In Part 1 and Part 2 of this healthy weight loss series, I shared the scientific foundation for diet and lifestyle changes that promote healthy and sustainable weight loss. In an ideal world, we should be able to implement these changes and lose weight with (relative) ease. Yet, I know that the equation is actually a lot more complicated! Indeed, there are many different factors that might interfere with our ability to reach our weight loss goals.
Table of Contents[Hide][Show]
Weight loss resistance is a very common problem that a lot of people struggle with (myself included!). In Parts 1 and 2, we detailed all of the conditions that must be met before someone can lose weight. Namely, we need our bodies to be in a relaxed state, micronutrient sufficient, and able to burn enough calories to utilize our stored fat. However, there are many different potential underlying issues that can stall weight loss, or we might just be facing psychological struggles that prevent us from getting done what we need to. So for this post, I’ve taken an in-depth review of the literature to make a comprehensive and digestible resource to help identify potential underlying causes of weight loss difficulties, so that our decisions can be logical and evidence-based.
 When we think of reasons that might be causing weight loss resistance, there are several factors at play. For the purpose of this post, I’m breaking them down into three main categories:
When we think of reasons that might be causing weight loss resistance, there are several factors at play. For the purpose of this post, I’m breaking them down into three main categories:
- Physiological Differences: How do our bodies have natural variations that won’t change? How do we accommodate those differences to allow for fat loss?
- Underlying Medical Problems: What are signs and symptoms that someone has a disease process preventing fat loss?
- Need for Support: How can we supplement and support the body to promote the nutrient sufficiency necessary for fatty acid metabolism? How does mental and social wellbeing come into play?
Save 80% Off the Foundations of Health
Expand your health knowledge on a wide range of topics relevant to you, from how to evaluate scientific studies, to therapeutic diet and lifestyle, to leaky gut and gut microbiome health, to sustainable weight loss, and much more!!!

My goal here is for you to leave this post having an action plan for troubleshooting weight loss, assuming all of the goals in Part 1 and Part 2 have already been met. We’re also going to have some real talk about what it takes to accomplish this challenging goal.
 Physiological Differences
Physiological Differences
In Part 1 and Part 2, I discussed in detail the metabolic requirements that we must meet in order to promote weight loss. However, we aren’t robots – there are many individual differences between us! We must identify and account for these differences if we want to facilitate the most efficient weight loss.
Food Intolerances
Food intolerances are probably one of the most buzzed-about aspects of the Paleo lifestyle. In eating Paleo, we seek to eliminate the foods we don’t tolerate. But, what does that actually mean? And what is the benefit of doing so when it comes to weight loss? The key word here, as we’ve discussed in the previous posts, is inflammation. When we regularly consume a food that our system doesn’t tolerate, it generates inflammation, which can prevent weight loss. When we think about food intolerances, I mentally divide it into three categories, each of which have different etiologies and symptoms:
Common allergenic foods. There are several foods that are considered common allergenic foods, meaning that many people have food allergies or intolerances to them (and yes, we can react to foods without having a downright allergy – the allergenic foods are more likely to trigger the i mmune system in the gut, causing an assortment of reactions). The eight most common allergenic foods are:
mmune system in the gut, causing an assortment of reactions). The eight most common allergenic foods are:
- Milk
- Eggs
- Fish
- Shellfish
- Tree nuts
- Peanuts
- Wheat
- Soybeans
Obviously, most of these are eliminated by a strict Paleo diet, but there are several that are included in the “standard” Paleo protocol. When thinking about foods that might elicit a reaction, I would also add nightshades, seeds, coffee, chocolate and alcohol (yes, the additional foods eliminated on the Autoimmune Protocol). So, we can eat a squeaky-clean Paleo diet and still include foods that don’t “work” for our bodies. What does this translate to? Some kind of intolerance reaction. There are many signs that you might be experiencing a food intolerance, including:
- Nausea, bloating, and/or diarrhea
- Fatigue and/or mood problems
- Brain fog
- Acne
- Headaches
- Rashes and other skin symptoms
…and, most pertinent to our discussion today: weight gain or difficulty losing weight! This is deeply related to the inflammation that food intolerances naturally create (especially if we consume the foods on the daily, which is very easy to do when it comes to Paleo-friendly foods like nightshades, coffee, or nuts and seeds!).
Managing this type of food intolerance is pretty straightforward: we just need to eliminate that food. This category is part of the “physiological differences” category simply because these intolerances are individual (the result of our unique genetics, environmental exposures, diet history, and lifestyle); for optimal health, they shouldn’t be included in our diet. For example, I know that I can’t have tomatoes without a reaction, but I’m lucky enough to be able to tolerate corn even within the AIP! Learning what our individual food intolerances are is critical for optimal health, including weight loss.
 One way to tackle the potential for general food intolerance is to follow the Autoimmune Protocol (AIP), which eliminates all foods known to stimulate the immune system (causing autoimmune symptoms and other reactions). I think that following the AIP strictly for at least a couple of months is the fastest way to see improvement in symptoms, and this may very well include spontaneous weight loss (I have seen this happen many times!). Just like everything else in the Paleo world, this is individual, so I recommend incorporating a strict reintroduction phase at the tail end of your AIP trial so that you can identify which individual foods are triggers for you. For 1-on-1 guidance through food sensitivity testing, see The Paleo Mom Consulting or to learn how to order and interpret your own tests, check out Test.Clear.Heal.
One way to tackle the potential for general food intolerance is to follow the Autoimmune Protocol (AIP), which eliminates all foods known to stimulate the immune system (causing autoimmune symptoms and other reactions). I think that following the AIP strictly for at least a couple of months is the fastest way to see improvement in symptoms, and this may very well include spontaneous weight loss (I have seen this happen many times!). Just like everything else in the Paleo world, this is individual, so I recommend incorporating a strict reintroduction phase at the tail end of your AIP trial so that you can identify which individual foods are triggers for you. For 1-on-1 guidance through food sensitivity testing, see The Paleo Mom Consulting or to learn how to order and interpret your own tests, check out Test.Clear.Heal.
Histamine, salicylate, & fructose intolerance. In addition to the possibility of being allergic to entire food groups, some people experience intolerance to specific molecules found within foods. Though the symptoms of each of these intolerances varies, I think categorizing them as “molecule intolerances” as a broader group is appropriate for the purpose of this article.
Histamine intolerance is a condition caused by a disequilibrium of accumulated histamine and the capacity of histamine degradation, i.e., when there is more histamine in your body (generally, consumed in the foods you eat and/or produced within your body) than your body can effectively handle. Histamine (which you will recognize as the key chemical produced by your body during an allergic reaction) is a type of molecule called a biogenic amine, which is created by removing the carboxyl group off of an amino acid. In the case of histamine, the amino acid that is “decarboxylated” is histidine. Histamine is a normal part of the diet (at least in small amounts) and also a normal product of the bacteria in our guts. In healthy people, histamine and other biogenic amines are rapidly detoxified by enzymes in the gut. In the case of histamine intolerance however, either production of histamine is unusually high or activity of these detoxification enzymes is unusually low (or both). I have written extensively about histamine intolerance in The Paleo Approach, but, luckily enough for you, the excerpt is also available on the blog at Teaser Excerpt from The Paleo Approach: Histamine Intolerance, and I discussed histamine intolerance with Stacy on The Paleo View Episode 170.
Salicylate intolerance is a reaction to a class of compounds called salicylates. Salicylates are the salts and esters of salicylic acid, an organic acid that is a key ingredient in aspirin and other pain medications, is frequently found in cosmetics and beauty products, and is also naturally occurring in varying concentrations in plants. In plants, salicylates act as a natural immune hormone and preservative, protecting the plants against diseases, insects, fungi, and bacterial infection. Salicylic acid is toxic to everyone in high doses. In the case of salicylate sensitivity/intolerance, much smaller doses produce symptoms of toxicity. The typical reactions are gastrointestinal and/or asthma-related and/or what is called pseudoanaphylaxis (the symptoms of anaphylaxis through a non-IgE antibody mediated pathway). I’ve written more extensively about this in the post, What is Salicylate Sensitivity/Intolerance?
Fructose (FODMAP) intolerance is a similar phenomenon by which certain sugars cannot be processed and absorbed by the gut. The term FODMAP is an acronym, derived from “Fermentable, Oligo-, Di-, Mono-saccharides and Polyols”. FODMAPs are short chain carbohydrates rich in fructose molecules which, even in healthy people are inefficiently absorbed in the small intestine. The symptoms of FODMAP issues are most often going to be gastrointestinal, but even GI distress can easily cause systemic inflammation (since 80% of the immune system is in the gut!). I wrote about FODMAP issues in the post Modifying Paleo for FODMAP- Intolerance and Modifying Paleo for Small Intestinal Bacterial Overgrowth (SIBO).
Intolerance and Modifying Paleo for Small Intestinal Bacterial Overgrowth (SIBO).
Again, for 1-on-1 guidance through food sensitivity testing, see The Paleo Mom Consulting or to learn how to order and interpret your own tests, check out Test.Clear.Heal.
Intolerance(s) due to leaky gut. There is a third category of intolerances that I think needs to be discussed independently. Leaky gut is another mechanism by which we can end up with food intolerances that may NOT be unique to our individual physiology. How? The leaky gut permits the entrance of many food particles into the bloodstream, which generates an immune response. If leaky gut is a problem, it needs to be addressed immediately before true (i.e., permanent) food intolerance is ruled in or out. I’ve written extensively about leaky gut in the post, What Is a Leaky Gut?
I know what you might be thinking: is it easier to just get tested for food allergies and sensitivities? Well, it is and it isn’t. Some people will have food sensitivities to foods that are allowed on the AIP. In this case, even following the AIP, 100% will not be sufficient to see substantial alleviation of your symptoms (and I have a whole post about this coming soon). In the case of nightshades, eggs, caffeine and alcohol (and NSAIDS, even though they aren’t a food), they can be problematic in a way that is not a food allergy or sensitivity, so you will very likely have to try an elimination diet strategy with those foods anyway. Food sensitivity testing also won’t tell you if specific foods are feeding Small Intestinal Bacterial Overgrowth or if you have a FODMAP-sensitivity. However, if getting food sensitivity testing done is within your budget, then I definitely recommend it as the information will still be very useful for you. Also, if you continue to have issues after following the AIP very strictly for several months, food sensitivity testing may help you find the missing link. However, not all foods are tested for and some sensitivities may still be missed. In this case, you may wish to work with a naturopathic physician or nutrition-savvy physician or chiropractor to do an even stricter elimination diet approach to narrow in on the culprits. At the risk of sounding like a broken record, for 1-on-1 guidance, see The Paleo Mom Consulting or to learn how to order and interpret your own tests, check out Test.Clear.Heal.
Genetic Mutations
In Part 1 of this series, we talked about the complex biochemical pathways that our bodies undergo to metabolize fatty acids, including the release of the fat molecules from adipose cells and the subsequent processing and breakdown of the molecules to be used for energy in the liver and elsewhere. Each of the steps in this process requires an enzyme – a protein that is specialized to facilitate chemical reactions. Enzymes are encoded for in our DNA and are absolutely essential to life. But, while the biochemical pathways are the same throughout our species, there are different slight variations to our DNA that might alter the function of the enzymes. These “mutations” or “variants” can change our ability to process fat and many other factors that go into fatty acid metabolism. In fact, there are several genetic variants that have been linked to difficulty losing weight.
 MTHFR, MTRR, & other Methylation Pathway Enzymes
MTHFR, MTRR, & other Methylation Pathway Enzymes
One of the buzzwords in the greater complementary and alternative medical world is the MTHFR mutation. The MTHFR gene is actually one of several genes that encode for proteins (MTHFR specifically encodes methylenetetrahydrofolate reductase) that methylates vitamins B12 and B9 (folate) for use in the methyl cycle. The methyl cycle is the process by which the body recycles methyl groups, which are used to control the activity of a huge variety of proteins through the post-translational modification methylation. Some extremely important hormones, such as cortisol and melatonin, and some extremely important neurotransmitters, such as epinephrine and serotonin, are controlled through methylation. Methylation is also an important conjugation mechanism in Phase 2 liver detoxification (see What The Heck Does Our Liver Do Anyway? Detoxification Explained).
When the methyl cycle functions improperly, certain molecules aren’t created, and others aren’t eliminated and then build up. The most notable molecule that builds up is homocysteine, which is highly related to many symptoms associated with MTHFR defects. Signs and symptoms that indicate an MTHFR mutation might be at play include:
- Mood problems (depression & anxiety)
- Autoimmune-like symptoms without a known autoimmune disorder
- Migraines
- Hormonal issues
- Fatigue
- Digestion problems
- Problems during pregnancy
- Elevated serum homocysteine (this is the biggest red flag)
The only way to know that we have an MTHFR or other mutation related to methylation is by getting a genetic test. This can be ordered by doctors in some states if you have demonstrated elevated homocysteine with elevated B12 (which builds up in the blood because it can’t be used in the methylation cycle). Definitely confer with a doctor before “deciding on your own” that you “must” have an MTHFR mutation. A doctor or alternative health practitioner can help you interpret your test results and start you on the appropriate supplemental protocol. The Paleo Mom Consulting offers functional medicine services.
This topic is complicated and merits further scientific research before I can make in-depth recommendations myself. If you are an MTHFR mutant (it’s kind of fun to refer to oneself as a mutant… or is it just me?), it’s critical to get enough folate into the diet (for ALL of us!) and many healthcare providers recommend supplementation with methylfolate (check with YOUR healtcare provider first!). The best food sources of folate are leafy greens and organ meats.
CLOCK Genes
Another family of genes, called the CLOCK genes, are responsible for our circadian rhythm and have been associated in multiple ways with obesity. How is that possible? Scientists are still trying to figure it out, but it  appears that certain CLOCK gene variants make someone much more susceptible to increased hunger and food cravings after inadequate sleep. Studies are showing that there are differences in the dopamine receptors in the brain, making highly palatable foods more irresistible to those with this mutation.
appears that certain CLOCK gene variants make someone much more susceptible to increased hunger and food cravings after inadequate sleep. Studies are showing that there are differences in the dopamine receptors in the brain, making highly palatable foods more irresistible to those with this mutation.
In the context of actionable steps, this is a REALLY easy one: make sure to get enough sleep! I would argue that all people should make sleep one of their priorities anyways. If you’re struggling with getting enough good quality sleep, my online sleep program Go to Bed is truly the most comprehensive resource on sleep in existence.
Vitamin Metabolism Genes
Okay, this topic is extremely broad and certainly more than I can cover for this purpose of this already very lengthy post! But, I think we should all be aware of the fact that there is much variance in the way that we metabolize certain vitamins and minerals – and this is largely due to our genes! One easy example is that people of different skin tones make and absorb vitamin D at different levels. A fair-skinned person can easily absorb too much vitamin D and reach toxic levels, whereas someone with a different genetic makeup may have trouble getting enough vitamin D to sustain even normal amounts!
I recommend that anyone with the available budget ask their doctor to order a comprehensive panel of serum vitamins and minerals (some of these are included in standard labs, and some aren’t). We’re also going to discuss this below.
We don’t need to dwell on the fact that we have different genes that influence our ability to lose weight. In fact, dwelling on it and being stressed out about your cellular makeup might even make some of your weight loss resistance worse! But, I think understanding all of the variation in our genetics and how to potentially accommodate our individual genetics is a critical way to influence. When it comes to vitamin metabolism challenges, these can usually be simply overcome with smart and targeted supplementation.
 Food Addiction
Food Addiction
There is one more big difference in the way that our bodies work from an individual perspective that I want to touch on before moving to medical concerns. The way that our bodies respond to different foods can vary a lot; while some foods are “designed” to make us addicted to them (you know, the ones with slogans like “bet you can’t have just one”), there are even Paleo foods that trigger the same neurological pathways. As I alluded to above, there are genetic differences in the way that our bodies produce and respond to dopamine.
Dopamine is a neurotransmitter that plays important roles in motor control, motivation, arousal, cognition, and reward, as well as a number of basic lower-level functions including lactation, sexual gratification, and nausea. The particular effect of dopamine signaling depends on the particular nerve pathway that’s involved, but the most relevant effect of dopamine for our purposes is responses to reward. In order to perform its functions, dopamine must bind to a receptor, so its efficacy is only as good as both its levels and the levels of its receptors (you could say this about almost any chemical messenger relationship). In addition, receptors can be more or less sensitive to dopamine, adding another layer of complication to understanding how this system impacts our health.
 Dopamine has been studied in many contexts because of its variety of functions. A particularly important relationship is the one between dopamine and food. When we eat highly palatable foods (those that are manufactured to be high in fat, sugar, and salt), our bodies release neurotransmitters that make us feel good (with dopamine being the main one). Because of that signaling, we crave more of these foods; this can create a horribly addictive process and compulsive eating. Certain foods quite literally have the same effect on the brain as drugs. This simple relationship can get skewed (and feel uncontrollable!) in a variety of other situations, including drug addiction and anxiety disorders. Certain characteristics can make people more susceptible to these patterns because of differences in their dopamine pathways, including obesity and eating disorders.
Dopamine has been studied in many contexts because of its variety of functions. A particularly important relationship is the one between dopamine and food. When we eat highly palatable foods (those that are manufactured to be high in fat, sugar, and salt), our bodies release neurotransmitters that make us feel good (with dopamine being the main one). Because of that signaling, we crave more of these foods; this can create a horribly addictive process and compulsive eating. Certain foods quite literally have the same effect on the brain as drugs. This simple relationship can get skewed (and feel uncontrollable!) in a variety of other situations, including drug addiction and anxiety disorders. Certain characteristics can make people more susceptible to these patterns because of differences in their dopamine pathways, including obesity and eating disorders.
The concept of “food addiction” is very controversial in the world of obesity and eating disorder researchers, so I’m going to avoid using that language too much (though, I am pretty strongly in the camp of believing that it is a real phenomenon). What’s not controversial? The notion that different people have variations in their release of and responsiveness to dopamine as well as the amount of receptors found on their brain cell surface, and these differences can impact our mental and physical health over time.
Opportunistic eating behavior and body mass index (BMI) are both positively associated with something called dopamine D2-like receptor binding potential (essentially, how readily D2 dopamine receptors bind to dopamine) in a particular part of the striatum (but they were negatively associated in the rest of the striatum). This pattern suggests that obese people have alterations in dopamine neurocircuitry that may increase their susceptibility to opportunistic overeating while making food intake less rewarding, less goal- directed, and more habitual. This translates into the vicious cycle that a lot of people with binge eating behaviors and weight problems (which are not necessarily seen in all of the same people!) experience: a cycle of being completely able to resist eating certain foods and then not being able to stop eating them once they start. The reason for this is actually a dampened or reduced reward response to foods. You would think that food addiction-like behavior would be a result of an exaggerated reward response to food, but actually, it’s the opposite! So, in addition to a compulsion to eat, those of us with a history of obesity find eating to be less fulfilling, and our brains register less enjoyment from food. We eat because it’s a habit to eat…. and that also means that we’re compelled to eat more in order to feel satisfied.
When it comes to recovering from food addiction, one interesting link with inadequate sleep. There are plenty of studies showing that getting enough sleep regulates hunger and cravings and makes us less likely to choose junk and fast food and more likely to choose fresh vegetables and fruits. And the link might be dopamine! Short answer, working on getting enough quality sleep is super helpful here too (again, see Go To Bed). For more details, see The Link Between Sleep and Your Weight.
 Underlying Medical Concerns
Underlying Medical Concerns
We’ve now spent a lot of time considering the ways that the body varies so that we can understand how certain individuals might be naturally susceptible to weight loss resistance. Beyond differences in our physiology, there are several medical reasons that someone might be unable to shed excess fat.
Insulin Resistance
We discussed the function of insulin in Part 2 of this series, including how it relates to sleep (spoiler alert: we need to get enough sleep in order to have proper insulin function!). But, there is a condition related to insulin that can undermine weight loss: insulin resistance.
 Insulin resistance occurs when the same amount of insulin elicits less of a response, so your pancreas has to release more and more of it to manage your blood glucose. Eventually, the cell receptors for insulin in the brain may stop being expressed (meaning there are fewer of them on the cell surface), so our circulating insulin doesn’t decrease appetite the way it’s supposed to. In that way, insulin resistance makes it difficult for us to regulate our hunger response, so our caloric intake can creep up without us noticing. Plus, when there is extra insulin circulating in our system, we have a tendency to think that all extra carbohydrate in circulation must be stored immediately; the insulin is kind of like a flag saying that we need to store carbohydrate right away.
Insulin resistance occurs when the same amount of insulin elicits less of a response, so your pancreas has to release more and more of it to manage your blood glucose. Eventually, the cell receptors for insulin in the brain may stop being expressed (meaning there are fewer of them on the cell surface), so our circulating insulin doesn’t decrease appetite the way it’s supposed to. In that way, insulin resistance makes it difficult for us to regulate our hunger response, so our caloric intake can creep up without us noticing. Plus, when there is extra insulin circulating in our system, we have a tendency to think that all extra carbohydrate in circulation must be stored immediately; the insulin is kind of like a flag saying that we need to store carbohydrate right away.
You might be thinking: but this sounds a lot of diabetes! And you’d be right – insulin resistance is a precursor to type 2 diabetes. There are several signs and symptoms that you are experiencing insulin resistance:
- Weight gain
- Menstrual problems
- Hirsutism: hair growth in unusual places (like the face or chest for women)
- Acanthosis nigricans: dark skin in the armpits, groin, and/or neck
I nsulin problems also tends to run in families; so, if you have family member with type 1 or 2 diabetes, you’re much more likely to develop insulin resistance and then full-blown diabetes. If you’re concerned about your insulin response, fasting blood sugar and fasting insulin can be ordered by your doctor. Then, we can calculate insulin resistance rather easily using an online calculator like the one included online by The Blood Code: HOMA-IR Calculator.
nsulin problems also tends to run in families; so, if you have family member with type 1 or 2 diabetes, you’re much more likely to develop insulin resistance and then full-blown diabetes. If you’re concerned about your insulin response, fasting blood sugar and fasting insulin can be ordered by your doctor. Then, we can calculate insulin resistance rather easily using an online calculator like the one included online by The Blood Code: HOMA-IR Calculator.
Modifying weight loss strategies to accommodate insulin resistance is quite simple: we just need to consume fewer carbohydrates and always consume them as part of a complete meal. Generally, I would recommend consuming between 50 and 100 grams of carbohydrates, because less than 50 grams can cause thyroid problems. Studies have also shown that supplementation with chromium can improve insulin resistance, so taking chromium picolinate could be beneficial (again, check with your doctor!).
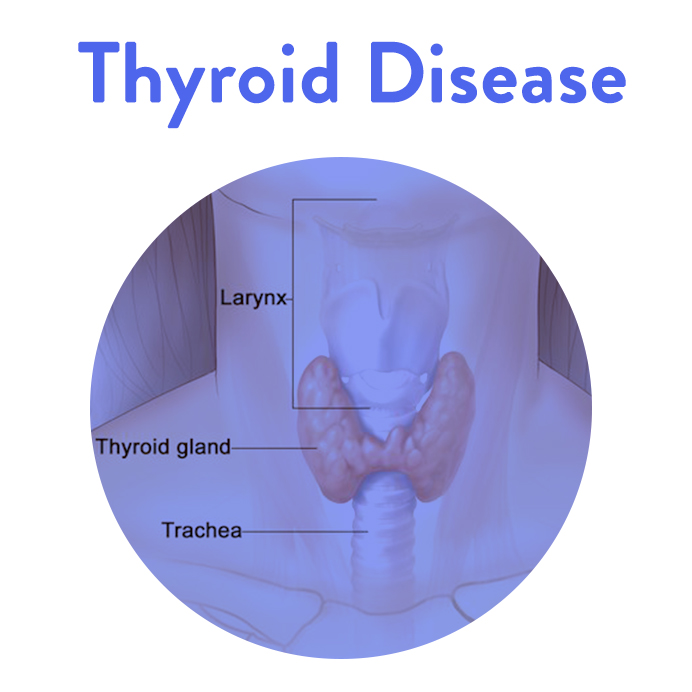 Thyroid Disease
Thyroid Disease
Thyroid Disease, in particular hypothyroidism or Hashimoto’s Thyroiditis, is also very commonly associated with weight loss problems (and weight gain!). Hypothyroidism can be caused by either medical treatment (like removal of a nodule or radioactive treatment of goiters) or by inflammation that leads to damage of a part of the thyroid, reducing its ability to make enough thyroid hormone. For this reason, most treatment of thyroid conditions merits taking thyroid hormone (because our body simply does not make it). There are other causes, like a dysfunction in signaling from the pituitary gland, which communicates that thyroid hormone should be released, but these are much more rare. Plus, there are some functional medicine perspectives on suboptimal thyroid function.
Hashimoto’s thyroiditis (or autoimmune thyroiditis), which I personally have and have discussed before on the blog (in my post Grief Upon Diagnosis: Uncovering Hashimoto’s Thyroiditis), is the main (80-90% of cases) cause of hypothyroidism. Hashimoto’s is an autoimmune condition in which the body attacks and kills thyroid cells. Over time, the thyroid stops being able to produce adequate thyroid hormone, which functionally causes hypothyroidism.
There are many symptoms of thyroid disease that extend beyond weight loss difficulties:
- Fatigue
- Coarse, dry hair
- Dry skin
- Hair loss
- Cold intolerance
- Muscle cramps
- Constipation
- Depression and irritability
- Memory loss
- Abnormal menstrual cycles
- Decreased libido
Like the other medical conditions we’re discussing here, experiencing multiple of these symptoms at one time merits a conversation with your doctor.
Compared to the complexities of some endocrine disorders, hypothyroidism is measured using a simple thyroid panel (that measures free T3, free T4, reverse T3, and TSH [thyroid stimulating hormone]). Including a test for thyroid antibodies is highly recommended (antibodies against Thyroid Peroxidase [TPO] and thyroglobulin), considering how commonly Hashi’s can be missed without their inclusion in testing due to the overly generous reference ranges for thyroid hormone levels.
The good news is that thyroid disease, once diagnosed, is relatively easy to manage. Most people who are able to manage their thyroid disease will see a spontaneous weight reduction if they are currently overweight or larger. From a weight loss perspective, all of the recommendations in Part 1 and Part 2 stand true. Notably, we must exercise to optimize metabolic function, and we must sleep in order to promote healthy endocrine function (thyroid gland included!).
Autoimmune Disease
There are more than one hundred confirmed autoimmune diseases and many more diseases that are suspected of having autoimmune origins (download a complete list here). The root cause of all autoimmune diseases is the same: our immune system, which is supposed to protect us from invading microorganisms, turns against us and attacks our proteins, cells, and tissues instead. Which proteins, cells, and tissues are attacked determines the autoimmune disease and its symptoms. In Hashimoto’s thyroiditis, the thyroid gland is attacked. In rheumatoid arthritis, the tissues of your joints are attacked. In psoriasis, proteins within the layers of cells that make up your skin are attacked. However, the root cause is the same.
The issue of autoimmune disease is far too great of a topic for me to cover in one blog post – that is why it is all over my site (considering this is my specialty!) and why I wrote The Paleo Approach. And, the many signs and symptoms of autoimmune disease vary too much by condition for me to list here! Why, then, am I including this category in this post? Because I firmly believe that autoimmune diseases are critically under-diagnosed, and even something as seemingly benign as weight loss resistance could point to a greater concern like an autoimmune disease.
The Paleo Autoimmune Protocol, typically abbreviated AIP, is a powerful strategy that uses diet and lifestyle to regulate the immune system, putting an end to these attacks and giving the body the opportunity to heal. As a complementary approach to healing, utilizing the AIP is one way to minimize inflammation, and it may dampen the symptoms of a suspected autoimmune disease. If you are concerned about autoimmunity, talk with your doctor or a licensed alternative care practitioner; then, you can start experimenting with the therapeutic potential of the AIP!
Hormonal Imbalances: Sex Hormones & Adrenal Fatigue
There is one remaining category of medical concerns that really merits our attention: hormonal imbalances. While thyroid disease and insulin resistance involve hormones and endocrine system regulation, the underlying cause is not hormonal imbalance but a deeper physiological process (autoimmune disease being the main one). Yet, there are other complicated endocrine disorders derived from imbalance. Considering hormonal function is key for weight loss (we need the signals saying that it’s okay for us to release stored fat, after all!), knowing about these disorders is absolutely key if weight loss proves unusually trying.
 Polycystic Ovary Syndrome (PCOS) (aka Androgen Excess)
Polycystic Ovary Syndrome (PCOS) (aka Androgen Excess)
PCOS occurs when a woman’s ovary grows multiple cysts. Scientists are still trying to determine the causes of PCOS, though we know that main causes of cyst development are excess androgens (like testosterone and DHEA) and/or insulin, PLUS PCOS is frequently co-morbid with autoimmune disease.
In addition to the hormonal imbalance that is inherently present in this condition, the cysts may release hormones that could cause big changes in the endocrine system, which we know in turn can cause symptoms in almost any organ system of the body. Common symptoms of PCOS include:
- Acne
- Hirsutism
- Disrupted menses
- Infertility
- Insulin resistance
- Fatigue
PCOS is diagnosed using a combination of medical history, physical exam, ultrasound of the reproductive organs, and blood work. To be diagnosed, a woman must present with two of three of the main symptoms: polycystic ovaries, menstrual dysfunction, or androgen dominance.
Weight loss resistance without any of the menses-related symptoms is probably not PCOS. But, PCOS can go unnoticed, so chat with your doctor if you have any of these symptoms.
Just like with most things in nature, there is kind of an “opposite” to PCOS, and that’s estrogen dominance. Estrogen dominance can be a nebulous topic, because some research is inconclusive, and clinicians treat it in many different ways. But, the reality is that estrogen dominance can definitely cause issues with weight loss.
Estrogen is one of several “female” hormones (we all have it in varying amounts, depending on our sex) that is released from the ovaries. The amount of estrogen in the female body should fluctuate according to her cycle, but, in some cases, the fluctuations wane, and estrogen remains elevated. This is notably in an opposite pattern from estrogen’s complementary hormone, progesterone, which should be high at different times of the month from estrogen. Since both hormones are involved in this balance, a deficiency in progesterone may also lead to estrogen imbalance. Importantly, especially for people trying to lose weight, we should note that estrogen is also produced by fat cells, so overweight and obese women are at much higher risk for estrogen dominance (this is also the reason that this population is at higher risk for breast, ovarian, and endometrial cancers).
So, what are some signs of estrogen dominance or excess estrogen? There is considerable overlap with other endocrine disorders, but the pattern of estrogen dominance is distinct. There are many potential symptoms of too much estrogen:
- Bloating
- Decreased sex drive
- Irregular, abnormal periods
- Bloating (not related to food)
- Headaches, especially before starting your period
- Thyroid dysfunction without a known cause
- Brain fog
- Insomnia
Clearly, not all of these symptoms are associated with the lady parts! Make sure to consider your entire picture of health when trying to determine if there is another reason for weight loss resistance.
You may be thinking, but what are the signs of progesterone deficiency?! Progesterone deficiency is mostly associated with dysmenorrhea or issues with menses. This could be severe PMS, irregular or heavy bleeding, or irregular cycles. Yes, this does overlap with estrogen dominance. In most cases, doctors will address both concerns within the same treatment protocol. Also, stress management is critical here, see How Chronic Stress Leads to Hormone Imbalance.
Considering the underlying cause of estrogen dominance can be excess weight, feel confident that you are on the right path! In the mean time, working with an alternative health practitioner or open-minded doctor is critical to get estrogen dominance under control to permit weight loss and reduce risk of adverse health outcomes in the long run! If you can’t find a physician to test you for hormone imbalances, consider functional medicine services from The Paleo Mom Consulting.
I have broken down adrenal fatigue into the details in my adrenal fatigue series, starting with Demystifying Adrenal Fatigue, Part 1, so I won’t sound like a broken record by describing it in detail here. Yet, I need to mention it, because adrenal fatigue can easily be an underlying cause of weight loss resistance! The very minimalistic view of adrenal fatigue is that it’s the result of serious chronic stress, which we are not evolutionarily equipped to handle. Chronic stress results in elevated serum cortisol all the time, which has a series of associated complications, including:
- Breakdown of muscle
- Excessive adrenaline release
- Hyperglycemia (elevated blood sugar)
- Weakened bones
- Worsened immune system function and responsiveness
- Inhibition of reproductive function
Adrenal fatigue happens when chronic stress continues without relief (and relief means more than just a weekend getaway or an occasional day off – I’m talking about actual stress management on the daily), and the adrenal glands stop being able to function properly. In the naturopathic medical community, adrenal fatigue was originally referred to as the general adaptation symptom – like your adrenals are literally adapting to too much stress! (And a reminder that someone in the conventional medical community is not likely to recognize adrenal fatigue. You’re more likely to get help from an integrative or functional medicine specialist or a licensed naturopathic physician).
If you’re worried about adrenal fatigue, or just want to learn more about it, I have detailed the underlying mechanism, testing, and management in my Demystifying Adrenal Fatigue series: Part 1, Part 2, and Part 3.
Wow, we just covered a lot of medical diagnoses very quickly! My intention here is not to scare you; rather, I hope to provide some potential relief if weight loss seems to be inappropriately difficult after all the topics in Part 1 and Part 2 of this series have been covered. Some of these disorders are nebulous, and others aren’t recognized by all medical practitioners, which creates an additional barrier to getting care. So, I hope that having a comprehensive list like this is enough of a footing for you to investigate on your own and find the right healthcare practitioner to help
That being said, I have one more topic to cover: what if you don’t have one of the physiological disadvantages or the medical conditions and are still struggling?! Additional support, from more angle than one, might just  be the thing we need.
be the thing we need.
Need for Support & Supplementation
We’ve talked a lot about things out of our control in this post. Now, I want to discuss the ways that we can take charge of our health and refocus our weight loss efforts in the face of plateaus or overall weight loss resistance. While all of the above must be considered when it comes to difficulty shedding pounds, there is more to the story here. Namely, are you getting everything you need?
Micronutrient Sufficiency Through Supplementation
In Part 1 and Part 2 of this series, I addressed the importance of micronutrients in the processing of weight loss. Believe it or not, we have a metabolic requirement for certain vitamins, minerals, and other cofactors in order to even permit weight loss! This is simply due to the fact that fatty acid metabolism (which is really fat loss at the microscopic, cellular level) is a series of biochemical reactions that require enzymes and their vitamin cofactors – and without the necessary molecules, these reactions won’t proceed, and we won’t lose weight!
I’ve written generally about this topic before in the post, 10 Nutrients That Can Help You Burn Fat. However, I want to offer some more direct guidance for someone with a longterm history of nutrient deficiency or someone who is worried about their stalled or stagnant weight loss:
- Start with a panel to investigate your micronutrient status. While there are some indicators of our nutrient status (e.g., weak hair and nails), there is no way to truly know what nutrients we are deficient or sufficient in. I highly suggest getting a comprehensive blood panel that measures blood levels of micronutrients. Most alternative care practitioners will have access to this, and some PCPs are even able to order them with justification (i.e., weight problems count, and insurance may cover this!). From here, we can establish a baseline and make targeted changes
- Utilize targeted supplementation with practitioner-quality brands. Supplements, like many things in life, are a double-edged sword. On the one hand, they are a great way to improve our health and even optimize our progress. But, since they aren’t regulated by the FDA, it can be tough to know exactly how much we’re getting (especially when we talk about herbs, but that’s another story altogether!). I must always recommend that we start with practitioner-quality brands like Metagenics, Douglas Labs, Seeking Health, Standard Process, and others. This is just one reason of many reasons to work with a practitioner for care management, including weight loss! They can recommend the appropriate supplements based on your individual test results.
- Focus on nutrient density and diversity in food choices. In addition to targeted supplemental support, don’t forget about food! Focusing even more on getting at least the RDV of fruits and vegetables (or even more), and including a diversity of plant and animal matter in your diet, is one way to enhance nutrient sufficiency and to continue to work synergistically with supplements to support weight loss and beyond. See 3 Ways to Up Your Nutrient Game.
Clearly, I can’t emphasize my love of micronutrients enough, nor could I stress how important they are for weight loss! But, this is hardly the most important way that we should seek out support during weight loss.
Social Support: Leaning on Friends and Family or Finding a Community
It’s important to address the fact that weight loss is even harder when we have to do it alone. An unsupportive partner, friends, or other community can easily sabotage a weight loss effort. But, having the right support is essential for health and has been demonstrated to improve weight loss.
 The bottom line is that we sometimes have to ask for help and support from our loved ones when it comes to weight loss. A big part of being able to ask for help (and getting it) is having a good support network. Social connection is key for mental health and stress management. Research has proven the role that connection plays in health through two extremes:
The bottom line is that we sometimes have to ask for help and support from our loved ones when it comes to weight loss. A big part of being able to ask for help (and getting it) is having a good support network. Social connection is key for mental health and stress management. Research has proven the role that connection plays in health through two extremes:
- Social isolation and loneliness corresponds with increased risk of morbidity and mortality
- A strong social support network corresponds with decreased risk of disease and increased longevity.
Having a social support network improves health, and not having one pretty dramatically increases risk of disease. How does this work? We are hardwired to be social creatures. Positive social interactions stimulate changes in hormones that affect nearly every system in the body. So, how large is the impact on our health from feeling connected and having a sense of community? This quote sums it up well:
“Social relationships, or the relative lack thereof, constitute a major risk factor for health—rivaling the effect of well-established health risk factors such as cigarette smoking, blood pressure, blood lipids, obesity and physical activity” — House, et al; Science, 1988
Connection is just as important for your health as not smoking, being a healthy weight, and being active. That’s great news if you are close with your family, have an awesome group of friends, and live in a tight-knit community. Not so cool if you’re like a growing number of us who live far from home, feel like we have friendly acquaintances in our lives more so than true friends, and generally have a sense that life would be better in a different city or region. Finding some sort of community, even online, could be hugely beneficial when trying to lose weight! This is one of the reasons why I host several online Facebook groups for support, including the AIP Community and the Go to Bed Challenge page.
Having a strong social network provides a huge range of benefits. It can make all the difference to have someone you can count on to watch your kids, pick something up at the grocery store for you, or talk to when you’ve had a bad day. Research actually shows that having a closer inner circle of 8 to 10 people that you can depend on and confide in is optimal. Feeling socially connected lowers cortisol and makes us more resilient to psychological stressors, meaning that our body produces less cortisol when we’re stuck in traffic and late for a meeting. Having positive social interactions in your life, reduces the effects of chronic stress, and that leads to improved health over the long term.
Physical touch may be even better. Research has shown that physical connection— whether hugging a family member, enjoying sexual relations with your partner, cuddling with a pet, or receiving therapeutic touch or massage—reduces cortisol. And, as we discussed in Part 1 and Part 2 of this series, it’s really important to have fine-tuned cortisol regulation when it comes to weight loss.
Touch, love, and positive social interactions increase the hormone oxytocin, which is sometimes referred to as the “love hormone.” Oxytocin is produced by specialized neurons in the thalamus and then stored and released by the posterior pituitary gland. Upon release, oxytocin is associated with feelings of contentment and calm, reductions in anxiety, and increases in human bonding and trust. It also inhibits fear and nervousness. You may recognize oxytocin as the hormone released during childbirth and breastfeeding. Like most hormones discussed, it has many roles in the body.
 Importantly, increased oxytocin levels lead to a decrease in activity in the hypothalamic-pituitary-adrenal axis (the HPA axis controls the production of cortisol!) and enhanced immune function. Essentially, increasing oxytocin protects against stress. In fact, positive social interaction has been shown to have a direct impact on wound healing, attributable to increased levels of oxytocin. Oxytocin also modulates inflammation by decreasing some pro-inflammatory cytokines (chemical messengers of the immune system). Whether the effects of oxytocin are completely owing to direct interactions with the immune system or to the effects on cortisol and the HPA axis remains unknown. Either way, the feeling of connection is important for general health and wellbeing.
Importantly, increased oxytocin levels lead to a decrease in activity in the hypothalamic-pituitary-adrenal axis (the HPA axis controls the production of cortisol!) and enhanced immune function. Essentially, increasing oxytocin protects against stress. In fact, positive social interaction has been shown to have a direct impact on wound healing, attributable to increased levels of oxytocin. Oxytocin also modulates inflammation by decreasing some pro-inflammatory cytokines (chemical messengers of the immune system). Whether the effects of oxytocin are completely owing to direct interactions with the immune system or to the effects on cortisol and the HPA axis remains unknown. Either way, the feeling of connection is important for general health and wellbeing.
Part of having a functional support network is actively choosing the people in it. If there are people in your life who are not supportive or who undermine your efforts to heal (either subversively or overtly) or who simply cause more stress than they alleviate, you can choose not to have these people in your life. Yes, navigating family (and friend and work and school) politics can be tricky, and each situation has its unique challenges. But limiting the presence of negative people in your life as much as possible (you don’t necessarily have to totally cut them off) will significantly decrease your stress, making it easier to reach your goals and lose weight.
Reality Check: Remembering the Goal
Okay, I might be doing us all a disservice without mentioning one last thing: it’s really, really easy to make excuses not to do the work and implement the steps necessary to lose weight. It’s hard work. I know this for a fact, considering all the pounds I’ve lost and gained and lost over the years. But, the bottom line is that we won’t lose weight and maintain that weight loss without the putting the work in.
So, after reading all of this information, I implore you to consider whether you’re truly implementing all of techniques that I’ve outlined in this series. The bottom line is that we must be doing it all when we want to lose weight efficiently and healthfully and keep it off. I’m not here to say that it isn’t tough, because it is. But we can’t count on medical intervention to do it for us, and there is no magic bullet for weight loss.
I’m almost done with my epic weight loss series. But, there is one more topic that we still need to cover, and it’s a big one: how do we set the right weight loss goals? What are the advantages and disadvantages of setting really big goals versus step-by-step goals? Are there any benefits at all of actually being a few pounds overweight?! All of this information can be found in the scientific literature, and I’m excited to walk through it together. Next up, we’re doing to discuss using the Obesity Paradox to inform our weight loss goals!
Citations
Lorenz AR, Scheurer S, Vieths S. Food allergens: molecular and immunological aspects, allergen databases and cross-reactivity. Chem Immunol Allergy. 2015;101:18-29.
Lomer MC. Review article: the aetiology, diagnosis, mechanisms and clinical evidence for food intolerance. Aliment Pharmacol Ther. 2015;41(3):262-75.
Kovacova-hanuskova E, Buday T, Gavliakova S, Plevkova J. Histamine, histamine intoxication and intolerance. Allergol Immunopathol (Madr). 2015;43(5):498-506.
Weidenhiller M, Layritz C, Hagel AF, Kuefner M, Zopf Y, Raithel M. [Histamine intolerance syndrome (HIS): plethora of physiological, pathophysiological and toxic mechanisms and their differentiation]. Z Gastroenterol. 2012;50(12):1302-9.
Baenkler HW. Salicylate intolerance: pathophysiology, clinical spectrum, diagnosis and treatment. Dtsch Arztebl Int. 2008;105(8):137-42.
Wilder-smith CH, Olesen SS, Materna A, Drewes AM. Predictors of response to a low-FODMAP diet in patients with functional gastrointestinal disorders and lactose or fructose intolerance. Aliment Pharmacol Ther. 2017.
Tsang BL, Devine OJ, Cordero AM, et al. Assessing the association between the methylenetetrahydrofolate reductase (MTHFR) 677C>T polymorphism and blood folate concentrations: a systematic review and meta-analysis of trials and observational studies. Am J Clin Nutr. 2015;101(6):1286-94.
Altuğ Şen T, Köken R, Narcı A, Yılmazer M. Homocysteine and ghrelin link with polcystic ovary syndrome in relation to obesity. J Pediatr Adolesc Gynecol. 2011;24(4):211-7.
Narayanaswami V, Thompson AC, Cassis LA, Bardo MT, Dwoskin LP. Diet-induced obesity: dopamine transporter function, impulsivity and motivation. Int J Obes (Lond). 2013;37(8):1095-103.
Zhao L, Fu Z, Wu J, et al. Inflammation-induced microvascular insulin resistance is an early event in diet-induced obesity. Clin Sci. 2015;129(12):1025-36.
Verma A, Jayaraman M, Kumar HK, Modi KD. Hypothyroidism and obesity. Cause or effect?. Saudi Med J. 2008;29(8):1135-8.
Versini M, Jeandel PY, Rosenthal E, Shoenfeld Y. Obesity in autoimmune diseases: not a passive bystander. Autoimmun Rev. 2014;13(9):981-1000.
Zheng Y, Sereika SM, Danford CA, et al. Trajectories of Weight Change and Predictors Over 18-Month Weight Loss Treatment. J Nurs Scholarsh. 2017;49(2):177-184.