A pervasive and harmful myth that has been circulating is that there’s no science to support wearing facemasks to reduce the spread of covid-19. Let’s bust this one right now because wearing a facemask, even a homemade one, is one of the best things we can do to limit the spread of the novel coronavirus as well as other respiratory infections, like influenza. Other high-priority action items include social distancing—maintaining a minimum 6-foot (2-meter) distance between yourself and others—and prudent and proper handwashing—lathering vigorously for a full 20 seconds, rinsing for 10 seconds, and washing hands upon returning home, before eating, after using the bathroom, and any time you touch something that may be contaminated.
Let’s first agree that reducing the spread of covid-19 is important! As of 6-25-20, there have been almost 9.5 million confirmed cases globally and over 480,000 deaths. (Almost exactly a quarter of the global cases and deaths are/were in the USA, which also saw its highest single-day new cases on 6-24-20 as case numbers continue to accelerate in at least half of the country.) While many experts estimate that we’re undercounting cases by about a factor of 10 (due to testing availability, testing limitations, and asymptomatic/mild infections), even in that best-case scenario (assuming 10 times more mild cases), we’re still talking about a mortality rate in the neighborhood of 0.5%. That’s not just bad because it’s 1 in 200 people, a mortality rate that’s 5 times higher than the seasonal flu, but because this is a novel [meaning new] coronavirus, we’ve never encountered it before, so nobody had prior immunity. That means that this virus can spread more easily, infecting a much broader swath of the population than the seasonal flu (in which many people have at least partial immunity thanks having had flu recently or getting the annual flu shot). This means that many more people could die from covid-19 than just five times the seasonal flu number. And, there’s another big problem: with such a large proportion of covid-19 sufferers requiring hospitalization and ICU care, unimpeded spread of covid-19 risks overwhelming the healthcare system entirely. That not only poses a problem for covid-19 sufferers requiring advanced medical care, but for anyone facing a medical emergency during this pandemic, for example a stroke, heart attack, or severe car accident. And, while there have been some advances in treatment of the severe pneumonia and Acute Respiratory Distress Syndrome that occurs in a subset of those infected with the novel coronavirus, we still don’t have the necessary effective treatment options or preventatives required for life to safely return to normal.
To understand the benefits of all of us wearing masks during this global pandemic, we need to examine how SARS-CoV-2 (the virus that causes covid-19) spreads from person to person, how SARS-CoV-2 infects our cells, how fabrics compare to medical-grade masks to block that spread, and why even imperfect masks are a vast improvement to no mask at all. While we’re at it, we’ll bust some other myths about masks, like safety concerns.
Save 80% Off the Foundations of Health
Expand your health knowledge on a wide range of topics relevant to you, from how to evaluate scientific studies, to therapeutic diet and lifestyle, to leaky gut and gut microbiome health, to sustainable weight loss, and much more!!!

Transmission of SARS-CoV-2
 The primary mode of transmission of the SARS-CoV-2 virus (the novel coronavirus that causes the covid-19 illness) is what’s called respiratory droplets. These teeny tiny drops of saliva and mucus are expelled from our mouth and nose not only when we cough or sneeze, but even when we breath heavily or speak. The louder we talk (like speaking in front of an audience or singing) or the worse the cough, the farther these droplets can be expelled. Respiratory droplets range in size but can be so small that they can remain suspended in the air for hours, depending on droplet size, humidity and airflow.
The primary mode of transmission of the SARS-CoV-2 virus (the novel coronavirus that causes the covid-19 illness) is what’s called respiratory droplets. These teeny tiny drops of saliva and mucus are expelled from our mouth and nose not only when we cough or sneeze, but even when we breath heavily or speak. The louder we talk (like speaking in front of an audience or singing) or the worse the cough, the farther these droplets can be expelled. Respiratory droplets range in size but can be so small that they can remain suspended in the air for hours, depending on droplet size, humidity and airflow.
Respiratory droplets are an excellent vector for respiratory viruses like SARS-CoV-2. Studies of the novel coronavirus show that it remains viable (i.e., infectious) in an aerosol (equivalent to a very small respiratory droplet, technically called respiratory droplet nuclei) for at least three hours. These facts have some researchers calling the 6-foot (2-meter) social distancing guidelines into question as insufficient, especially in indoor environments with limited airflow, where there’s evidence that the virus could be transmittable over much greater distances. In fact, some researchers have proposed that the 6-foot guidelines are only sufficient indoors if people also wear masks, and that in the absence of masks, 30 feet (10 meters) is a safer distance to maintain!
Current estimates are that somewhere between 20% and 80% of covid-19 infections are asymptomatic, meaning the infected person has absolutely no symptoms and generally no way of knowing they’re infected in the absence of broad testing programs. And, people with asymtomatic infection are still contagious, shedding virus for an average of 19 (!) days! In addition, in those people who do develop symptoms, viral load (the amount of virus in their body, more on this below) is highest the day before symptoms start, so we’re most infectious before we even suspect that we’re sick. This is in contrast to previous coronaviruses, including SARS and MERs. For example, people infected with SARS-CoV-1 (the related coronavirus responsible for SARS epidemics in 2002 and 2003) did not shed virus until 24 to 36 hours after symptom onset, which made it vastly easier to contain the virus because people could be isolated before transmitting the virus to others (a major reason why less than 800 people died from SARS over two years globally despite a higher mortality rate than covid-19). The fact that SARS-CoV-2 is most contagious before symptoms start is one of the reasons why containment efforts have failed in most countries (along with insufficient testing capabilities).
Inoculation with SARS-CoV-2
When a respiratory droplet containing SARS-CoV-2 enters your mouth or nose, it’s easily inhaled into your airway where it encounters pulmonary cells that have ACE2 enzymes embedded within their surface membranes. (ACE2 is a type I transmembrane metallocarboxypeptidase that degrades angiotensin-2, thereby negatively regulating the renin-angiotensin system to lower blood pressure. ACE2’s role in regulating blood pressure is why hypertension is such a major risk factor for a more severe course of covid-19 illness. ACE2 is also found in arteries, heart, kidney, and intestines.) The now infamous spike proteins on the outside of SARS-CoV-2 bind with ACE2, releasing the fusion machinery that the virus uses to dump its RNA and viral proteins into the target cell, where it hijacks the cells organelles to produce viral replicas instead of all of the various proteins that the cell needs to survive. Within about 10 hours, the infected cell can produce hundreds of virus copies that are released via exocytosis, typically killing the infected cell in the process. Some of those viral particles go on to infect neighboring cells, while others are expelled in respiratory droplets to spread to new hosts.
A few things to know…
First, viral load, meaning the number of viral particles measurable in your body (typically serum) strongly correlates with covid-19 disease severity. Viral load isn’t the only contributor to disease severity, but on balance, the more viruses in your body, the sicker you are (and with covid-19, the higher the mortality rate).
Second, high viral load generally increases virus shedding, meaning that you’re more contagious if you have a high viral load than a low viral load because your body is expelling more virus.
Third, SARS-CoV-2 has some pretty ingenious ways that it can evade detection by our immune systems (blocking interferon secretion and antigen presentation by major histocompatibility complex class II molecules), at least until it has had a good headstart replicating itself.
And fourth, it takes the adaptive immune system (the part of your immune system that can target a specific antigen, and hence cause less bystander damage to healthy human cells while being more effective at fighting off an infectious organism) at least 3 days to start ramping up a response and at least a week to be fully activated.
Okay, so what happens if you’re exposed to only a few viral particles versus tons of them? This is known as the inoculation dose, the amount of virus particles you’re initially exposed to when you become infected. (In contrast, the infectious dose is the minimum number of viral particles required to make you sick, also relevant to this discussion.) If every virus can make a few hundred copies of itself by hijacking our cellular machinery every 10 hours or so, it’s easy to see how much more quickly viral load can skyrocket if the inoculation dose is high versus low. That also means that, by the time the adaptive immune system is engaged, the job is way bigger because there’s way more viral particles and way more infected cells. Of note, immune overactivation is the major driver of Acute Respiratory Distress Syndrome, the major complication causing death from covid-19.
Not surprisingly, inoculation dose is a strong predictor of disease severity, compounded with other risk factors, including: pre-existing conditions (like high blood pressure, diabetes, cardiovascular disease, and cancer), age (especially being over 65), and genetics (in particular the ApoE4/4 genotype). While it’s no guarantee of a mild disease course, it’s definitely far preferable if we’re going to be exposed to SARS-CoV-2 to minimize the inoculation dose.

The Science of Homemade Masks
Facemasks provide a physical barrier that traps the majority of respiratory droplets exhaled by infected people as well as working to reduce the probability of inhaling respiratory droplets containing viral particles by healthy people. That’s why surgeons and surgical staff wear facemasks as one component of their personal protective equipment (PPE) to protect the patient from wound infection and contamination from the operating team, as well as to protect the operating team from airborne infections originating from the patient.
But how do homemade cloth masks compare to surgical masks or that epitome of filtration, the N95 respirator mask?
Homemade facemasks have been studied for their filtration efficiency. For example, a 2013 study tested how well homemade masks made with various materials could filter aerosols containing Bacillus atrophaeus. Depending on the material used and whether it was a single or double layer, well-fitted homemade masks filtered between 58% and 97% compared to a surgical mask’s 96%. The same study found that mask fit was also a big factor in how well they protect against respiratory droplet transmission, which makes a ton of sense. If too much air can leak out the sides of a poorly-fitted mask, the filtration efficiency becomes less relevant. And, while the surgical mask was better at reducing the number of microorganisms expelled during coughing (especially with the lowest respiratory droplet size), the homemade mask still offered significant protection compared to no mask, blocking between 60% and 85% of respiratory droplets, depending on the droplet size.
| Mean % Filtration Efficiency | |
| Tea towel – double layer | 97 % |
| Vacuum cleaner bag | 94 % |
| Cotton mix – single layer | 75 % |
| 100% cotton T-shirt – double layer | 71 % |
| Scarf – single layer | 62 % |
| Pillowcase – double layer | 62 % |
| Silk – single layer | 58 % |
*Adapted from Davies A, Thompson KA, Giri K, Kafatos G, Walker J, Bennett A. Testing the efficacy of homemade masks: would they protect in an influenza pandemic? Disaster Med Public Health Prep. 2013 Aug;7(4):413-8. doi: 10.1017/dmp.2013.43.
A 2020 study also evaluated the filtration efficiency of various fabrics for homemade masks, comparing to both surgical masks and N95 masks. While filtration efficiency ranged from 9% to 99%, the study found lots of great options for homemade masks, with the best performing being those well-fitted masks made from multiple layers of mixed fabric types.
| Mean % Filtration Efficience <300nm | Mean % Filtration Efficience >300nm | |
| N95 mask | 85 % | 99.9 % |
| Surgical mask | 76 % | 99.6 % |
| 1 layer of 600 TPI cotton and 2 layers of chiffon | 97 % | 99 % |
| 1 layer of 600 TPI cotton and 2 layers of silk | 94 % | 99 % |
| 1 layer of 600 TPI cotton and 1 layer of flannel | 95 % | 96 % |
| 2 layers of 600TPI cotton | 82 % | 99.5 % |
| 2 layers of chiffon | 83 % | 90 % |
| 4 layers of natural silk | 86 % | 88 % |
*Adapted from Konda A, Prakash A, Moss GA, Schmoldt M, Grant GD, Guha S. ACS Nano. Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks. 2020 May 26;14(5):6339-6347. doi: 10.1021/acsnano.0c03252.
Which design of facemask is best? Are elastic earloops better than ties? When it comes to mask design, what matters is how it fits. Facemasks should be large enough to reach the bridge of the nose, all the way to the edge of the face on the side and under the edge of the chin. The mask should fit snugly around the contours of the face, with no gaps, but should still feel comfortable. While wearing, you should be able to breath easily through the mask. A nosepiece can help the mask fit better over the nose, while blocking hot exhaled air from leaking out the top edge, which is what fogs up glasses.
 The usefulness of facemasks for reducing respiratory infections in humans has been studied. For example, a 2010 study of over 1400 college students living in dorms, showed that the combination of wearing a medical procedure facemask plus handwashing decreased the risk of an influenza-like illness by about 50% after 6 weeks during flu season. In a 2009 study of parents looking after their sick children, wearing a surgical mask and handwashing within 3 days of the child’s symptom onset reduced likelihood of the parent catching an influenza-like illness by about 70%.
The usefulness of facemasks for reducing respiratory infections in humans has been studied. For example, a 2010 study of over 1400 college students living in dorms, showed that the combination of wearing a medical procedure facemask plus handwashing decreased the risk of an influenza-like illness by about 50% after 6 weeks during flu season. In a 2009 study of parents looking after their sick children, wearing a surgical mask and handwashing within 3 days of the child’s symptom onset reduced likelihood of the parent catching an influenza-like illness by about 70%.
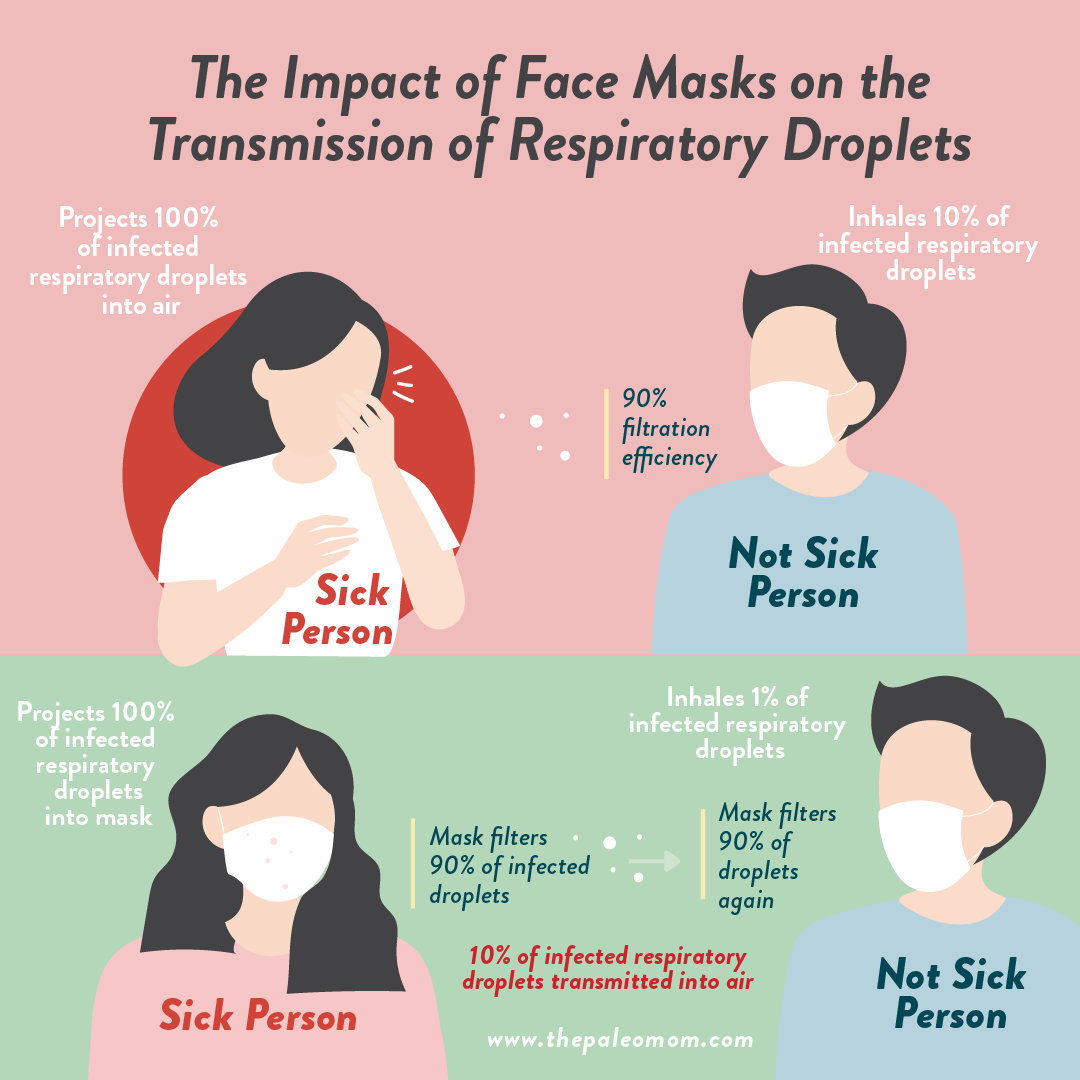
As you can likely deduce, the most protection comes from everyone wearing a mask, because it means the virus must cross two physical barriers in order to travel from an infected person to a healthy person.
Let’s do some back-of-the-envelope math. Let’s consider a scenario where an infected person is talking right into the mouth of a healthy person, so 100% of their respiratory droplets are being inhaled by the healthy person. If you put a well-fitted mask that has a 90% filtration efficiency on the sick person’s face, 10% of the respiratory droplets will pass through to be inhaled by the healthy person. Now, put a 90% filtration efficiency mask on both of our hypothetical close-talkers. That second mask filters 90% of the 10% that makes it through the first mask, so in this scenario, the healthy person is only breathing in 1% of the respiratory droplets. Add some respect for personal space and airflow into the equation, and there’s a much greater chance that the healthy person doesn’t even get exposed to an infectious dose (the minimum dose required to make the person sick). Even if they do get exposed to an infectious dose, the inoculation dose has been greatly reduced, lowering the risk of severe infection. YAY FOR MASKS!
And in fact, a 2020 systematic review of covid-19, SARS and MERS showed that facemasks are very effective at reducing transmission, and not surprisingly, the strongest association, an 85% reduction in transmission, was with N95 or other similar respirator use.
So, Why Isn’t Everyone Wearing a Mask?
While polls show that the vast majority of Americans think masks are a-o-k (and, for example, don’t feel judged negatively for wearing one), the majority of people still aren’t wearing them most of the time. An April Gallup poll showed that 36% of American adults wear a mask at all times outside the home, 32% wear a mask sometimes outside the home, and 31% (!) never wear a mask.
 Studies have long shown facemask compliance to be an issue. For example, in a 2010 study evaluating the benefit of surgical masks for reducing household spread of influenza, 75% of participants reported discomfort with mask use, 45% of which found the masks too warm, 33% felt they had trouble breathing (as we’ll discuss in the next paragraph, they weren’t actually having trouble breathing), and the rest found the facemask to be too humid. In a similar 2009 study, less than 30% of the participants were still wearing their facemasks most of the time by day 5 (not that the participants started out with high compliance, it was less than 50% on day 1!). In fact, in both of these studies, the authors concluded that facemasks were ineffective at reducing influenza-like illness attributable purely to low compliance. It turns out that facemasks are pretty useless at reducing infection if we don’t wear them.
Studies have long shown facemask compliance to be an issue. For example, in a 2010 study evaluating the benefit of surgical masks for reducing household spread of influenza, 75% of participants reported discomfort with mask use, 45% of which found the masks too warm, 33% felt they had trouble breathing (as we’ll discuss in the next paragraph, they weren’t actually having trouble breathing), and the rest found the facemask to be too humid. In a similar 2009 study, less than 30% of the participants were still wearing their facemasks most of the time by day 5 (not that the participants started out with high compliance, it was less than 50% on day 1!). In fact, in both of these studies, the authors concluded that facemasks were ineffective at reducing influenza-like illness attributable purely to low compliance. It turns out that facemasks are pretty useless at reducing infection if we don’t wear them.
Yes, many people don’t find masks to be comfortable, especially when they aren’t used to wearing them. You can improve the comfort of your mask by making sure it fits properly, and as medial professionals can attest to, you do get used to it over time. Like most things worth pursuing, practice makes perfect.
There’s also some rumors circulating the internet that are deterring people from wearing masks, one of the most pervasive of which is that wearing a mask all day will give you CO2 poisoning, also known as hypercapnia. This is not supported by the science. A 2010 study evaluated the physiological effects of wearing an N95 (with or without a valve) while walking on a treadmill in 10 healthcare workers. Compared to not wearing a mask, wearing an N95 mask while walking 2.5 miles per hour for one hour did not change the participants’ oxygen saturation (SpO2 was 98.5 in control versus 98.4 with respirator) nor did it change their partial pressure of CO2 (PtcCO2 was 40.8 in control versus 42.0 with respirator, which is still normal and within the margin of error, so not statistically different). Because when you’re wearing an N95 mask, you do need to breathe harder, there is an increase in metabolism while wearing it, as shown in a 2015 study in pregnant women (again no hypoxia or hypercapnia with N95 use, nor any risk to the mom or fetus). So, it has long been advised that people with health conditions that cause hypoxia and hypercapnia, like COPD, avoid prolonged use of N95 type respirator masks. However, a 2020 study of N95 facemask use in people with COPD found that only 7 out of 97 participants did not tolerate the mask (these were the participants with the lowest pulmonary function to begin with), but they still experienced only very small changes to O2 saturation (from 96.4 to 94.9, statistically significant) and exhaled carbon dioxide (ETCO2 went from 24.8 to 29.7, a trend but not a statistically significant change). The other 90 participants experienced no change to O2 saturation or exhaled CO2. So no, wearing a homemade cloth mask all day will not cause hypercapnia nor hypoxia, even in people with predisposition due to pulmonary disease.
Is there anyone who shouldn’t wear a mask? The CDC recommends not putting masks on children below the age of 2, nor anyone who has trouble breathing (without a mask on!), or is unconscious, incapacitated or otherwise unable to remove the mask without assistance. Quite frankly, it would be unethical to test whether a facemask causes hypercapnia in babies and incapacitated people, so in the absence of data, caution is the better part of valor.
The fact is that wearing a mask, whether or not you feel it is uncomfortable, and whether or not you are personally concerned about covid-19, is one of the best ways that you can contribute to reducing the spread of covid-19 and protecting the vulnerable in our communities. But, for it to work, everyone needs to wear a facemask, because it means that the virus must cross two physical barriers in order to go from the infected person to the healthy person. Remember that you are contagious before symptoms start, and that while older people with pre-existing conditions are in a higher risk category, the data has shown us that no one is exempt from a severe or even deadly course of covid-19. Even if you are not concerned about covid-19 personally, consider those of us at higher risk. You might have a mild or even asymptomatic disease course, but the people you infect may not be so lucky. So, on behalf of high-risk people everywhere, I thank you for sticking with that mask, even through the summer heat and humidity.
How to Wear a Mask
I hope you’re convinced that wearing a mask is important, so let’s wrap up with when, where and how to wear one.
Let’s start with when and where.
Best practice is to wear a mask at all times indoors when not in your home; that includes at work, at school, at the store (any store), at places of worship, at community centers, and at the gym. You may wish to also wear a mask in your home if you live with someone who works outside the home in a high-risk environment, such as a hospital or long-term care facility, or conversely, if you work outside the home and want to protect an at-risk family member or roommate. When outdoors in an area where you can not socially distance (a narrow sidewalk or crowded park or beach, for example), mask use is also prudent.
Why is it okay to skip the mask outside when you’re far away from people? A 2020 study calculated that 11 to 34 minutes of midday sunlight in most cities during the summer is sufficient to deactivate 90% or more of aerosolized SARS-CoV-2. (Basically, the stronger the UV radiation, the less time it takes to deactivate the virus, so that’s a function of time of day, time of year, latitude and weather.) This study didn’t take into account dispersal from airflow, which also reduces the likelihood of exposure. So, if you’re going for a neighborhood walk, for example, and able to maintain social distance, your risk of exposure is extremely low.
If you aren’t concerned about catching covid-19 yourself and are purely wearing a mask to protect others (you rock!), all you need to do is make sure you’re wearing a mask that is made of at least two layers of a tight-weave fabric, that fits snugly, and that completely covers your entire nose and mouth. You can wear the same mask day after day, and only wash it or swap it out when it gets funky. Why have you seen public health officials giving briefings with a mask below their nose and only covering their mouth? When you project your voice (think public speaking, lecturing, teaching, stage performing, singing, etc.), respiratory droplets are expelled with more force from the mouth, but not the nose. Those public health officials are at least 6 feet away from their audience, but still wearing a mask over their mouth to protect the people they’re speaking to because their respiratory droplets are traveling farther while they’re speaking loudly. The only time when it’s okay to wear a mask below the nose is when you’re also socially distancing, and even then, best practice is to wear the mask over both nose and mouth.
 If, on the other hand, you’re wearing a mask to protect yourself, there’s a little more to it.
If, on the other hand, you’re wearing a mask to protect yourself, there’s a little more to it.
First, it’s really, really, really important not to fiddle with the mask. Early on, when public health officials were debating mask policies for the USA, one major point of contention was the increased risk of infection if people wearing masks end up touching their faces more often because they aren’t used to the feeling of the mask. When out and about, the no-touching-your-face rule still applies when you have a mask on. Making sure your mask fits well but isn’t too tight is the best thing you can do to resist the urge to adjust it.
Second, it’s important to treat the outside of the mask as contaminated. When you remove your mask, do so without smearing it over your nose and mouth. Think of how a doctor removes their mask. Hold the mask in place with one hand while untying it or unhooking earloops with the other hand; then pull the mask straight away your face. Throw the mask immediately in the laundry (yes, wash after every use), and then wash your hands thoroughly. If you aren’t near a sink and want to remove your mask (for example, if you’ve returned to your car after grocery shopping and don’t want to wear the mask for the entire drive home), you can wear latex or nitrile disposable gloves to remove the mask, stuff it in a plastic bag, toss the gloves (removing them by flipping them inside out so you aren’t touching the outside of the glove with your ungloved hand), and then use alcohol-based hand sanitizer (using enough that it takes a full minute of rubbing hands together before it’s fully evaporated). Safe mask removal is a skill that medical professionals and researchers develop, but it does take some conscientiousness if wearing masks and gloves are not yet old hat for you.
Are Masks Our New Normal?
Maybe. We’re learning the value of mask-wearing by the public to limit the spread of a pandemic serious respiratory illness. We still don’t know if covid-19 will be like the seasonal flu—spiking every winter, and mutating with enough frequency that we need annual vaccines that have to predict the dominant strain but don’t always get it right—or like chicken pox or roseola where once you’ve had it, you’re immune for life (unless you’re immunocompromised, of course). Or perhaps covid-19 could be like meningococcal disease or tetanus, where our immunologic memory only lasts a few years. If covid-19 is like the seasonal flu or meningitis, mask-wearing during “covid season” is likely to become our new normal. But, even if covid-19 is more like the vast collection of childhood diseases that we only ever get once, shifting our culture towards facemasks as business-as-usual could reduce mortality from not just covid-19 but plenty of other respiratory infections, including the seasonal flu, which kills tens of thousands of people annually. And, it would mean that we’re better prepared in the event that the future challenges us with yet another novel pandemic virus.
Citations
Aiello AE, Murray GF, Perez V, Coulborn RM, Davis BM, Uddin M, Shay DK, Waterman SH, Monto AS. Mask use, hand hygiene, and seasonal influenza-like illness among young adults: a randomized intervention trial. J Infect Dis. 2010 Feb 15;201(4):491-8. doi: 10.1086/650396.
Bae S, Kim MC, Kim JY, Cha HH, Lim JS, Jung J, Kim MJ, Oh DK, Lee MK, Choi SH, Sung M, Hong SB, Chung JW, Kim SH. Notice of Retraction: Effectiveness of Surgical and Cotton Masks in Blocking SARS-CoV-2: A Controlled Comparison in 4 Patients. Ann Intern Med. 2020 Jun 2;L20-0745. doi: 10.7326/L20-0745.
Brienen NC, Timen A, Wallinga J, van Steenbergen JE, Teunis PF. Risk Anal. The effect of mask use on the spread of influenza during a pandemic. 2010 Aug;30(8):1210-8. doi: 10.1111/j.1539-6924.2010.01428.x.
Canini L, Andréoletti L, Ferrari P, D’Angelo R, Blanchon T, Lemaitre M, Filleul L, Ferry JP, Desmaizieres M, Smadja S, Valleron AJ, Carrat F. Surgical mask to prevent influenza transmission in households: a cluster randomized trial. PLoS One. 2010 Nov 17;5(11):e13998. doi: 10.1371/journal.pone.0013998.
Cheng KK, Lam TH, Leung CC. Wearing face masks in the community during the COVID-19 pandemic: altruism and solidarity. Lancet. 2020 Apr 16:S0140-6736(20)30918-1. doi: 10.1016/S0140-6736(20)30918-1.
Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ; COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020 Jun 1:S0140-6736(20)31142-9. doi: 10.1016/S0140-6736(20)31142-9.
Cowling BJ, Chan KH, Fang VJ, Cheng CK, Fung RO, Wai W, Sin J, Seto WH, Yung R, Chu DW, Chiu BC, Lee PW, Chiu MC, Lee HC, Uyeki TM, Houck PM, Peiris JS, Leung GM. Facemasks and hand hygiene to prevent influenza transmission in households: a cluster randomized trial. Ann Intern Med. 2009 Oct 6;151(7):437-46. doi: 10.7326/0003-4819-151-7-200910060-00142.
Davies A, Thompson KA, Giri K, Kafatos G, Walker J, Bennett A. Testing the efficacy of homemade masks: would they protect in an influenza pandemic? Disaster Med Public Health Prep. 2013 Aug;7(4):413-8. doi: 10.1017/dmp.2013.43.
Eikenberry SE, Mancuso M, Iboi E, Phan T, Eikenberry K, Kuang Y, Kostelich E, Gumel AB. To mask or not to mask: Modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect Dis Model. 2020 Apr 21;5:293-308. doi: 10.1016/j.idm.2020.04.001.
He X, Lau EHY, Wu P, Deng X, Wang J, Hao X, Lau YC, Wong JY, Guan Y, Tan X, Mo X, Chen Y, Liao B, Chen W, Hu F, Zhang Q, Zhong M, Wu Y, Zhao L, Zhang F, Cowling BJ, Li F, Leung GM. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020 May;26(5):672-675. doi: 10.1038/s41591-020-0869-5.
Howard, J.; Huang, A.; Li, Z.; Tufekci, Z.; Zdimal, V.; van der Westhuizen, H.; von Delft, A.; Price, A.; Fridman, L.; Tang, L.; Tang, V.; Watson, G.L.; Bax, C.E.; Shaikh, R.; Questier, F.; Hernandez, D.; Chu, L.F.; Ramirez, C.M.; Rimoin, A.W. Face Masks Against COVID-19: An Evidence Review. Preprints 2020, 2020040203 (doi: 10.20944/preprints202004.0203.v1).
Konda A, Prakash A, Moss GA, Schmoldt M, Grant GD, Guha S. ACS Nano. Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks. 2020 May 26;14(5):6339-6347. doi: 10.1021/acsnano.0c03252.
Kyung SY, Kim Y, Hwang H, Park JW, Jeong SH. Risks of N95 Face Mask Use in Subjects With COPD. Respir Care. 2020 May;65(5):658-664. doi: 10.4187/respcare.06713.
Liu Y, Yan LM, Wan L, Xiang TX, Le A, Liu JM, Peiris M, Poon LLM, Zhang W. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect Dis. 2020 Jun;20(6):656-657. doi: 10.1016/S1473-3099(20)30232-2.
MacIntyre CR, Cauchemez S, Dwyer DE, Seale H, Cheung P, Browne G, Fasher M, Wood J, Gao Z, Booy R, Ferguson N. Emerg Infect Dis. Face mask use and control of respiratory virus transmission in households. 2009 Feb;15(2):233-41. doi: 10.3201/eid1502.081167.
MacIntyre CR, Wang Q. Physical distancing, face masks, and eye protection for prevention of COVID-19. Lancet. 2020 Jun 1:S0140-6736(20)31183-1. doi: 10.1016/S0140-6736(20)31183-1.
Patterson EI, Prince T, Anderson ER, Casas-Sanchez A, Smith SL, Cansado-Utrilla C, Turtle L, Hughes GL. Methods of inactivation of SARS-CoV-2 for downstream biological assays. bioRxiv. 2020 May 23:2020.05.21.108035. doi: 10.1101/2020.05.21.108035.
Roberge RJ, Coca A, Williams WJ, Palmiero AJ, Powell JB. Surgical mask placement over N95 filtering facepiece respirators: physiological effects on healthcare workers. Respirology. 2010 Apr;15(3):516-21. doi: 10.1111/j.1440-1843.2010.01713.x.
Roberge RJ, Coca A, Williams WJ, Powell JB, Palmiero AJ. Physiological impact of the N95 filtering facepiece respirator on healthcare workers. Respir Care. 2010 May;55(5):569-77.
Sagripanti JL, Lytle CD. Estimated Inactivation of Coronaviruses by Solar Radiation With Special Reference to COVID-19. Photochem Photobiol. 2020 Jun 5:10.1111/php.13293. doi: 10.1111/php.13293.
Sehra ST, Salciccioli JD, Wiebe DJ, Fundin S, Baker JF. Maximum Daily Temperature, Precipitation, Ultra-Violet Light and Rates of Transmission of SARS-Cov-2 in the United States. Clin Infect Dis. 2020 May 30:ciaa681. doi: 10.1093/cid/ciaa681.
Setti L, Passarini F, De Gennaro G, Barbieri P, Perrone MG, Borelli M, Palmisani J, Di Gilio A, Piscitelli P, Miani A. Airborne Transmission Route of COVID-19: Why 2 Meters/6 Feet of Inter-Personal Distance Could Not Be Enough. Int J Environ Res Public Health. 2020 Apr 23;17(8):2932. doi: 10.3390/ijerph17082932.
Setti L, Passarini F, De Gennaro G, Barbieri P, Perrone MG, Borelli M, Palmisani J, Di Gilio A, Piscitelli P, Miani A. Airborne Transmission Route of COVID-19: Why 2 Meters/6 Feet of Inter-Personal Distance Could Not Be Enough. Int J Environ Res Public Health. 2020 Apr 23;17(8):2932. doi: 10.3390/ijerph17082932.
To KK, Tsang OT, Leung WS, Tam AR, Wu TC, Lung DC, Yip CC, Cai JP, Chan JM, Chik TS, Lau DP, Choi CY, Chen LL, Chan WM, Chan KH, Ip JD, Ng AC, Poon RW, Luo CT, Cheng VC, Chan JF, Hung IF, Chen Z, Chen H, Yuen KY. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020 May;20(5):565-574. doi: 10.1016/S1473-3099(20)30196-1.
Tong PS, Kale AS, Ng K, Loke AP, Choolani MA, Lim CL, Chan YH, Chong YS, Tambyah PA, Yong EL. Respiratory consequences of N95-type Mask usage in pregnant healthcare workers-a controlled clinical study. Antimicrob Resist Infect Control. 2015 Nov 16;4:48. doi: 10.1186/s13756-015-0086-z.
van der Sande M, Teunis P, Sabel R. Professional and home-made face masks reduce exposure to respiratory infections among the general population. PLoS One. 2008 Jul 9;3(7):e2618. doi: 10.1371/journal.pone.0002618.
van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloyd-Smith JO, de Wit E, Munster VJ. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med. 2020 Apr 16;382(16):1564-1567. doi: 10.1056/NEJMc2004973.
Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA, Niemeyer D, Jones TC, Vollmar P, Rothe C, Hoelscher M, Bleicker T, Brünink S, Schneider J, Ehmann R, Zwirglmaier K, Drosten C, Wendtner C. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020 May;581(7809):465-469. doi: 10.1038/s41586-020-2196-x.
Wood ME, Stockwell RE, Johnson GR, Ramsay KA, Sherrard LJ, Jabbour N, Ballard E, O’Rourke P, Kidd TJ, Wainwright CE, Knibbs LD, Sly PD, Morawska L, Bell SC. Face Masks and Cough Etiquette Reduce the Cough Aerosol Concentration of Pseudomonas aeruginosa in People with Cystic Fibrosis. Am J Respir Crit Care Med. 2018 Feb 1;197(3):348-355. doi: 10.1164/rccm.201707-1457OC.