This time of year, health advice abounds. We’re barraged with directions to change many different aspects of our lifestyles: “Eat this! Drink that! Detox from this! Stop this! Start that!” For me, turning to the scientific literature is a respite from the madness, and the main goal of this website and my books is to disseminate this information to people without them having to read the original papers themselves. Let’s cut through the hype, dogma and 30-day challenges and talk about a critical input to health that we all generally suck at: balance.
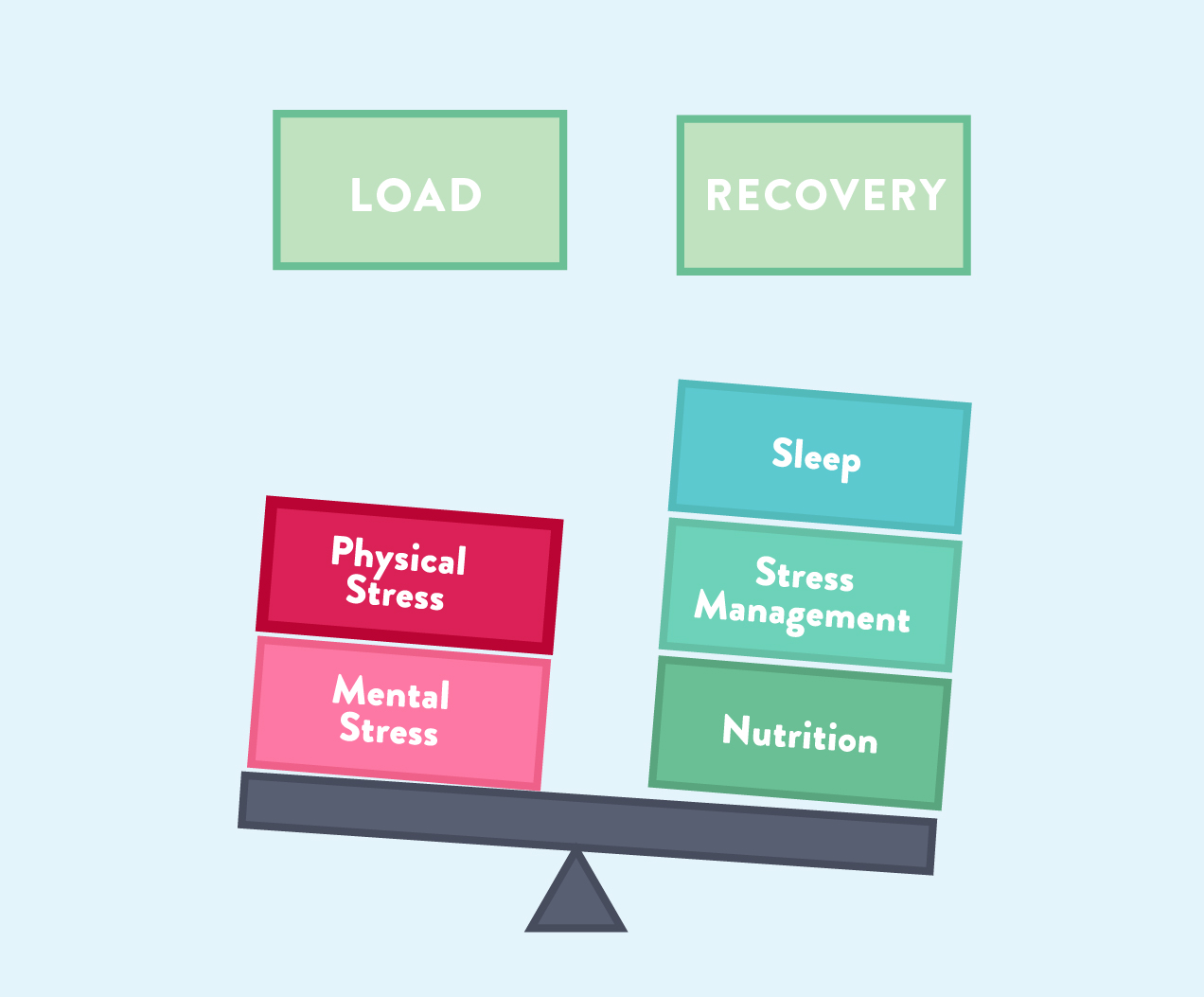 When most of us hear the word balance, we think about balancing work and play (the elusive work-life balance that was my resolution last year!). But the concept studied in medical research refers to balancing load (that includes physical load and mental load) with recovery. Load includes both physical and mental load, the stressors, both good and bad, of our every day life. For example, physical load includes the stress of sitting for a prolonged period of time but also the stress of a demanding workout; mental load includes psychological stressors like deadlines, toxic relationships, and parenting. And while recovery chiefly refers to sleep, stress management and nutrition are also criticial.
When most of us hear the word balance, we think about balancing work and play (the elusive work-life balance that was my resolution last year!). But the concept studied in medical research refers to balancing load (that includes physical load and mental load) with recovery. Load includes both physical and mental load, the stressors, both good and bad, of our every day life. For example, physical load includes the stress of sitting for a prolonged period of time but also the stress of a demanding workout; mental load includes psychological stressors like deadlines, toxic relationships, and parenting. And while recovery chiefly refers to sleep, stress management and nutrition are also criticial.
As I wrote in Go to Bed, the demands of the modern world have left us totally unbalanced: for most of us, our load is MUCH greater than our recovery. We want to fulfill all of our perceived obligations and push ourselves at school, our jobs, and the gym, and often do so until the brink of exhaustion (or end up with adrenal fatigue and/or associated conditions, as I’ve discussed in my new post series, Demystifying Adrenal Fatigue), but it’s also super important that we get enough activity and not spend too much time on our bums. The bottom line is that these lifestyle factors are incredibly important for our health, but knowing how to balance rest and activity can be a daunting task. So, in this post, I detail the factors that contribute to this complex equation and how we might do a better job of balancing our load and recovery in our own lives. There are three main factors: physical activity (aka physical load), sleep (aka recovery), and stress (aka mental load).
Save 80% Off the Foundations of Health
Expand your health knowledge on a wide range of topics relevant to you, from how to evaluate scientific studies, to therapeutic diet and lifestyle, to leaky gut and gut microbiome health, to sustainable weight loss, and much more!!!

Exercise: The Type(s) and Frequency of Physical Load Matters
When it comes to load, we might first think of physical load (the modern equivalent of that being exercise or movement), which is definitely one of the pillars of good health. Getting regular moderate exercise decreases risks of cardiovascular disease, type 2 diabetes, insulin resistance, anxiety, cognitive decline, depression, and some cancers. In fact, the World Health Organization has identified the lack of physical activity as the fourth leading risk factor for mortality, being responsible for an estimated 3.2 million deaths each year globally!
Many of us think we can cancel out an otherwise sedentary lifestyle (sitting at our desk job, commuting in the car, watching TV, and spending way too much time on Facebook) by going to the gym a few times per week and breaking a sweat. In fact, it’s common to think of exercise as a sort of “payment” to put in so we can veg out on the couch afterward (eating whatever food we’ve “earned”) and not feel guilty about it. But, a growing body of research is showing that it’s not just the absence of exercise that makes sitting an issue. Sitting itself, especially for long periods, is actually hazardous for our bodies. And unfortunately, you can’t make up for sitting all day by giving 110% at CrossFit for an hour in the evening. When it comes to this aspect of load, we do need to take on a certain amount of physical activity throughout the day – but that may not be as difficult as we think.
A growing body of scientific literature shows that moving around for just 2 minutes out of every 20 minutes that you would be otherwise completely sedentary has tremendous health benefits. This means that repeatedly setting a 20 minute timer and then getting up and walking around for 2 minute throughout your work day can completely negate the health detriment of prolonged sitting. Interestingly, one paper published this May showed that simply standing for 2 minutes didn’t work, and that moving (a slow walk) is key (see also The Benefits of Gentle Movement).
There’s more to the story, too. Gentle movement, when it also involves bearing weight, helps improve bone mineral density and protect against fracture—across all age groups, and regardless of whether you’re male or female. Mechanical loads from extra weight (from dumbbells, grocery bags, your children, your overweight cat, or even from your own body as you perform squats and similar exercises) stimulate cells called osteoblasts, which are responsible for synthesizing and mineralizing bone tissue. Engaging in gentle weight-bearing exercise throughout the day (hello, walking!) is a great investment for your skeletal health.
It’s also important to emphasize that the goal is to incorporate gentle movement throughout the day is in addition to some form of more moderately-intense activity at least a few times a week. I’m absolutely NOT saying that lifting weights, CrossFit, yoga, or a challenging hike aren’t amazingly good for you! In fact, muscle mass is a key predictor of health and longevity in people over 65 years old; and for everyone else, every 10% increase in the ratio of muscle mass to total bodyweight decreases risk of type 2 diabetes by 12%. There’s absolutely tons of benefits to including more rigorous exercise in our life, (although prolonged strenuous exercise can be a problem, see Why Exercising Too Much Hurts Your Gut).
When we are incorporating enough movement into our lives in the right frequencies, we can reap the many benefits. But, the stressful load of exercise requires the synergistic element of sleep to really give our bodies the complete physiological and mental betterments.
Sleep: The Foundation of Recovery
Sleep is an incredibly important aspect of life. As I discuss in Go to Bed, sleep is a cornerstone of health and is the foundation of recovery from our load. Without it, we cannot recover from whatever stressors we face. We just can’t.  The interrelationship between sleep and load can’t be understood without a thorough review of the basic functions of sleep. Indeed, much like our discussion of exercise, there are different aspects of sleep that merit attention to detail: namely, the different stages of sleep! Each stage of sleep contributes to our recovery from physical and mental load differently. Although the details remain a mystery, the sleep cycle stems from an interaction between the circadian clock and a separate sleep-wake homeostatic process.
The interrelationship between sleep and load can’t be understood without a thorough review of the basic functions of sleep. Indeed, much like our discussion of exercise, there are different aspects of sleep that merit attention to detail: namely, the different stages of sleep! Each stage of sleep contributes to our recovery from physical and mental load differently. Although the details remain a mystery, the sleep cycle stems from an interaction between the circadian clock and a separate sleep-wake homeostatic process.
Here is a brief review of the different stages of sleep, including non-REM and REM (Rapid Eye Movement).
Stage 1 sleep is a light non-REM sleep that begins the moment you drift off. You can think of stage 1 like your transition from being awake to being asleep. During this stage, which lasts only about 5 minutes, your heart rate will decline, your body temperature will drop, and your eyes will slowly move in a pattern from side to side. This phase of sleep is usually dreamless and is easily disturbed.
After that, the body begins to transition into established sleep. In stage 2 sleep, which lasts between 10 and 25 minutes in our first sleep cycle (remember: each cycle lasts longer and longer), eye movement stops and brain waves become slower with only an occasional burst of rapid brain waves, called “sleep spindles.” During sleep spindles, which it is theorized the brain is sorting through the information it picked up that day and synthesizing it with existing knowledge. As you might have expected, memory consolidation occurs while we are in stage 2 sleep. Along with sleep spindles, the brain activity of stage 2 sleep is characterized by sharp, short bursts of brain activity; these brainwaves are called a “K-complex,” and scientists believe that their purpose is to keep the brain prepared in the event that we need to be awakened.
 Deep sleep begins when a person enters stage 3 sleep, characterized by extremely slow brain waves called delta waves. During this stage, more of the brain’s active centers shut down for the night, and the remaining active brain cells become more synchronized in their brainwave pattern. As the neurons fire in more synchronized patterns, their combined frequencies increase to create the delta waves. The goal of stage 3 sleep is to get to this point. In stage 4 (which, again, some scientists characterize as just an extension of stage 3), the brain produces the slow delta waves almost exclusively. This is why the stages 3 and 4 are referred to as slow-wave sleep, deep sleep, or delta sleep. In this stage of sleep, there is no eye movement or muscle activity, blood pressure is reduced by 20-30%, and the brain becomes much less responsive to external stimuli. It is very difficult to wake someone from deep sleep—and if you do happen to wake up during this stage, you will likely feel very groggy and unrested. This is when some children experience bedwetting, sleepwalking or night terrors.
Deep sleep begins when a person enters stage 3 sleep, characterized by extremely slow brain waves called delta waves. During this stage, more of the brain’s active centers shut down for the night, and the remaining active brain cells become more synchronized in their brainwave pattern. As the neurons fire in more synchronized patterns, their combined frequencies increase to create the delta waves. The goal of stage 3 sleep is to get to this point. In stage 4 (which, again, some scientists characterize as just an extension of stage 3), the brain produces the slow delta waves almost exclusively. This is why the stages 3 and 4 are referred to as slow-wave sleep, deep sleep, or delta sleep. In this stage of sleep, there is no eye movement or muscle activity, blood pressure is reduced by 20-30%, and the brain becomes much less responsive to external stimuli. It is very difficult to wake someone from deep sleep—and if you do happen to wake up during this stage, you will likely feel very groggy and unrested. This is when some children experience bedwetting, sleepwalking or night terrors.
Deep sleep seems to be one of the most critical times for body repair (like recovering from physical activity!). At the beginning of stage 3/4, the pituitary gland releases growth hormone, which stimulates the growth and repair of important tissues. Your brain cools during this phase, as less blood is directed to it (in part because of the lowered blood pressure), which may help to improve its function and allow for repair. Interestingly, it seems that there are also increased levels of interleukins (there are many different types, all of which are released by white blood cells, some which reduce inflammation and some which stimulate inflammation), indicating increased immune system activity during this phase of sleep as well; so, immune function is related to deep sleep too! Since slow-wave sleep is so important, our bodies designate a lot of time to it: at its peak importance, which is generally young adulthood, deep sleep makes up about 20% of our total sleeping time, but then it declines in later adulthood (especially after the age of 65). When someone is sleep-deprived, they pass more quickly through the earlier stages of sleep and spend more time in this stage as well.
After deep sleep, REM sleep begins. Brain waves during REM sleep increase to levels experienced when a person is awake, appearing more erratic in their pattern and with higher frequency. Unlike the restorative quality of “quiet sleep,” this dreaming, “active” sleep is just that: it is almost as active as if you were awake! In general, breathing becomes more rapid, irregular and shallow, eyes jerk rapidly, and limb muscles are temporarily paralyzed (except in those who sleepwalk, acting out their dreams). Similarly, heart rate increases, blood pressure rises, sex organs become aroused, and the body loses some of the ability to regulate its temperature. Additionally, the sympathetic nervous system, which is responsible for the “fight or flight” response, is twice as active as when you’re awake! However, despite all of this activity, your body remains relatively still, since all muscles except for those controlling eye movement and breathing are paralyzed during this phase of sleep. This is the time when most dreams occur. Scientists are still trying to understand how dreams contribute to our health and what they may mean, but it appears that dreaming sleep is really important for managing learning and memory. Studies have shown that repeated interruption of REM sleep, rather than NREM sleep, decreases cognitive performance compared to a night with the standard 3-5 REM cycles. In total, REM sleep accounts for about one to two hours of your sleep each night, with the rest of the time spent in light sleep to deep (NREM) sleep.
 The amount of time that we spend in each stage of sleep (especially deep sleep and REM sleep) varies, but inadequate amounts of time in these stages might seriously affect our health. Knowing how much time we spend in each sleep stage is hugely beneficial if we can find the appropriate wearable device, because certain interventions may impact our sleep differently (and thus the benefits we get from proper exercise recovery). Importantly, it’s not just about optimizing our sleep – from a health perspective, we really just can’t afford to miss out on Z’s.
The amount of time that we spend in each stage of sleep (especially deep sleep and REM sleep) varies, but inadequate amounts of time in these stages might seriously affect our health. Knowing how much time we spend in each sleep stage is hugely beneficial if we can find the appropriate wearable device, because certain interventions may impact our sleep differently (and thus the benefits we get from proper exercise recovery). Importantly, it’s not just about optimizing our sleep – from a health perspective, we really just can’t afford to miss out on Z’s.
Epidemiological studies show a strong correlation between short or disturbed sleep and obesity, diabetes and cardiovascular disease (see Sleep and Disease Risk: Scarier than Zombies!). In fact, lack of adequate sleep has been associated of increased morbidity and mortality from all causes. Studies have also evaluated the role that sleep plays in healing from specific diseases, like breast cancer, and show that the less you sleep, the less likely you are to survive. Sleep deprivation is also associated with increased susceptibility to infection. In fact, the less sleep you get, the more likely you are to catch the common cold. Getting adequate sleep can also protect you from infection. One study even showed that the longer the sleep duration, the lower the incidence of parasitic infections in mammals.
So, how much sleep do you need? There is no clear answer to this. Consensus is that healthy adults need 7-10 hours of sleep per night (see Sleep Requirements and Debt: How do you know how much sleep you need?). If you are trying to heal from an autoimmune disease, don’t be surprised if what your body needs is on the longer end of that range (say 9 to 10 hours) or even exceeding that range (some people with autoimmune disease report needing 12 hours of sleep every night to heal).
Like all things in physiology, sleep and exercise do not act independently when it comes to balance – rather, these lifestyle factors have been shown to directly influence each other.
Sleep <=> Exercise
These two activities are even more intertwined than you might think! In fact, the science tells us that they influence each other greatly. Scientists believe that sleep and exercise influence each other through complex interactions between psychological and physiological pathways throughout our bodies.
Anyone who’s spent a significant amount of time and effort training knows that a bad night’s sleep can impact our performance in the gym. This phenomenon is well understood and delineated in the literature. There are several proposed mechanisms for how poor sleep (we’re talking quantity AND quality) impacts athletic performance within just one day:
- Autonomic nervous system dysfunction. The autonomic nervous system, divided into the sympathetic and parasympathetic branches, works to regulate the functions of our organs and other bodily functions that we don’t think about. Dysfunction of this system would certainly impact our performance in the gym, because fine-tuned regulation of autonomic processes like heart rate and breathing rate is necessary for intense exercise (to meet the needs of our tissues as they go through tons of cellular energy to move us around!).
- Increases in pro-inflammatory cytokines. Have you ever underslept… and then overdid it in the gym… and then woke up sick the next day? That phenomenon is explained with this finding. Not getting enough sleep increases the release of inflammatory cytokines, which may contribute to systemic inflammation or make us more susceptible to infections.
- Cognitive function decreases. Another well-understood impact of less sleep is that it decreases our cognitive function. While that may seem unrelated to exercise, it might impact things like our reaction times (hello, wallball!). This also makes us more susceptible to injuries.
Apart from day-to-day performance details, getting enough sleep regularly impacts our ability to recover from the previous day’s exercise and promotes long-term growth of muscle as well as improved cardiovascular function.
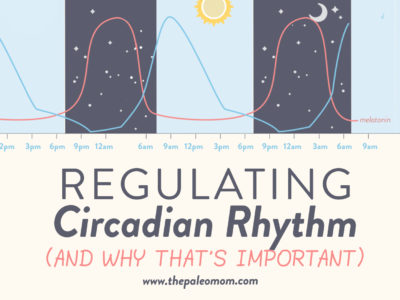
 Conversely, exercise affects our sleep! There’s a reason why getting 30 minutes of exercise is included in my 14-Day Go to Bed Challenge. Studies show that inactivity causes poor sleep. The main proposed mechanism of this relationship is that exercise impacts our hormones; specifically, mild-to-moderate exercise is very beneficial to hormone regulation, including hunger hormones, insulin sensitivity, and, most importantly, cortisol (the stress hormone). Cortisol is known to act directly against the pro-sleep hormone, melatonin, so getting exercise (which often causes a spike of cortisol, as it is a physical stressor) earlier in the day is often best (melatonin starts to be secreted in the evening and peaks in the middle of the night. Exercising also increases blood flow to the brain, which can help reduce inflammation in the brain (which also has the net effect of boosting your mood), which is an important strategy for those with gut-brain axis problems. Along those lines, I can’t help but wonder if exercise may aid in optimizing the glymphatic system, which is what clears the toxins from the brain overnight. Clearly, activity is essential for sleep health! There is evidence supporting both aerobic activity (like jogging, walking, rowing, etc.) and resistance training (lifting weights), so incorporating both into our routines is the best way to optimize sleep!
Conversely, exercise affects our sleep! There’s a reason why getting 30 minutes of exercise is included in my 14-Day Go to Bed Challenge. Studies show that inactivity causes poor sleep. The main proposed mechanism of this relationship is that exercise impacts our hormones; specifically, mild-to-moderate exercise is very beneficial to hormone regulation, including hunger hormones, insulin sensitivity, and, most importantly, cortisol (the stress hormone). Cortisol is known to act directly against the pro-sleep hormone, melatonin, so getting exercise (which often causes a spike of cortisol, as it is a physical stressor) earlier in the day is often best (melatonin starts to be secreted in the evening and peaks in the middle of the night. Exercising also increases blood flow to the brain, which can help reduce inflammation in the brain (which also has the net effect of boosting your mood), which is an important strategy for those with gut-brain axis problems. Along those lines, I can’t help but wonder if exercise may aid in optimizing the glymphatic system, which is what clears the toxins from the brain overnight. Clearly, activity is essential for sleep health! There is evidence supporting both aerobic activity (like jogging, walking, rowing, etc.) and resistance training (lifting weights), so incorporating both into our routines is the best way to optimize sleep!
An important thing to note is that overtraining has the opposite effect on sleep. Overtraining is a highly individual phenomenon that results from exercising too much without allowing the body to recover. Exercising too much actually decreases sleep quality and can cause increased sleep latency (the amount of time it takes us to go to sleep). Plus, difficulty sleeping is actually a sign of overtraining… just another point to how much sleep and exercise are related, and how much we need to balance these activities!
So, we’ve talked a lot about the relationship between sleep and exercise, really pinning down how important it is to give them equal clout on our to-do lists, but there’s another factor here that we can’t ignore: stress! In fact, stress is a huge moderating factor in the relationship between sleep and exercise (especially when we consider the fact that exercise is absolutely a form of physical stress).
Stress: How Do We Measure Mental Load?
Like sleep, stress affects every system of our bodies. But, I think for this purpose, we can consider it a tally in the “mental load” category, as it is regulated by the brain and oftentimes a result of perceived threats (that sounds pretty mental to me). Like sleep and exercise, stress merits some background discussion so that we can understand its importance in the picture of pursuing balance.
Historically, all stress was acute and would include situations such as being chased by a lion or slipping off the edge of a cliff. During these events, the fight-or-flight response is activated, and cortisol and adrenaline work together to ensure survival. At the end of the event, you are either dead (because you fell from the cliff onto craggy rocks four hundred feet below) or alive and safe (because you grabbed onto a branch as you slipped off the cliff and pulled yourself back up to safety). In either case, there is no need for the body to continue producing adrenaline and excess cortisol (more on this below). Levels return to normal (unless you’re dead, of course), and you go on your merry way.
Chronic stress is that unrelenting stress that never goes away. It can be at a low level, perhaps the stresses we all experience from having a job, raising kids, and having to make ends meet. It can be moderate, perhaps from an impending deadline or exam, your kids getting into trouble at school, or ripping your favorite shirt. It can also be high, such as illness, divorce, or a death in the family. What’s different about chronic stress is that it’s never over. There’s no big relief at the end before you go on your merry way. It’s always there, having its insidious effects that build up over time. How quickly and severely the effects of chronic stress are felt depends on the severity of the stress and your resilience (more on that below too).
Like the other factors we already discussed, an imbalance in the amount of stress we have can be hugely detrimental to our health (and yes, a little bit of mental load is actually healthy! It’s the long-term stress that really gets us). Chronic stress is known to affect health in a variety of ways, including causing the development of metabolic syndrome (the nasty combination of obesity, insulin resistance, and high blood pressure), dysregulation of the hypothalamic-pituitary-adrenal axis along with sympathetic nervous system activation, sleep disturbances, systemic inflammation, impaired immunity functions, blood coagulation and fibrinolysis, and poor health behaviors (chronic stress causes increased appetite, cravings for energy-dense foods, and uninhibited eating behaviors). See also Demystifying Adrenal Fatigue, Pt. 1: What Is Adrenal Fatigue?
Importantly, stress impacts both sleep and our athletic performance (oh, what a complicated web we weave, am I right?!). So, when we’re experiencing stress, it influences our ability to get the physical load we need, AND it impedes our ability to recover via sleep! I won’t drone on about this, because I believe we all have the picture here. When we discuss balancing our load, we can’t ignore the role that stress plays in our needs – that is why I included stress management as one of the necessary tools for recovery. But, compared to our physical load and our recovery, it’s more difficult to measure our mental load, which makes the goal of balance much more difficult to attain. Luckily, we are now gaining more resources to measure the effect that stress is having on our bodies (thereby elucidating how much stress we’re really under!).
Heart Rate Variability: the Red Flag
Now, we know that the right kinds of sleep and exercise are critical for our health, and we understand that modulating stress is another way to improve both… but how do we really know if we’re striking the right balance? Firstly, we can listen to our bodies. How do we feel? The “just right” feeling is individual, but someone who is making the right choices in both realms is likely to be making gains and meeting other goals in the gym (and life!) while still feeling rested upon waking in the morning. Next, it might be best to measure our resilience in other ways. This might include hormonal testing or visiting our doctor or functional medicine practitioner for a check-up, but there are now ways to measure our resilience at home that might be as good as going to the doc (seriously). With that, we are now exploring ways to examine how our bodies are affected by stress (this might also be discussed as “arousal” or “anxiety” or “alertness” in the scientific literature, which muddles interpretation a bit). Because stress has such a huge impact on our health, getting a handle on how much stress our bodies are registering is very valuable. So, how do we do that?
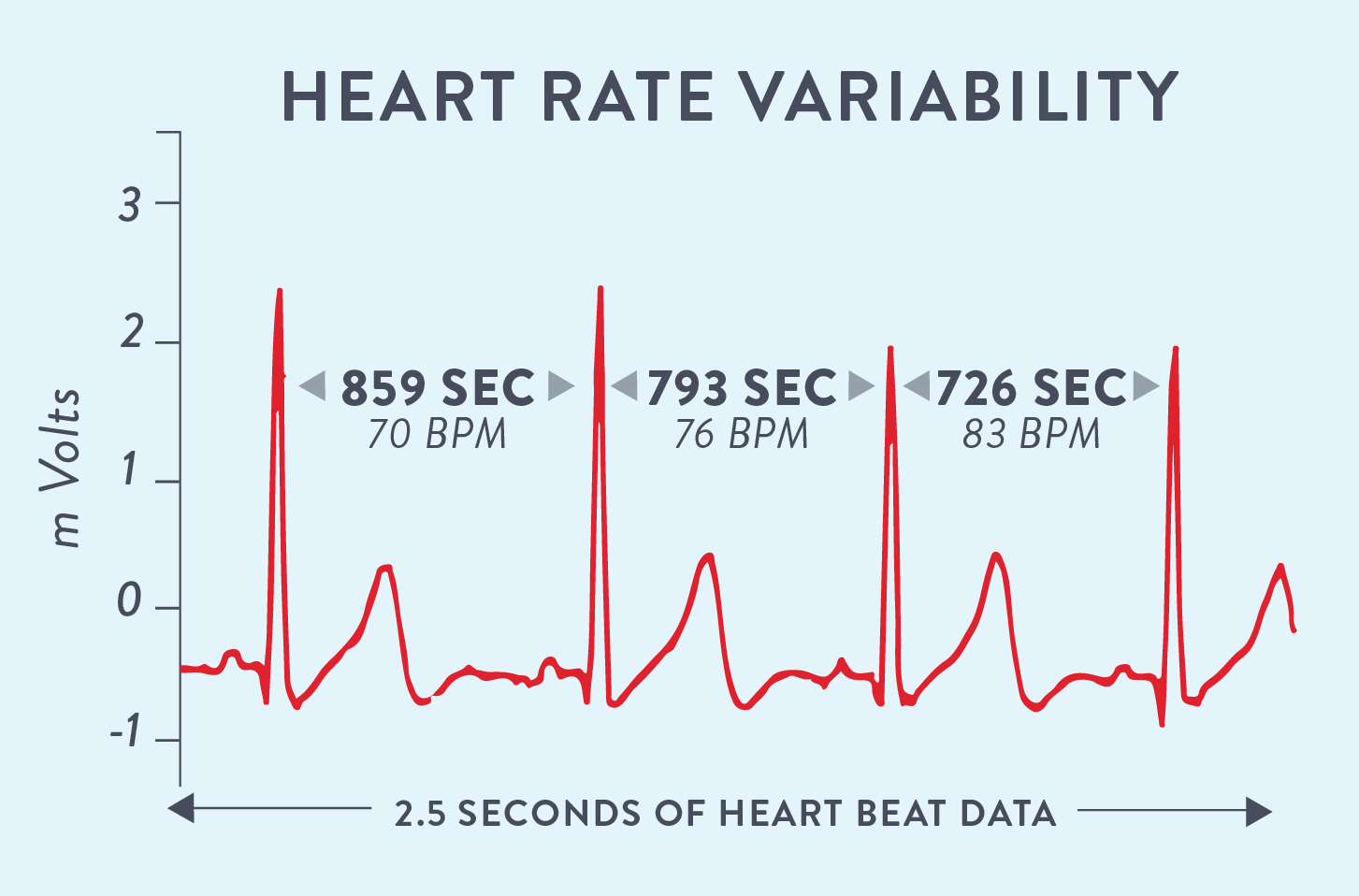 There’s a new(ish) measure of stress that is all over the scientific community, now spreading into the public domain: heart rate variability (HRV). Unlike what we had previously thought, there is a great deal of variance in our heart’s rate and rhythm (so much so that physicians can’t detect variability when taking our heart rate in their offices, which is really an average rate over the course of a minute. We’re talking about variability from second to second!); the change in intervals between heartbeats is referred to as HRV. How? The autonomic nervous system is activated in response to the perceived threat (anyone who’s had anxiety or experienced chronic stress knows that the “threat” definitely feels real!), and this leads to a more regulated interval between heartbeats. Like most physiological measures, there is an optimal level of HRV, though generally speaking, the higher the HRV, the better. More variability reflects a resilient and healthy cardiovascular system (as well as all of the necessary hormonal balance and health systems necessary for a strong heart), and decreased variability may be related to one of the many ways we experience stress. Scientists have spent a lot of time figuring out how HRV is related to health (or lack thereof); in fact, lower HRV is associated with higher mortality (death risk) overall as well as chances of developing hypertension, type 2 diabetes, chronic obstructive pulmonary disease, and others.
There’s a new(ish) measure of stress that is all over the scientific community, now spreading into the public domain: heart rate variability (HRV). Unlike what we had previously thought, there is a great deal of variance in our heart’s rate and rhythm (so much so that physicians can’t detect variability when taking our heart rate in their offices, which is really an average rate over the course of a minute. We’re talking about variability from second to second!); the change in intervals between heartbeats is referred to as HRV. How? The autonomic nervous system is activated in response to the perceived threat (anyone who’s had anxiety or experienced chronic stress knows that the “threat” definitely feels real!), and this leads to a more regulated interval between heartbeats. Like most physiological measures, there is an optimal level of HRV, though generally speaking, the higher the HRV, the better. More variability reflects a resilient and healthy cardiovascular system (as well as all of the necessary hormonal balance and health systems necessary for a strong heart), and decreased variability may be related to one of the many ways we experience stress. Scientists have spent a lot of time figuring out how HRV is related to health (or lack thereof); in fact, lower HRV is associated with higher mortality (death risk) overall as well as chances of developing hypertension, type 2 diabetes, chronic obstructive pulmonary disease, and others.
Many scientists are studying the relationship between HRV and stress, and it looks like changes in HRV is one of the most sensitive ways to quantify our physiological stress (and changes in HRV seem highly related to improving perceived stress).
HRV is highly related to the question at hand: balance. For any given person, a normal HRV or higher may indicate that we’ve done a good job of keeping load (including physical and mental stressors) and rest in balance. However, a decreased HRV in the long term is almost definitely related to high load and/or inadequate recovery. And considering the number of health risks associated with reduced HRV (most notably, increased risk of heart attack), HRV might just be the red flag when it comes to balance.
I can’t stress this enough: all signs point to balance being an absolute necessity for health. So, it is worth our time to keep track of whether we’re in balance as much as we can. Fortunately, we now have the option of purchasing wearable devices that give us enough feedback (like measuring activity, sleep and HRV) to tweak our lifestyle and get the most health benefit.
Getting It Right: It’s All About the Numbers!
 I believe that we can tweak our routines and habits to optimize our health and wellness, and a fundamental tool for this optimization is to use wearable tracking devices to gather data and make informed decisions about our own bodies moving forward. While we can guess how we’re doing at balance, there are now tools that provide amazingly accurate data for us. In fact, there is now a wearable device that even utilizes the inputs we discussed above – sleep, movement, and HRV/stress – to determine how well we’re balancing each factor.
I believe that we can tweak our routines and habits to optimize our health and wellness, and a fundamental tool for this optimization is to use wearable tracking devices to gather data and make informed decisions about our own bodies moving forward. While we can guess how we’re doing at balance, there are now tools that provide amazingly accurate data for us. In fact, there is now a wearable device that even utilizes the inputs we discussed above – sleep, movement, and HRV/stress – to determine how well we’re balancing each factor.
I’ve been using an Ōura Ring, a new and advanced lifestyle tracking tool, for nearly two months, and I’ve been incredibly impressed. One of the biggest and best features of the Ōura Ring is that it gives us information on balancing our “load” (this includes the physical activity and other stressors that we might face during our everyday lives) according to the amount and quantity of rest we get during the night. Basically, it’s reducing all the work of figuring out our personal balancing acts into one output on a phone app: our daily “readiness score.” This score is intended to be a reflection of our physiological resilience – calculated each and every day! There are seven factors that contribute to the readiness score:
- Previous night’s sleep
- Sleep balance
- Previous day’s activity
- Activity balance
- Body temperature
- Resting heart rate
- Recovery index (overnight HRV)
The readiness score gives us a good idea of how well we balance our rest and physical activity. With a score of 85 to 100, we know it’s a good day to push ourselves. A score of 75 to 85 indicates the need for a more moderate load day and a focus on recovery activities. A score less than 75 tells us that it’s a good day to take it easy and make choices that reduce stress and improve sleep. The people behind Ōura are totally on board when it comes to the importance of sleep and believe that it is a cornerstone of health. The Ōura Ring is able to track our sleep and exercise in an incredible level of detail and confidence because of the ring technology; in fact, the pulses measured at the fingers are 100x more accurate than those measured at the wrist! Everything Ōura measures and recommends is based on scientific evidence.
The Ōura Ring measures an amazing number of different physiological variables that focus on balancing load and recovery, including movement, heart rate, HRV, pulse wave form, and skin temperature. Sleep quantity and quality are measured at an accuracy rivaling a hospital sleep study, providing us with critical information on the amount of deep and REM sleep we’re getting. Plus, we get tons other information that reflects our health, including HRV!
Achieving balance is a noble goal that requires attention to detail, time management, and a lot of effort. Using a tool like the Ōura Ring has made my balance goal for 2017 seem more attainable; luckily, Ōura has agreed to help out my readers by giving them an incredible deal!
Citations
Alley JR, Mazzochi JW, Smith CJ, Morris DM, Collier SR. Effects of resistance exercise timing on sleep architecture and nocturnal blood pressure. J Strength Cond Res. 2015;29(5):1378-85.
Bollinger, T., et al., Sleep-dependent activity of T cells and regulatory T cells, Clin Exp Immunol. 2009 Feb;155(2):231-8
Bosy-Westphal, A., et al., Influence of partial sleep deprivation on energy balance and insulin sensitivity in healthy women, Obes Facts. 2008;1(5):266-73
Boudjeltia KZ, et al., Sleep restriction increases white blood cells, mainly neutrophil count, in young healthy men: a pilot study, Vasc Health Risk Manag. 2008;4(6):1467-70.
Chennaoui M, Arnal PJ, Sauvet F, Léger D. Sleep and exercise: a reciprocal issue?. Sleep Med Rev. 2015;20:59-72.
Cohen, S et a., Psychological Stress and Disease, JAMA. 2007;298(14):1685-1687. doi:10.1001/jama.298.14.1685.
Cohen, S., et al., Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk, Proc Natl Acad Sci U S A. 2012;109(16):5995-9
Dhabhar, F. S. and McEwen, B. S., Acute stress enhances while chronic stress suppresses immune function in vivo: a potential role for leukocyte trafficking, Brain Behav Immun. 1997;11:286-306
Donga, E., et al., A single night of partial sleep deprivation induces insulin resistance in multiple metabolic pathways in healthy subjects, J Clin Endocrinol Metab. 2010 Jun;95(6):2963-8.
Dzierzewski JM, Buman MP, Giacobbi PR, et al. Exercise and sleep in community-dwelling older adults: evidence for a reciprocal relationship. J Sleep Res. 2014;23(1):61-8.
Frey, D.J., et al., The effects of 40 hours of total sleep deprivation on inflammatory markers in healthy young adults, Brain Behav Immun. 2007 Nov;21(8):1050-7
Fullagar HH, Skorski S, Duffield R, Hammes D, Coutts AJ, Meyer T. Sleep and athletic performance: the effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sports Med. 2015;45(2):161-86.\
Heslop, P., et al., Sleep duration and mortality: The effect of short or long sleep duration on cardiovascular and all-cause mortality in working men and women, Sleep Med. 2002 Jul;3(4):305-14.
Hirotsu, C., et al., Sleep loss and cytokines levels in an experimental model of psoriasis, PLoS One. 2012;7(11)
Lehrer S, et al., Insufficient sleep associated with increased breast cancer mortality, Sleep Med. 2013 Mar 4 pii: S1389-9457(12)00384-X. doi: 10.1016/j.sleep.2012.10.012. [Epub ahead of print]
Lucassen EA, et al., Interacting epidemics? Sleep curtailment, insulin resistance, and obesity, Ann N Y Acad Sci. 2012 Aug;1264(1):110-34
Meier-Ewert HK, et al., Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk, J Am Coll Cardiol. 2004 Feb 18;43(4):678-83.
Palma, B.D. & Tufik, S., Increased disease activity is associated with altered sleep architecture in an experimental model of systemic lupus erythematosus, Sleep. 2010 Sep;33(9):1244-8.
Palma, B.D., et al., Effects of sleep deprivation on the development of autoimmune disease in an experimental model of systemic lupus erythematosus, Am J Physiol Regul Integr Comp Physiol. 2006 Nov;291(5):R1527-32.
Ranjbaran, Z., et al., The relevance of sleep abnormalities to chronic inflammatory conditions, Inflamm Res. 2007 Feb;56(2):51-7.
Reynolds AC, et al., Impact of five nights of sleep restriction on glucose metabolism, leptin and testosterone in young adult men, PLoS One. 2012;7(7)
van Leeuwen WM, et al., Sleep restriction increases the risk of developing cardiovascular diseases by augmenting proinflammatory responses through IL-17 and CRP, PLoS One. 2009;4(2)
Wu, G., et al., Understanding resilience, Front Behav Neurosci. 2013;7:10