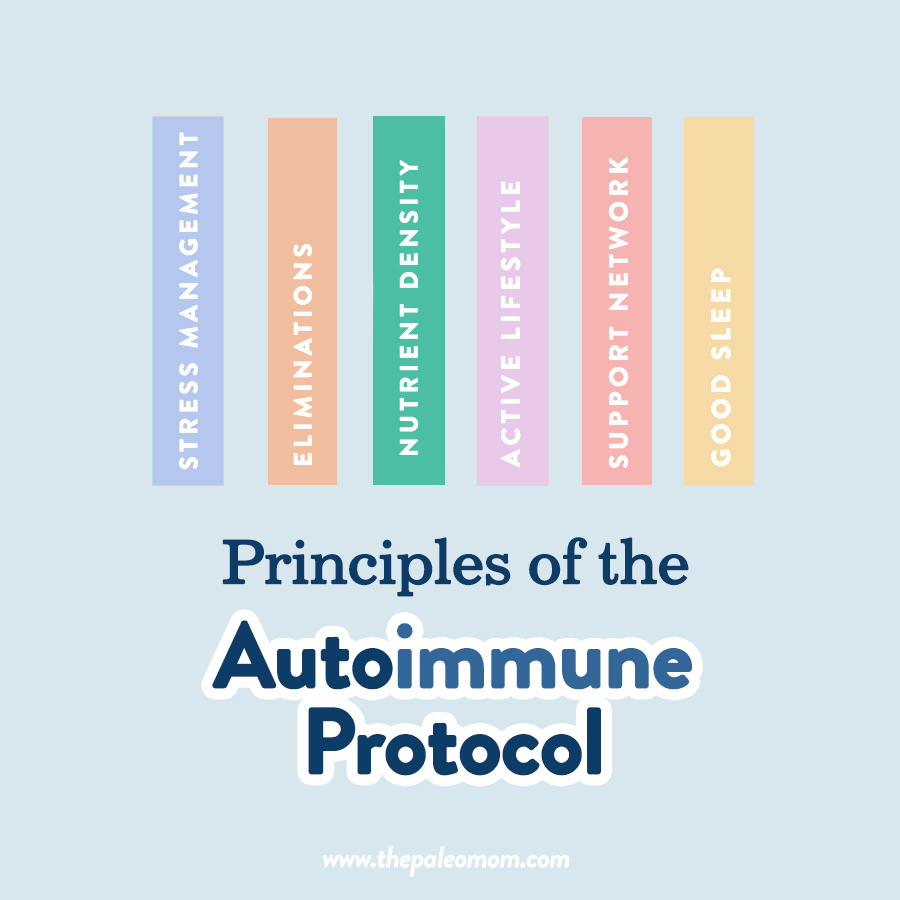
 The Autoimmune Protocol, or AIP, is a science-based diet and lifestyle intervention for autoimmune disease and other chronic illnesses driven by immune dysregulation. You can think of it as a collection of best practices related to diet and lifestyle, not to the exclusion of additional treatments or interventions, that can be individualized to address specific circumstances and goals, framed in the context of a person whose health challenges imply a lower resilience to suboptimal choices.
The Autoimmune Protocol, or AIP, is a science-based diet and lifestyle intervention for autoimmune disease and other chronic illnesses driven by immune dysregulation. You can think of it as a collection of best practices related to diet and lifestyle, not to the exclusion of additional treatments or interventions, that can be individualized to address specific circumstances and goals, framed in the context of a person whose health challenges imply a lower resilience to suboptimal choices.
As I discussed in My Personal Journey with the Autoimmune Protocol, my work both popularized the AIP and helped transform it from an obscure fad to a valid dietary strategy to support people with autoimmune disease. My core belief in the importance of representing scientific evidence in an unbiased and nuanced way brought scientific validity to the AIP. I wrote The Paleo Approach (which remains the definitive guide to the AIP), based on collective insight gleaned from over 1200 scientific studies. Since its publication in 2014, hundreds of thousands of people have successfully used the AIP to manage and mitigate their autoimmune diseases.
But the most exciting thing that has been happening is the increase in medical studies that have formally evaluated the benefits of the AIP on serious clinical health conditions. These studies are building the type of concrete proof that has the capacity to transition the AIP from a complementary approach to first-line course of treatment, advancing the AIP to the mainstream. It is the culmination of nearly a decade of my work in conjunction with the AIP community at large, and something for which I am immensely proud.
Autoimmune Protocol Clinical Trials
Let’s review the clinically-validated benefits of the Autoimmune Protocol (so far)!
Konijeti GG, Kim N, Lewis JD, Groven S, Chandrasekaran A, Grandhe S, Diamant C, Singh E, Oliveira G, Wang X, Molparia B, Torkamani A. Efficacy of the Autoimmune Protocol Diet for Inflammatory Bowel Disease. Inflamm Bowel Dis. 2017 Nov;23(11):2054-2060. doi: 10.1097/MIB.0000000000001221.
This 2017 study evaluated the efficacy of the Autoimmune Protocol for management of inflammatory bowel disease.
Fifteen patients with active inflammatory bowel disease—9 participants with Crohn’s disease and 6 with ulcerative colitis, and 47% of which were on biologics—were placed on the Autoimmune Protocol by transitioning gradually over 6 weeks (using the SAD to AIP in 6 program), followed by 5-weeks maintaining the strict elimination phase of the AIP (see The 3 Phases of the Autoimmune Protocol). Patients were closely monitored and given access to health coaching. They were also given two books The Paleo Approach by Dr. Sarah Ballantyne, PhD and The Autoimmune Wellness Handbook by Mickey Trescott, NTP and Angie Alt, NTC, CHC, as resources for following the protocol. This study evaluated disease markers for IBD including the Harvey-Bradshaw Index (HBI) for those with Crohn’s disease, and Mayo Score for those with Ulcerative Colitis—both of which are pain and symptom scores—as well as endoscopy improvements and laboratory markers.
For patients with ulcerative colitis, the Mayo scores at 0, 6 and 11 weeks were significantly improved from 5.8 to 1.2 to 1.0. And for patients with Crohn’s disease, the mean HBI was improved from 7 to 3.6 and finally to 3.4. The mean fecal calprotectin (a serology marker of inflammation) improved from 471 to 112 at week 11. Endoscopy improvements were also noted in 6 of the 7 participants who completed a follow-up endoscopy at week 11.
Clinical remission was achieved by week 6 in 11 of the 15 (73%) study participants, and all 11 maintained clinical remission throughout the study’s maintenance phase. The authors did not expect to achieve clinical remission so early into the study, and remarked that 6-week remission “rivals that of most drug therapies for IBD.” The authors note that dietary therapy and modifications can be used as an adjunct to current IBD therapies and medical practices in those even with moderate-to-severe disease.
Some limitations of this study include the lack of detailed follow-up with regard to the non-dietary aspects on patient improvement, such as: close follow-up with practitioners, stress, sleep, physical activity, social support etc. Treatment for IBD relies heavily on reducing overall inflammation and isolating the effect of all factors independently was not considered. Nutrient repletion was also utilized for participants with deficiencies in vitamin D and iron, which may have impacted the results for those few patients.
Chandrasekaran A, Molparia B, Akhtar E, Wang X, Lewis JD, Chang JT, Oliveira G, Torkamani A, Konijeti GG. The Autoimmune Protocol Diet Modifies Intestinal RNA Expression in Inflammatory Bowel Disease. Crohns Colitis 360. 2019 Oct;1(3):otz016. doi: 10.1093/crocol/otz016.
This 2019 study evaluated the effect of the AIP diet on gene expression for those with inflammatory bowel disease (IBD), by extending the data analysis from the above-described 2017 trial where 73% of IBD patients achieved clinical remission by 6 weeks on the Autoimmune Protocol.
This data extension included examining changes in mucosal RNA expression from baseline to the end of the study. In this previous cohort, 5 participants had biopsies collected for analysis at both time points (at the baseline and end of diet implementation). There was only 1 patient with Crohn’s disease, therefore the analysis was limited to the 4 patients with ulcerative colitis (UC) only.
The results of the study illustrated that there were 324 significant differentially regulated genes, of which 167 were down regulated—that is they were “turned down”, and 157 genes were up regulated—that is they were “turned up”. The study found beneficial modulation of functional pathways involved in inflammation, DNA repair, metabolic processes, and cellular proliferation.
Save 70% Off the AIP Lecture Series!
Learn everything you need to know about the Autoimmune Protocol to regain your health!
I am loving this AIP course and all the information I am receiving. The amount of work you have put into this is amazing and greatly, GREATLY, appreciated. Thank you so much. Taking this course gives me the knowledge I need to understand why my body is doing what it is doing and reinforces my determination to continue along this dietary path to heal it. Invaluable!
Carmen Maier
In particular, the gene expression changes observed are associated with downregulation of inflammatory T-cell-mediated responses, which drive tissue injury in autoimmune disease, so turning down these genes is a great thing! And, there was also concurrent upregulation of regulatory T-cell responses and function, the insufficiency of which is a hallmark of autoimmune disease. Regulatory T-cells are crucial for regulating the adaptive immune system—these cells suppress the activity of immune and inflammatory cells to shut down T-cell-mediated immunity toward the end of an immune reaction. So, turning up these genes is also a great thing! Other functional pathways that were modulated indicate increased gut mucosal healing (yay!), including protein synthesis, fatty acid synthesis, and DNA repair.
The authors conclude: “Results from this RNA substudy would suggest dietary elimination, along with emphasis on a nutrient-dense diet, has the potential to positively modify inflammation and reduce symptoms in UC.”
Chandrasekaran A, Groven S, Lewis JD, Levy SS, Diamant C, Singh E, Konijeti GG. An Autoimmune Protocol Diet Improves Patient-Reported Quality of Life in Inflammatory Bowel Disease. Crohns Colitis 360. 2019 Oct;1(3):otz019. doi: 10.1093/crocol/otz019.
This 2019 study is another data extension from the same IBD cohort in which the improvement of quality of life (QOL) scores were evaluated for the participants with irritable bowel disease (IBD).
This study also evaluated disease markers for IBD including the Harvey-Bradshaw Index (HBI) for those with Crohn’s disease, and Mayo Score for those with Ulcerative Colitis—both of which are pain and symptom scores—as well as endoscopy improvements and laboratory markers. The participants also completed the Short Inflammatory Bowel Disease Questionnaire (SIBDQ) at baseline weeks 3, 6, 9 and 11, which is the most commonly used tool for evaluating the quality of life in patients with IBD. The SIBDQ uses total scores ranging from 10-70 and ≥50 being a good quality of life. Upon completion of the 11-week trial, patients mean Mayo score improved from 5.8 to 1.0 and the HBI improved from 7 to 3.4. Laboratory inflammation markers showed marked improvements, and for those with follow-up endoscopies, there were observed improvements also.
While the SIBDQ survey completion percentage reduced throughout the study, the final analysis revealed that mean scores improved from 46.5 at baseline to 61.5 at week 11. Some limitations of this study were dietary compliance, survey responsiveness, and the effect of health coach interactions on QOL independent from actual clinical improvement. Additionally, the cohort was a relatively small sample size at 15 people, and a control group was not incorporated. This study was intended to act as a pilot study for the potential efficacy of AIP on people with IBD.
The study acknowledges that the AIP has the potential to significantly improve quality of life measurements in patients with IBD, and that larger randomized controlled trials are warranted. I agree!
Abbott RD, Sadowski A, Alt AG. Efficacy of the Autoimmune Protocol Diet as Part of a Multi-disciplinary, Supported Lifestyle Intervention for Hashimoto’s Thyroiditis. Cureus. 2019 Apr 27;11(4):e4556. doi: 10.7759/cureus.4556.
This 2019 study studied 16 middle-aged women diagnosed with Hashimoto’s thyroiditis, and the impact of the Autoimmune Protocol on their symptoms, quality of life survey and serological testing. Currently, there are few, if any, efficacious treatments for Hashimoto’s thyroiditis outside of thyroid hormone replacement. Similar to the IBD study design, study participants were placed on the Autoimmune Protocol by transitioning gradually over 6 weeks (using the SAD to AIP in 6 program), followed 4-week maintaining the elimination phase of the AIP, and facilitated by health coaches.
Patients experienced a statistically significant improvement in health-related quality of life scores as measured by the 36-Item Short Form Health Survey and Cleveland Clinic Center for Functional Medicine’s Medical Symptoms Questionnaire (MSQ). In fact, the clinical symptom burden, as measured by the MSQ, decreased from an average of 92 at the beginning of the study to 29 after the 10 weeks. There were no statistically significant changes in thyroid function including TSH, free and total T3, and free and total T4, and thyroid antibodies. Inflammation however was significantly decreased by 29%, as measured by C-reactive protein (a measurement of systemic inflammation)!
The study concluded that a diet and lifestyle program facilitated by a multidisciplinary team could significantly improve the health related quality of life and symptom burden of women with Hashimoto’s thyroiditis, and could reduce systemic inflammation and even modulate the immune system (as evidenced by changes in white blood cell counts in the serology of participants).
The authors highlight that “[t]he role of the physician, health coaches, and NTPs, as well as the participants’ communal group environment, cannot be understated and appears to be the primary mediating elements behind the high rate of adherence.”
There are some other AIP studies in the works and I’m excited to share them once they complete the peer-review process and are published!
 If you’re looking to deepen your knowledge on the AIP, the AIP Lecture Series is without a doubt my most effective and comprehensive resource for learning about the Autoimmune Protocol, thanks to my careful layering of information with a multimedia approach plus the interactive nature of this online course. I teach every aspect of this course and provide individual support within a private Facebook group, where I connect with every student and answer ever question posed during the session. Of the (many) benefits of this type of intensive educational experience is the opportunity to:
If you’re looking to deepen your knowledge on the AIP, the AIP Lecture Series is without a doubt my most effective and comprehensive resource for learning about the Autoimmune Protocol, thanks to my careful layering of information with a multimedia approach plus the interactive nature of this online course. I teach every aspect of this course and provide individual support within a private Facebook group, where I connect with every student and answer ever question posed during the session. Of the (many) benefits of this type of intensive educational experience is the opportunity to:
- emphasize the comprehensive and holistic nature of the Autoimmune Protocol;
- maintain a positive focus on what to eat (rather than perseverate on what to eliminate);
- dive into the nitty gritty why’s behind, and scientific evidence for, each facet of the protocol;
- discuss how to troubleshoot and individualize the AIP; and
- address mindset, balance, and sustainability when it comes to utilizing the AIP as a complementary approach to healing.
Over the last 4 years of running my course, I have learned that this deep understanding and learning about the AIP is not only interesting and helpful for students, but it is a keystone to the true empowerment and confidence that transforms autoimmune disease sufferers into disease warriors!!
However, my virtual classroom is far from the only way to learn the ins and outs of the AIP! You can also do so through self-education (reading my books [especially The Paleo Approach and The Autoimmune Protocol] and/or the vast collection of freely available and up-to-date articles on the AIP on my site, for example), 1-on-1 coaching (like working with an AIP Certified Coach), or group coaching (like SAD to AIP in Six).
Additional Dietary Elimination Protocol Studies – The Wahls Protocol
 The Wahls Protocol is the most similar approach to the Autoimmune Protocol out there, and because Dr. Wahls has led the way with her rigorously-designed studies, her protocol is a reliable additional proof of concept that a nutrient-dense diet and healthy lifestyle can improve autoimmune disease.
The Wahls Protocol is the most similar approach to the Autoimmune Protocol out there, and because Dr. Wahls has led the way with her rigorously-designed studies, her protocol is a reliable additional proof of concept that a nutrient-dense diet and healthy lifestyle can improve autoimmune disease.
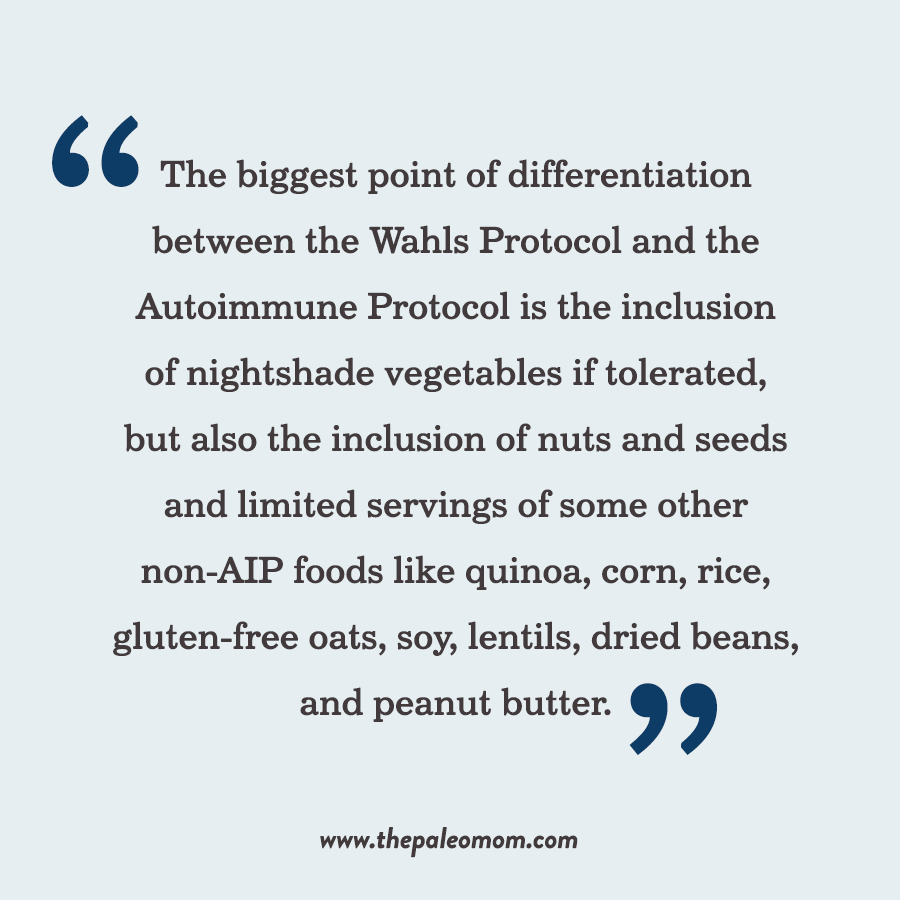
The Wahls Protocol diet is mainly focused on eating 9 cups of vegetables per day (3 cups each of green veggies, colorful veggies, and sulfur-rich veggies), animal and fish protein while encouraging fish oil consumption, nutritional yeast consumption, kelp and algae consumption, allowed non-dairy milk substitutes, limited non-gluten containing grains, and completely eliminated dairy, gluten, and eggs. The biggest point of differentiation between the Wahls Protocol and the Autoimmune Protocol is the inclusion of nightshade vegetables if tolerated, but also the inclusion of nuts and seeds and limited servings of some other non-AIP foods like quinoa, corn, rice, gluten-free oats, soy, lentils, dried beans, and peanut butter. If you’re familiar with my work, you’ll recognize most of those as early AIP reintroductions. So, while the Wahls Protocol leaves room for self-experimentation and has added the Wahls Paleo and Wahls Paleo Plus levels that have more eliminations, the AIP take the approach of eliminating all of the possible culprits driving inflammation and immune overactivation and then methodically testing individual tolerance through a reintroduction phase. Both diets heavily promote nutrient-density including eating tons of veggies (the AIP does not put a firm serving amount on any food but does suggest aiming for a minimum of 8 to 10 servings per day), organ meat and seafood. Exercise and meditation are also endorsed on the Wahls Protocol, although the lifestyle focus on the Autoimmune Protocol is more rigorous.
With that said, there have been some amazing studies including the Wahls Protocol in recent years and the following section summarizes them as an important inclusion to the healing power of food, and the similar principles of AIP. See also The First Clinical Trial Using a Paleo Diet for Autoimmune Disease.
Wahls TL, Titcomb TJ, Bisht B, Eyck PT, Rubenstein LM, Carr LJ, Darling WG, Hoth KF, Kamholz J, Snetselaar LG. Impact of the Swank and Wahls elimination dietary interventions on fatigue and quality of life in relapsing-remitting multiple sclerosis: The WAVES randomized parallel-arm clinical trial. Mult Scler J Exp Transl Clin. 2021 Jul 31;7(3):20552173211035399. doi: 10.1177/20552173211035399.
In this brand-new 2021 study, 77 participants were studied over a 12-week interval and 72 participants were continued onto a 24 week study period to determine the effect of dietary modification on the impact of relapsing-remitting multiple sclerosis (RRMS). Trial participants were randomized into two different dietary protocol groups: the Swank diet or the Wahls Protocol. The Swank diet is a low-saturated fat diet, whereas the Wahls Protocol centers around the Paleolithic elimination diet focusing on high nutrient density and elimination of specific dietary antigens such as gluten, casein and lectins. The Wahls Protocol was randomized with 39 participants completing the primary endpoint, and the Swank diet had a cohort of 38 complete the 12-week duration. The primary evaluation points were to measure the change in perceived fatigue as determined by the Fatigue Severity Scale (FSS). Secondary results evaluated the Modified Fatigue Impact Scale (MFIS), the mental and physical quality of life (MSQoL-54 score) and the 6-minute walking test (6MWT).
The results showed significant mean reductions in FSS from baseline for both diets with the Wahls Protocol outperforming the Swank diet at the final 24-week endpoint. Additionally, both groups saw a reduction in MFIS with the Wahls Protocol group significantly outperforming the Swank diet at all time intervals. The MSQoL-54 measurements revealed the Wahls Protocol participants again achieving clinical significance through both time points and achieving significantly more improvement when compared to scores in the Swank diet group. Additionally, the 6MWT groups in the Wahls Protocol group severely outperformed the Swank diet participants and achieved the mark of clinical significance at the 24-week mark.
The findings of this study illustrate that both diets achieved significant reductions in fatigue and QoL for participants, however the Wahls Protocol was superior in all metrics at the final 24-week endpoint. “In addition, two trials show that dietary modification improves the mass and diversity of the gut microbiota in people with MS. Evidence suggests that people with MS have reduced mass and diversity of their gut microbiota compared to healthy controls, which likely promotes inflammation.”
Chenard CA, Rubenstein LM, Snetselaar LG, Wahls TL. Nutrient Composition Comparison between a Modified Paleolithic Diet for Multiple Sclerosis and the Recommended Healthy U.S.-Style Eating Pattern. Nutrients. 2019 Mar 1;11(3):537. doi: 10.3390/nu11030537.
The goal of this 2019 paper was to assess the nutritional content in of the Wahls Protocol in relation to the dietary reference intakes (DRI) of the Dietary Guidelines for Americans (DGA) Healthy US-style Eating Pattern (HEP). Different dietary protocols are often utilized in people with multiple sclerosis (MS), but due to the lacking scientific evidence there is limited guidance for patients on how to improve outcomes outside of medical treatment. The concern is that the Wahls protocol eliminates large food groups, and therefore has the potential to be deficient in nutrients. The analysis also took into account the nutrient composition and inclusion of any dietary supplements recommended on the Wahls protocol. Several iterations of the Walhs protocol were modeled with varying vegetable and fruit consumption amounts, and the subsequent nutrient sufficiency of 17 vitamins and minerals was evaluated.
The study found that the Wahls Protocol was of similar sufficiency as the HEP in all modeled cases, including variations in the serving numbers of fruits and vegetables. While the protocol alone demonstrated a shortfall of vitamin D and magnesium, the supplementation recommended alongside the diet protocol corrected the deficiencies in all cases modeled. However, supplementation did not correct the other shortfall nutrients such as iron and calcium, linoleic acid, choline, dietary fiber, and potassium. Some nutrients that were exceeded on the Wahls protocol include sodium, vitamin K, and saturated fats. Additionally, the high amount of nutritional yeast that is included in the diet results in high levels of B vitamins. Dr Wahls hypothesizes that some of the higher vitamin concentrations are helpful for remyelination (that is the growing of new myelin sheaths around the axons in the central nervous system), thus helping to ‘heal’ the body from the effects of multiple sclerosis. The study culminated in guidance for practitioners to closely monitor in their MS clients who are on the dietary protocol, especially with regard to lipids, vitamin D, bone, vitamin K, and iron status. The study was not able to determine levels of polyphenols, iodine, sulphur compounds, and biotin because data was not available.
Titcomb TJ, Bisht B, Moore DD 3rd, Chhonker YS, Murry DJ, Snetselaar LG, Wahls TL. Eating Pattern and Nutritional Risks among People with Multiple Sclerosis Following a Modified Paleolithic Diet. Nutrients. 2020 Jun 20;12(6):1844. doi: 10.3390/nu12061844.
Similar to the previous study, the goal of this 2020 paper was to determine the nutrient sufficiency of the Wahls Protocol diet on 19 participants, through means of dietary recall (that is, the participants were tasked with remembering their meals for the study periods), and the diets were analyzed with a nutrition software. Three 24-hour non-consecutive dietary recall entries were taken from each participant and modeled for analysis. Blood markers were collected from the participants both at the baseline and completion of the study period to determine any biomarker changes.
The study concluded that the micronutrients intake from food was sufficient in all clients, except for vitamin D, choline, and calcium. One participant exceeded the upper limit for zinc, one exceeded the limit for vitamin A, and 7 participants (or 37%) exceeded the chronic disease risk reduction (CDRR) limit for sodium. When vitamin intake from additional supplements was included, several individuals exceeded upper limits for magnesium, zinc, sodium, and vitamins A, D, C, B6, and niacin. “Serum values of vitamins D, B12, K1, K2, and folate significantly increased compared to respective baseline values, while homocysteine and magnesium values were significantly lower at 12 months. Calcium and vitamin A serum levels did not change.” The study concluded that the Wahls Protocol, otherwise known as a modified Paleolithic diet, is associated with minimal nutritional risks. However, the use of supplements alongside the dietary modification could result in exceeding upper limits of nutrients, and may be of concern.
Lee JE, Titcomb TJ, Bisht B, Rubenstein LM, Louison R, Wahls TL. A Modified MCT-Based Ketogenic Diet Increases Plasma β-Hydroxybutyrate but Has Less Effect on Fatigue and Quality of Life in People with Multiple Sclerosis Compared to a Modified Paleolithic Diet: A Waitlist-Controlled, Randomized Pilot Study. J Am Coll Nutr. 2021 Jan;40(1):13-25. doi: 10.1080/07315724.2020.1734988.
In this randomized controlled study, 15 participants with multiple sclerosis (MS) were randomized to 3 groups to determine the effect on fatigue and quality of life:
- modified Paleolithic diet (Paleo group: 6 participants)
- medium-chain triglyceride (MCT)-based ketogenic diet that included coconut as a fat source (Keto group: 5 participants)
- usual diet (Control group: 4 participants)
“Participants had blood drawn every 4 weeks to monitor nutritional ketosis. Participants completed 4-day weighed food records, measures of disability, fatigue, quality of life (QoL), cognitive function, and physical function at baseline and 12-weeks.”
The macronutrient intake and measured blood levels of β-hydroxybutyrate indicated that the Keto group had achieved nutritional ketosis by week 12. Macronutrient intake and blood levels indicated that neither the Paleo group nor the control were in nutritional ketosis at week 12. “The Paleo group had significant within group reductions in fatigue scores and maintained cognitive function scores compared to the Control group. The Keto group had significant reductions in fasting glucose and insulin compared to baseline values; however, no clinical outcomes significantly changed.” The study concluded that while the Keto group was able to obtain nutritional ketosis, it was not associated with significant clinical improvement, whereas the Paleo group experienced significant clinical improvement when compared with both the Keto and the Control groups. The study concludes that larger randomized controlled trials are required to determine the efficacy and safety of the modified Paleolithic diet for patients with MS.
It’s worth noting that I’ve written about the limitations and problems with a ketogenic diet before, so I’m in no way surprised that it was ineffective and comparable to the control group in this study. Read more in How Ketogenic Diet Wreaks Havoc on Your Gut, Adverse Reactions to Ketogenic Diets: Caution Advised, The Case for More Carbs: Insulin’s NonMetabolic Roles in the Human Body and TPV Podcast, Episode 140: The Danger of Ketogenic Diets.
Irish AK, Erickson CM, Wahls TL, Snetselaar LG, Darling WG. Randomized control trial evaluation of a modified Paleolithic dietary intervention in the treatment of relapsing-remitting multiple sclerosis: a pilot study. Degener Neurol Neuromuscul Dis. 2017 Jan 4;7:1-18. doi: 10.2147/DNND.S116949.
In this 2017 study, 17 patients were evaluated to determine the dietary effect of the modified Paleolithic dietary intervention (MPDI), for the treatment of fatigue and other clinical symptoms on relapsing-remitting multiple sclerosis (RRMS). The control group was 8 participants including one male, where the intervention group was 9 participants including one male. Study participants in the control were given training on completing food diaries, where the intervention group was trained on filling out a more detailed food log, to properly capture the detail required in the intervention group. The study length was 3-months and measurements were taken at baseline and at 3 months.
“Significant improvements were seen in Fatigue Severity Scale score and also in Multiple Sclerosis Quality of Life-54 and time to complete (dominant hand) 9-Hole Peg Test from baseline in MPDI subjects compared to controls. Increased vitamin K serum levels were also observed in MPDI subjects postprotocol compared to controls.”
The study concluded that modified Paleolithic diet may be useful in the treatment and management of MS, by reducing fatigue scores, increasing quality of life (both mental and physical), increasing exercise capacity, and improving hand and leg function. The results also showed that intervention participants had higher vitamin K serum levels than the control group, which may also reduce inflammation.
In Summary
The benefits of the AIP, and similar dietary approaches such as the Wahls Protocol, are gaining validation both in practice, and in the scientific literature. Those of us with anecdotal experience in the success of AIP for supporting our health goals are relieved, excited and understandably emotional about the validation offered by the scientific community.
I continue to anticipate further randomized controlled studies to further validate the impact of the AIP (there are a couple in the works!), and I look forward to all of the autoimmune disease warriors who will be helped in the future when the AIP becomes standard practice and a recommended adjunct therapy to the current medical interventions and treatment protocols.
Acknowledgements
I would be remiss to not offer my support and a shout-out to Mickey Trescott and Angie Alt of Autoimmune Wellness, whose organization works to provide funding and support of studies relating to the Autoimmune Protocol. Without their passion for AIP and the scientific method, many of these works would not be published today. Also, I must comment on my immense respect to Dr. Terry Wahls and her tireless mission towards providing infallible science to support her fellow MS disease warriors.