SCIENCE SIMPLIFIED:
- Caffeine is generally anti-inflammatory but the effects of coffee on immune function are complicated.
- In some people coffee consumption decreases inflammatory mediators, but in other people exactly the opposite effects occur.
- It’s still unclear why coffee is beneficial to immune function in some people and harmful in others, but two groups of autoimmune disease risk genes (NAT2 and HLA) are implicated in this relationship.
- It’s likely that coffee is helpful for some people with autoimmune disease, but drives autoimmune disease activity in others, therefore the best practice is to eliminate coffee initially on the Autoimmune Protocol and reintroduce later.
RELATED READING:
- Coffee as a Mediator of Health & Longevity
- The Autoimmune Protocol
- Reintroducing Foods after Following the Autoimmune Protocol
 For many of us, any study suggesting our coffee-drinking habits might be good for us is a reason to celebrate (and to raise our mugs of hot delicious Americanos in toast)! And as luck would have it, a number of research studies show that drinking coffee in moderation could legitimately provide a range of health benefits, including reducing the risk of certain cancers, stroke, diabetes, Parkinson’s disease, Alzheimer’s disease, cardiovascular disease, gout, gallstones, and depression, along with protecting against antibiotic-resistant bacterial infections and cirrhosis of the liver. It can even reduce muscle soreness after a workout! There are even studies, including some new and robust ones, that show coffee drinking as a mediator of all-cause mortality, suggesting that drinking coffee every day can have a life-extending effect. In fact, a meta-analysis from 2014 found that drinking four cups per day was associated with a 16% reduction in all-cause mortality (as well as a 21% reduction in cardiovascular disease mortality).
For many of us, any study suggesting our coffee-drinking habits might be good for us is a reason to celebrate (and to raise our mugs of hot delicious Americanos in toast)! And as luck would have it, a number of research studies show that drinking coffee in moderation could legitimately provide a range of health benefits, including reducing the risk of certain cancers, stroke, diabetes, Parkinson’s disease, Alzheimer’s disease, cardiovascular disease, gout, gallstones, and depression, along with protecting against antibiotic-resistant bacterial infections and cirrhosis of the liver. It can even reduce muscle soreness after a workout! There are even studies, including some new and robust ones, that show coffee drinking as a mediator of all-cause mortality, suggesting that drinking coffee every day can have a life-extending effect. In fact, a meta-analysis from 2014 found that drinking four cups per day was associated with a 16% reduction in all-cause mortality (as well as a 21% reduction in cardiovascular disease mortality).
Two important prospective cohort studies, recently published on the same day in the Annals of Internal Medicine, confirmed a mortality-reducing effect of coffee across a wide spectrum of populations. The first study—encompassing 10 different European countries and a total of 521,330 people—found that the highest coffee consumers (28 ounces per day for men and 23 ounces per day for women) had significantly lower all-cause mortality (12% lower for men, 7% lower for women) compared to people who didn’t drink coffee at all. This study also found that the highest coffee consumers had lower risk of death from digestive diseases (59% lower for men and 40% lower for women), and that the highest coffee-consuming women (but not men) had a 30% reduction in cerebrovascular diseases and a 22% reduction in circulatory diseases.
The second prospective cohort study confirmed that coffee’s mortality benefits hold true for non-white ethnic groups (an important finding, because data for coffee and mortality is sparse for non-whites, and there are many instances where dietary variables have different effects depending on a person’s ethnic background). Analyzing data from the Multiethnic Cohort, this study looked at 185,855 African Americans, Native Americans, Japanese Americans, Latinos, and whites and found that even after adjusting for smoking and other potential confounders, drinking at least two cups per day was associated with an 18% reduction in total mortality. Only in Native Hawaiians did coffee’s inverse association with total mortality not reach statistical significance. (Coffee also appeared protective against death from heart disease, stroke, cancer, diabetes, kidney disease, and respiratory disease in this analysis!)
Some of these effects are owed to the antioxidants, polyphenols, and bioactive compounds found in coffee (including some with insulin-sensitizing and anti-inflammatory properties). Some of the health benefits of coffee are also directly attributable to its caffeine content (which is why drinking tea—which is rich in antioxidants and polyphenols while also containing caffeine—is also associated with good health). This is partly why many of the health-protective effects of coffee are not seen with decaf coffee. In addition, the decaffeination process tends to strip the coffee not only of much of its caffeine content, but also of many of its antioxidants and polyphenols (potentially leaving behind a few of the more harmful substances that can be found in coffee).
Despite that great news, coffee can be a double-edged sword. One of the most prominent ways that applies (especially for me and my AIP readers) is that there is some evidence that coffee is a no-go for people with autoimmune disease. Before we get into the specifics, I want to briefly review the ways that we know coffee and caffeine impact the immune system.
Coffee’s Effect on the Immune System
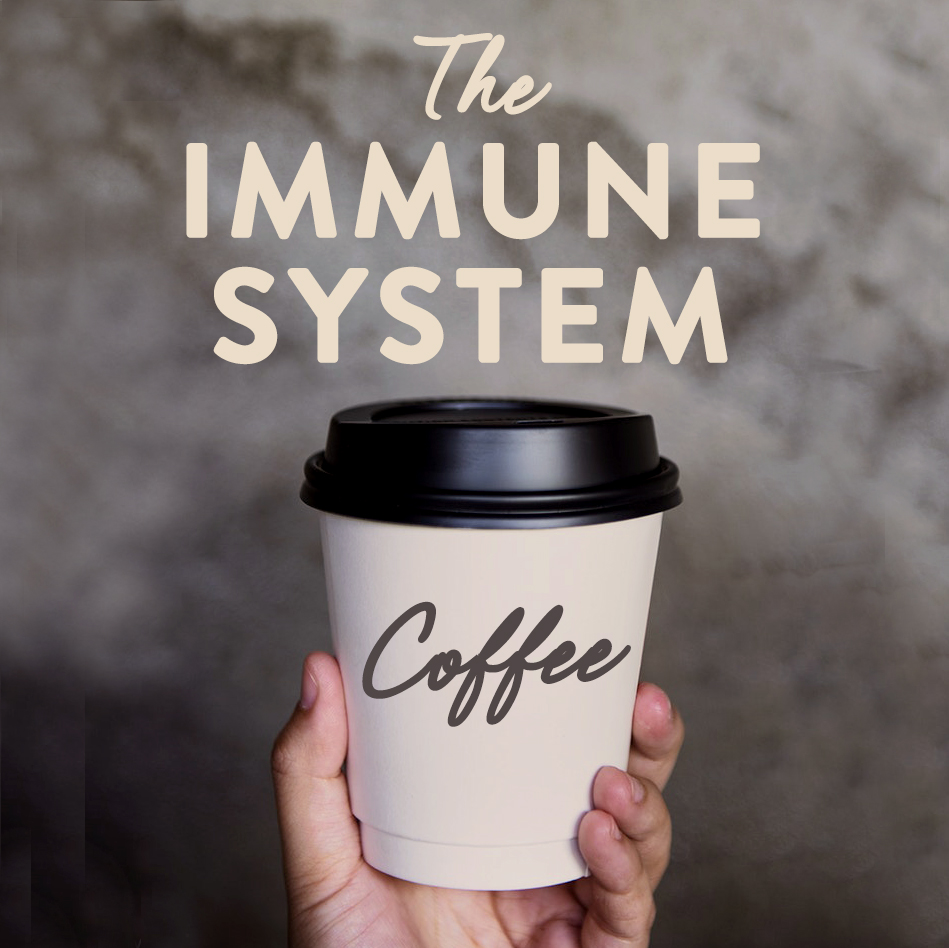 Scientific evidence demonstrates that coffee interacts with the immune system, but the effects are complicated and may be highly individualized, suggesting an interaction with genetics.
Scientific evidence demonstrates that coffee interacts with the immune system, but the effects are complicated and may be highly individualized, suggesting an interaction with genetics.
Generally-speaking, caffeine acts in an anti-inflammatory way on multiple components of the immune system. However, multiple studies have shown higher levels of inflammation in habitual coffee drinkers than in non-coffee drinkers. For example, one key study showed that moderate coffee consumption in healthy individuals correlated with increased markers of inflammation in their blood (C-reactive protein (CRP), serum amyloid-A, and white blood cell counts). People who drank more than 200 mL of coffee every day (equivalent to 37.3 mg of caffeine) had increased circulating white blood cells and several key inflammatory cytokines (chemical messengers of inflammation, including interleukin 6 and tumor necrosis factor alpha). These increases in markers of inflammation were persistent even after adjusting for other health and lifestyle factors (such as age, sex, weight, exercise, and smoking). However, other studies have shown a decrease in markers of inflammation with moderate coffee consumption, even in diabetics and obese individuals.
Studies that have evaluated the impact of caffeine and/or coffee consumption on specific cells and cytokines within both the innate and adaptive immune system also demonstrate a non-homogeneous effect. (Remember: the innate immune system is the body’s nonspecific first line of defense against foreign invaders, in contrast to the adaptive immune system, which is more complex and involves immunological memory of specific antigens. The innate immune system is our first response to pathogens and is responsible for generalized inflammation whereas adaptive immunity takes longer to activate but attacks antigens with high specificity thanks to the coordinated actions of T cells and B cells. See What Is the Gut Microbiome? And Why Should We Care About It?)
Save 70% Off the AIP Lecture Series!
Learn everything you need to know about the Autoimmune Protocol to regain your health!
I am loving this AIP course and all the information I am receiving. The amount of work you have put into this is amazing and greatly, GREATLY, appreciated. Thank you so much. Taking this course gives me the knowledge I need to understand why my body is doing what it is doing and reinforces my determination to continue along this dietary path to heal it. Invaluable!
Carmen Maier
Studies have shown that that neutrophils and monocytes, two important cell types of the innate immune system, exhibit decreased chemotaxis (movement towards a chemical signal), which indicates suppression of the innate immune system. However, this is counterbalanced by another study showing increased endothelial dysfunction-related inflammation biomarkers, including endothelial adhesion molecules, which are like microscopic velcro embedded in the outer cell membrane that interact with other adhesion molecules on white blood cells to facilitate their exit from the bloodstream (called extravasation) and entrance into tissues (inflammation).
In terms of the adaptive immune system, caffeine intake suppresses proliferation (cell division and expansion) of Th1 and Th2 cells, but also Th3 cells which are key inducible regulatory T cells. Caffeine intake can also alter B cell function and leads to the suppression of antibody production. It seems to have no impact on natural killer cell activity (an important cell type in cancer development, see TK). Coffee galactomannans, on the other hand, are immunostimulatory, increasing activity of B cells and T cells (the study that showed this measured an increase in both CD4+ and CD8+ T cell activity, but did not differentiate helper T cell subtypes or regulatory T cells).
Cell signaling is also affected by coffee intake. NF-κB is a protein complex that controls cytokine production (in addition to transcription of DNA and cell survival) and is a critical factor of the intestinal immune system. Autoimmune and chronic inflammatory conditions (e.g., inflammatory bowel disease) are associated with chronic activation of NF-κB. Studies show that coffee induces activation (specifically, nuclear translocation) of NF-κB in macrophages, intestinal epithelial cells (the cells that form the gut barrier) and intestinal endothelial cells (the cells that form capillaries). Caffeine increases expression of the anti-inflammatory cytokine interleukin-10 (IL-10), which suppresses Th1 pathways. To muddy the waters, coffee increases expression of the anti-inflammatory cytokine IL-2, which stimulates regulatory T cell pathways, except in the context of allergen sensitization, in which is suppresses IL-2 release!
A 2016 study may shed some light on these apparent contradictions. The authors took blood samples from volunteers before and after coffee, subjected the isolated blood cells to an inflammatory stimulus, and measured the response of the cells using mass spectrometric measurement of cytokines, chemokines, and eicosanoids, which are mediators of inflammation. The authors summarize their surprising results thusly: “Remarkably, the release of inflammation mediators IL-6, IL-8, GROA, CXCL2, CXCL5 as well as PGA2, PGD2, prostaglandin E2 (PGE2), LTC4, LTE4, and 15S-HETE was significantly affected after coffee consumption. While in several individuals coffee consumption or caffeine treatment caused significant downregulation of most inflammation mediators, in other healthy individuals exactly the opposite effects were observed.”
Generally, caffeine is considered anti-inflammatory, but coffee is a different question. And, from the data we have to date, it appears as though whether or not habitual coffee consumption is inflammatory or anti-inflammatory is dependent on yet unidentified factors. Certainly, genetics may be the determinant.
The Intersection of Coffee and Genetics
The way that we process and react to coffee is, at least in some part, related to our genes. In Genes to Know About: Caffeine Metabolism, I discuss that a polymorphism of the CYP450 enzyme family determines how quickly we metabolize caffeine. Likewise, there are high-risk genes for developing autoimmune disease (see also Genes to Know About: Celiac Genes and Genes to Know About: MTHFR). In recent studies, two genes have been linked with autoimmune disease and coffee tolerance.
NAT2 polymorphisms. Another key gene that I haven’t had the chance to discuss on the blog yet is polymorphisms of N-acetyltransferase 2 (NAT2) enzyme. This enzyme is involved in the metabolism of xenobiotics (foreign substances that are ingested or otherwise make their way into our bodies), including coffee. Specific polymorphisms lead to a slower acetylation and result in a slower degradation of toxic intermediate molecules. This slower acetylation rate can lead to worsened autoimmune disease processes, and it seems like coffee is no exception. Indeed, people with the NAT2 polymorphism that lead to slower coffee acetylation may have increased risk for autoimmune disease.
HLA genes. Another gene implicated in autoimmune disease is human leukocyte antigen (HLA), which has two haplotypes (I and II). Autoimmune diseases have been linked with haplotype II, which influences CD4+ Th cells (that includes helper T cells and regulatory T cells). Specifically, the autoimmune diseases that have been linked to HLA II include rheumatoid arthritis, type 1 diabetes mellitus, and Grave’s disease. One recent study also demonstrated that coffee consumption increases the risk of autoimmune diabetes of adulthood in people with high-risk HLA genes (specifically those with DR4-DQ8, DR3/4, DR3/3, DR4/4, DR4/3-DQ8, and/or DQA1*0501-DQB1*0201).
So, clearly, the way our bodies are coded is an important concept linking coffee consumption and autoimmune disease.
Coffee and the HPA Axis
 One of the most-noted detrimental effects of consuming caffeine from any source (whether it be coffee, tea, chocolate, or energy drinks) is the effect that it has on cortisol release. Caffeine acts to increase cortisol secretion by elevating production of adrenocorticotropic hormone by the pituitary gland (see How Stress Undermines Health).
One of the most-noted detrimental effects of consuming caffeine from any source (whether it be coffee, tea, chocolate, or energy drinks) is the effect that it has on cortisol release. Caffeine acts to increase cortisol secretion by elevating production of adrenocorticotropic hormone by the pituitary gland (see How Stress Undermines Health).
Excessive cortisol production can lead to a variety of health issues, including an overactive immune system, disrupted sleep, impaired digestion, and depression. When you consume caffeine, your cortisol level increases (dependent on what your cortisol management is like to begin with and how much caffeine you consume) and can stay elevated for up to six hours. With daily consumption, your body will adapt somewhat and not produce quite as much cortisol, but complete tolerance to caffeine does not occur. Very importantly, if you are a habitual consumer of caffeine, your cortisol will increase more dramatically in response to stress (like that guy cutting you off in traffic) than someone who doesn’t consume caffeine. If you have difficult managing stress as it is, caffeine is not helpful to you.
Given the impact that the HPA axis has in overall health, compounding chronic stress with habitual coffee intake may also explain the proinflammatory effects in some people. This evidence certainly makes a case for avoiding coffee if you are experiencing high stress or are at risk for adrenal fatigue (check out my series, Demystifying Adrenal Fatigue, for more information).
A Few More Concerning Effects
One of the reasons for the different responses to coffee is that coffee’s many preparatory strategies (i.e., caffeinated, decaffeinated, boiled, filtered, and so on) can impact its antioxidant content and thus its physiological effects. Several compounds in coffee (namely cafestol and kahweol) have cholesterol-raising effects, and can cause higher LDL and total cholesterol in some individuals (although they may also have a protective effect on the liver, and help explain the association between coffee consumption reduced risk of liver cancer). These compounds are largely removed via paper filtration, so their presence depends on how the coffee is prepared.
A large percentage of people report that coffee upsets their stomach or gives them heartburn. This is because coffee stimulates the secretion of the main gastric hormone gastrin, resulting in excessive secretion of gastric acid and speeding up gastric peristalsis (even decaf coffee has this effect). Coffee also stimulates release of the hormone cholecystokinin (CKK, see The Hormones of Hunger), which stimulates release of bile from the gallbladder (see The Link Between Gallbladder Disease and Gluten Sensitivity and The Paleo Diet for Kidney Disease). In a healthy individual, this release of bile salts is likely sufficient to neutralize the highly acidic chyme. However, deficiencies in gallbladder function are associated with metabolic syndrome. In the case of reduced gallbladder function or excessive coffee consumption, highly acidic chyme travels through the small intestine where it irritates and inflames the lining of the intestines. This is also clearly a good argument for consuming coffee with food.
Also, there is some preliminary evidence that coffee consumption can increase serum homocysteine levels, which indicates a potential concern for anyone with genetic variants in methylation genes (like MTHFR, see Genes to Know About: MTHFR, What The Heck Does Our Liver Do Anyway? Detoxification Explained and The Best Foods and Nutrients to Support Liver Detox) impacting function.
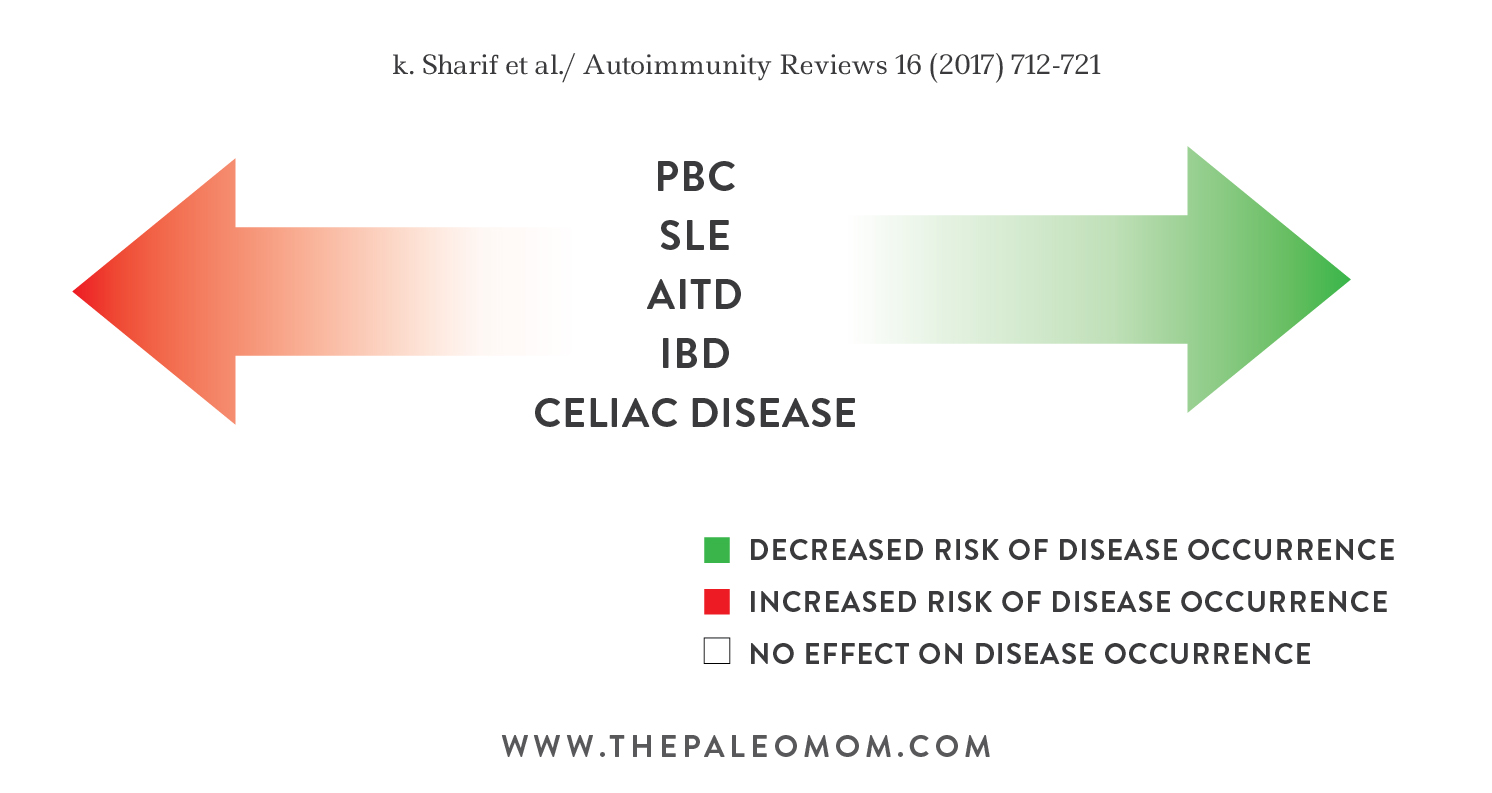
Coffee and Autoimmune Disease Risk by Individual Disease
Like so much research into autoimmune disease, there has thus far been a focus only on the most common autoimmune disease. But, the link between coffee consumption and autoimmune disease risk (and how it differs from one autoimmune disease to another) is super ! Here is a brief breakdown of coffee’s impact on several broad categories of autoimmune disease:
Rheumatoid arthritis.
RA is a painful disorder of the joints that often (like many autoimmune diseases) eludes the medical community. There is some evidence that RA risk is increased in coffee-drinkers, especially people who drink more than 4 cups of coffee a day. Interestingly, one study found more risk for people who drink decaffeinated rather than caffeinated coffee. Importantly, for people who are being managed with methotrexate, caffeine consumption may decrease methotrexate efficacy.
Thyroid autoimmune disease.
The two major thyroid diseases, hyperthyroidism and hypothyroidism, are most likely caused by autoimmune disease. As of now, there is the most evidence surrounding Hashimoto’s thyroiditis, which is the leading cause of hypothyroidism (low thyroid hormone). While we don’t know whether coffee is related to the onset and progression of this disease, we do know that coffee interrupts treatment with levothyroxine: taking this medication with coffee leads to decreased absorption AND longer time to reach peak blood levels. Yikes!
Type 1 diabetes mellitus.
Type 1 diabetes results from autoimmune destruction of beta islet cells in the pancreas, which leads to inadequate insulin secretion. While type 1 diabetes is most commonly developed in childhood and adolescence, there is a growing population of middle aged and elderly people developing this condition (and there is evidence that drinking more than 4 cups per day increases risk for late onset autoimmune diabetes, especially for those with high-risk HLA genes). Coffee consumption in this population seems to be related to disease outcomes. For example, there seems to be a relationship between coffee intake and episodes of hypoglycemia (low blood sugar). There was even a study that demonstrated a 15% reduction in insulin sensitivity among caffeine consumers!! Still, evidence is mixed.
Multiple sclerosis (MS).
MS is a chronic demyelinating disease of the central nervous system that causes progressive neurological deterioration. Interestingly, diets high in coffee are inversely associated with MS development, so coffee consumption may be protective!
Systemic lupus erythematous (SLE).
This autoimmune condition is a chronic multi-system disease that results in autoimmune attacks on areas of the body including the joints, skin, lungs, kidneys, and nervous system. Like many of the other disease we’ve talked about here, there is mixed evidence regarding SLE and coffee. It looks like there may be a dose-dependent relationship, meaning that the more coffee one consumes, the more likely they are to develop SLE.
Liver diseases.
There are three predominant autoimmune liver diseases: autoimmune hepatitis, primary sclerosing cholangitis (PSC), and primary biliary cholangitis (PBC). All three of these diseases result in cirrhosis and liver failure, and much about there pathogeneisis is currently unknown. While there isn’t a ton of evidence here, there is some research showing that coffee may be protective against the development of PSC but not PBC or autoimmune hepatitis.
Inflammatory bowel disease (IBD).
The two major inflammatory bowel diseases, Chrohn’s disease and ulcerative colitis, are both autoimmune in origin and result in an inflamed gastrointestinal tract. Interestingly, there is an inverse association between coffee consumption and IBD.
Celiac disease.
This common autoimmune disease is results in damage to the intestinal tract if a person consumes gluten. Importantly, coffee has been studied as a gluten cross-reactor, so people with Celiac disease may have to cut it out in order to see a resolution of their symptoms. Interestingly, the type of coffee preparation is related to whether the coffee results in a cross-reaction with gluten: espresso, Turkish- and Israeli-style coffee as well as pure coffee is less reactive than instant coffee.
While the above graphic outlines the current evidence linking coffee consumption and autoimmune disease risk, I think it’s important to emphasize that what to do about coffee isn’t as simple as a diagram. For example, if you suffer from multiple sclerosis, that doesn’t automatically mean that coffee will benefit you. I encourage you to think about how to apply these findings to your own body and lifestyle and want to emphasize that there is tremendous value in an elimination and challenge protocol (see The Autoimmune Protocol and Reintroducing Foods after Following the Autoimmune Protocol).
The Bottom Line
Coffee has a clear effect on the immune system, which can increase risk for certain autoimmune diseases. Even for those diseases for which coffee consumption seems to reduce overall risk, that’s no guarantee that coffee will benefit you as an individual–there’s still a chance that your immune system is being stimulated by coffee consumption. Because researchers have yet to conclusively identify the reason why some people experience an anti-inflammatory effect from coffee whereas other experience immune stimulation, the (unfortunate) bottom line is that coffee is still best eliminated in the initial phase of AIP implementation. (Learn more about The Autoimmune Protocol and Reintroducing Foods after Following the Autoimmune Protocol).
Citations
Akashi I, Kagami K, Hirano T, Oka K. Protective effects of coffee-derived compounds on lipopolysaccharide/D-galactosamine induced acute liver injury in rats. J Pharm Pharmacol. 2009 Apr;61(4):473-8. doi: 10.1211/jpp/61.04.0009.
Ata N, et al. “The metabolic syndrome is associated with complicated gallstone disease.” Can J Gastroenterol. 2011 May; 25(5): 274–276.
Aubin HJ & Berlin I. “Re: Coffee Consumption and Mortality From all Causes, Cardiovascular Disease, and Cancer: A Dose-Response Meta-Analysis.” Am J Epidemiol. 2015 May 1;181(9):734-5.
Boekema PJ, et al. “Coffee and Gastrointestinal Function: Facts and Fiction: A Review.” Scand J Gastroenterol Suppl. 1999;230:35-9.
Capek P, Paulovičová E, Matulová M, Mislovičová D, Navarini L, Suggi-Liverani F. Coffea arabica instant coffee–chemical view and immunomodulating properties. Carbohydr Polym. 2014 Mar 15;103:418-26. doi: 10.1016/j.carbpol.2013.12.068. Epub 2014 Jan 3.
Corrêa TA, Rogero MM, Mioto BM, Tarasoutchi D, Tuda VL, César LA, Torres EA. Paper-filtered coffee increases cholesterol and inflammation biomarkers independent of roasting degree: a clinical trial. Nutrition. 2013 Jul-Aug;29(7-8):977-81. doi: 10.1016/j.nut.2013.01.003. Epub 2013 Mar 17.
Crippa A, et al. “Coffee consumption and mortality from all causes, cardiovascular disease, and cancer: a dose-response meta-analysis.” Am J Epidemiol. 2014 Oct 15;180(8):763-75.
Dulson DK, Bishop NC. Effect of a high and low dose of caffeine on human lymphocyte activation in response to antigen stimulation. Appl Physiol Nutr Metab. 2016 Feb;41(2):224-7. doi: 10.1139/apnm-2015-0456. Epub 2015 Oct 29.
Freedman ND, et al. “Association of coffee drinking with total and cause-specific mortality.” N Engl J Med. 2012 May 17;366(20):1891-904.
Gavrieli A, Yannakoulia M, Fragopoulou E, Margaritopoulos D, Chamberland JP, Kaisari P, Kavouras SA, Mantzoros CS. Caffeinated coffee does not acutely affect energy intake, appetite, or inflammation but prevents serum cortisol concentrations from falling in healthy men. J Nutr. 2011 Apr 1;141(4):703-7. doi: 10.3945/jn.110.137323. Epub 2011 Feb 23.
Goto M, Yamaki K, Shinmoto H, Takano-Ishikawa Y. Continuous orally administered coffee enhanced the antigen-specific Th1 response and reduced allergic development in a TCR-transgenic mice model. Biosci Biotechnol Biochem. 2009 Nov;73(11):2439-44. Epub 2009 Nov 7.
Gough SC, Simmonds MJ. The HLA Region and Autoimmune Disease: Associations and Mechanisms of Action. Curr Genomics. 2007;8(7):453-65.
Gunter MJ, et al. “Coffee Drinking and Mortality in 10 European Countries: A Multinational Cohort Study.” Ann Intern Med. 2017 Jul 11. doi: 10.7326/M16-2945.
Horrigan LA, Kelly JP, Connor TJ. Immunomodulatory effects of caffeine: friend or foe?Pharmacol Ther. 2006 Sep;111(3):877-92. Epub 2006 Mar 15. Review.
Kantamala D, Vongsakul M, Satayavivad J. The in vivo and in vitro effects of caffeine on rat immune cells activities: B, T and NK cells. Asian Pac J Allergy Immunol. 1990 Dec;8(2):77-82.
Kiyohara C, Washio M, Horiuchi T, et al. Modifying effect of N-acetyltransferase 2 genotype on the association between systemic lupus erythematosus and consumption of alcohol and caffeine-rich beverages. Arthritis Care Res (Hoboken). 2014;66(7):1048-56.
Lammert C, Juran BD, Schlicht E, et al. Reduced coffee consumption among individuals with primary sclerosing cholangitis but not primary biliary cirrhosis. Clin Gastroenterol Hepatol. 2014;12(9):1562-8.
Lane JD, et al. “Caffeine affects cardiovascular and neuroendocrine activation at work and home.” Psychosom Med. 2002 Jul-Aug;64(4):595-603.
Lane JD, et al. “Caffeine effects on cardiovascular and neuroendocrine responses to acute psychosocial stress and their relationship to level of habitual caffeine consumption.” Psychosom Med. 1990 May-Jun;52(3):320-36.
Lee YH, Bae SC, Song GG. Coffee or tea consumption and the risk of rheumatoid arthritis: a meta-analysis. Clin Rheumatol. 2014;33(11):1575-83.
Loftfield E, Shiels MS, Graubard BI, Katki HA, Chaturvedi AK, Trabert B, Pinto LA, Kemp TJ, Shebl FM, Mayne ST, Wentzensen N, Purdue MP, Hildesheim A, Sinha R, Freedman ND. Associations of Coffee Drinking with Systemic Immune and Inflammatory Markers. Cancer Epidemiol Biomarkers Prev. 2015 Jul;24(7):1052-60. doi: 10.1158/1055-9965.EPI-15-0038-T. Epub 2015 May 21.
Lovallo WR, et al. “Caffeine Stimulation of Cortisol Secretion Across the Waking Hours in Relation to Caffeine Intake Levels.” Psychosom Med. 2005; 67(5): 734–739.
Lovallo WR, et al. “Stress-like adrenocorticotropin responses to caffeine in young healthy men.” Pharmacol Biochem Behav. 1996 Nov;55(3):365-9.
Melamed I, Kark JD, Spirer Z. Coffee and the immune system. Int J Immunopharmacol. 1990;12(1):129-34.
Muqaku B, Tahir A, Klepeisz P, Bileck A, Kreutz D, Mayer RL, Meier SM, Gerner M, Schmetterer K, Gerner C. Coffee consumption modulates inflammatory processes in an individual fashion. Mol Nutr Food Res. 2016 Dec;60(12):2529-2541. doi: 10.1002/mnfr.201600328. Epub 2016 Aug 30.
Muscat S, Pelka J, Hegele J, Weigle B, Münch G, Pischetsrieder M. Coffee and Maillard products activate NF-kappaB in macrophages via H2O2 production. Mol Nutr Food Res. 2007 May;51(5):525-35.
Park S-Y, et al. “Association of Coffee Consumption With Total and Cause-Specific Mortality Among Nonwhite Populations.” Ann Intern Med. 2017 Jul 11. doi: 10.7326/M16-2472.
Passos CP, Cepeda MR, Ferreira SS, Nunes FM, Evtuguin DV, Madureira P, Vilanova M, Coimbra MA. Influence of molecular weight on in vitro immunostimulatory properties of instant coffee. Food Chem. 2014 Oct 15;161:60-6. doi: 10.1016/j.foodchem.2014.03.119. Epub 2014 Apr 2.
Rasouli B, Ahlqvist E, Alfredsson L, et al. Coffee consumption, genetic susceptibility and risk of latent autoimmune diabetes in adults: A population-based case-control study. Diabetes Metab. 2018;44(4):354-360.
Rebello SA, Chen CH, Naidoo N, Xu W, Lee J, Chia KS, Tai ES, van Dam RM. Coffee and tea consumption in relation to inflammation and basal glucose metabolism in a multi-ethnic Asian population: a cross-sectional study. Nutr J. 2011 Jun 2;10:61. doi: 10.1186/1475-2891-10-61.
Sauer T, Raithel M, Kressel J, Muscat S, Münch G, Pischetsrieder M. Nuclear translocation of NF-κB in intact human gut tissue upon stimulation with coffee and roasting products. Food Funct. 2011 Sep;2(9):529-40. doi: 10.1039/c1fo10055f. Epub 2011 Sep 9.
Sharif K, Watad A, Bragazzi NL, Adawi M, Amital H, Shoenfeld Y. Coffee and autoimmunity: More than a mere hot beverage!. Autoimmun Rev. 2017;16(7):712-721.
Simões J, Madureira P, Nunes FM, Domingues Mdo R, Vilanova M, Coimbra MA. Immunostimulatory properties of coffee mannans. Mol Nutr Food Res. 2009 Aug;53(8):1036-43. doi: 10.1002/mnfr.200800385.
Tuomilehto J, Tuomilehto-wolf E, Virtala E, Laporte R. Coffee consumption as trigger for insulin dependent diabetes mellitus in childhood. BMJ. 1990;300(6725):642-3.
Wijnands JM, Kingwell E. Time to wake up and smell the coffee? Coffee consumption and multiple sclerosis. J Neurol Neurosurg Psychiatry. 2016;87(5):453.
Zampelas A, Panagiotakos DB, Pitsavos C, Chrysohoou C, Stefanadis C. Associations between coffee consumption and inflammatory markers in healthy persons: the ATTICA study. Am J Clin Nutr. 2004 Oct;80(4):862-7.