence of Childhood Celiac Disease and Changes in Infant Feeding. Pediatrics. 2013 Feb 18. [Epub ahead of print] http://pediatrics.aappublications.org/content/early/2013/02/13/peds.2012-1015.long