A year ago, I started my in-depth series on how to utilize a Paleo framework to promote healthy weight loss. It’s been quite the year for me (have you seen Paleo Principles, my 6lb epic tome of science and recipes?! And the AIP Lecture Series?), but I wanted to finish up this series. In this series of posts, I have outlined an evidence-based, Paleo-centric approach to healthy weight loss that emphasizes nutrient density and lifestyle change. In Part 1, we discussed how to tweak Paleo to promote natural weight loss, and in Part 2, we discussed the lifestyle factors that must be in place to permit fat metabolism and weight loss (and yes, I do mean to use the word “must!”). Then, Part 3 featured the many ways that weight loss can go awry (and how to potentially fix them!). Finally, with this post, I hope to bookend all of this information with a discussion on appropriate goal-setting with body composition in mind.
Table of Contents[Hide][Show]
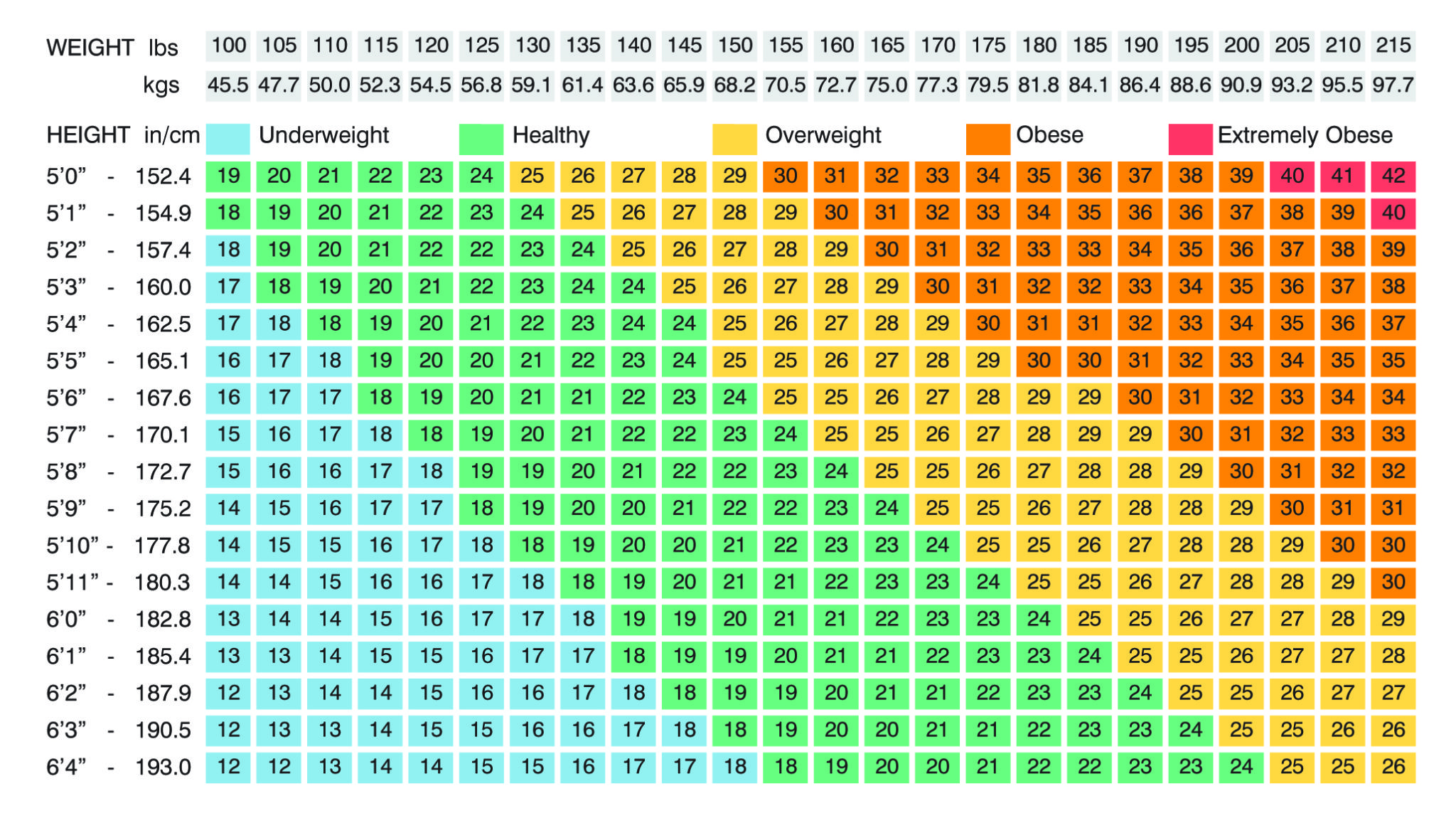
 I’ve been very open about my weight loss journey (you can read more about it in my Story), which is one of the reasons why I was inspired to write this post series: I feel like an expert, both professionally and personally! Also for this reason, there is one more issue that I’d like to address: the concept of evidence-based body composition goals. Why? It’s really, really easy to get caught up in the pursuit of a 6-pack, or even just trying to get into a “healthy weight range” for our height according to the BMI. I hear from many people who are frustrated that they can’t lose those last 10 pounds. But the scientific evidence suggests that throwing all of our effort into leanness might not be the best idea. (Spoiler: there might even be protective effects for people with a little more adipose [fat] tissue! We’ll get to this later, but what this suggests is that losing those last 10 pounds might not be the healthiest goal!). That being said, I think we can turn to the literature to make the best choices when it comes to body composition goals, extending it all past a number on the scale.
I’ve been very open about my weight loss journey (you can read more about it in my Story), which is one of the reasons why I was inspired to write this post series: I feel like an expert, both professionally and personally! Also for this reason, there is one more issue that I’d like to address: the concept of evidence-based body composition goals. Why? It’s really, really easy to get caught up in the pursuit of a 6-pack, or even just trying to get into a “healthy weight range” for our height according to the BMI. I hear from many people who are frustrated that they can’t lose those last 10 pounds. But the scientific evidence suggests that throwing all of our effort into leanness might not be the best idea. (Spoiler: there might even be protective effects for people with a little more adipose [fat] tissue! We’ll get to this later, but what this suggests is that losing those last 10 pounds might not be the healthiest goal!). That being said, I think we can turn to the literature to make the best choices when it comes to body composition goals, extending it all past a number on the scale.
This is fascinating, complicated, and controversial stuff. But, to understand this phenomenon, we need to discuss the ins and outs of body composition first. Woot!
Body Composition: A Meaningful Metric for Progress
 The term “body composition” is thrown out there a lot in the weight loss and fitness community. But, what does it actually mean? Body composition simply refers to the amount of fat compared to lean mass (muscle, bones, and organs) that someone carries. It’s important not to get trapped into thinking that there is one ideal body composition (no matter what personal trainers and the like might claim); there are many natural variances in someone’s body composition, and fighting this phenomenon may do more harm than good. Importantly, it is also natural for women to store more body fat than men – women need fat for breast tissue, to support healthy fertility, and to support healthy estrogen levels. Specifically, women must maintain at least 12% of their weight as “essential” body fat for optimal health, whereas men only need 3% of their weight to be essential body fat. Still, this doesn’t mean that all men and women should be aiming to ONLY have this amount of fat on our bodies! This is our bare minimum amount of fat. We will talk more about this in just a minute. First, we need to talk about the ways that we measure and report body composition so that we might understand the strengths and limitations of how we approach our goals.
The term “body composition” is thrown out there a lot in the weight loss and fitness community. But, what does it actually mean? Body composition simply refers to the amount of fat compared to lean mass (muscle, bones, and organs) that someone carries. It’s important not to get trapped into thinking that there is one ideal body composition (no matter what personal trainers and the like might claim); there are many natural variances in someone’s body composition, and fighting this phenomenon may do more harm than good. Importantly, it is also natural for women to store more body fat than men – women need fat for breast tissue, to support healthy fertility, and to support healthy estrogen levels. Specifically, women must maintain at least 12% of their weight as “essential” body fat for optimal health, whereas men only need 3% of their weight to be essential body fat. Still, this doesn’t mean that all men and women should be aiming to ONLY have this amount of fat on our bodies! This is our bare minimum amount of fat. We will talk more about this in just a minute. First, we need to talk about the ways that we measure and report body composition so that we might understand the strengths and limitations of how we approach our goals.
Measuring Body Fat
In my opinion, measuring body fat is one of the best ways to tailor our goals appropriately. Yet, there are a bunch of ways to do so! Let’s briefly review the different types of body fat measurement tools.
 DEXA Scan. The ultimate “gold standard” way of measuring body fat is with a DEXA scan – this is like an advanced x-ray that measures exactly how much of each type of tissue we have, including separating different types of fat. Most people won’t have access to this method because of cost and availability, but this is the researcher’s preferred way to measure body composition, so it’s important to know about.
DEXA Scan. The ultimate “gold standard” way of measuring body fat is with a DEXA scan – this is like an advanced x-ray that measures exactly how much of each type of tissue we have, including separating different types of fat. Most people won’t have access to this method because of cost and availability, but this is the researcher’s preferred way to measure body composition, so it’s important to know about.- Bioelectrical Impedance. This method of body composition measurement determines someone’s body fat percentage by reading the electrical current that can run through the body. Compared to a DEXA scan, bioelectrical impedance is much easier to access (most personal trainers will have one as will functional and integrative medicine practitioners) and use, – and it’s definitely way cheaper! However, it’s important to use bioelectrical impedance at the same time of day every time, ideally before eating or drinking anything (because that will affect the amount of tissue that can conduct electricity well, overestimating or underestimating body fat percentage). At-home models aren’t quite as accurate as what professionals use, but a much better investment than a regular bathroom scale for daily or weekly monitoring.
- Skin-Fold Calipers. Calipers are used to measure fat by pinching the skin at different areas. Measuring the skin-fold distance gives an accurate estimate of the amount of fat between the skin and underlying muscle or organs. After measurements are taken at several areas all over the body, the values are entered into a computer that calculates total body fat percentage. When done correctly, calipers have been shown to be effective by ±3% (for some people,this isn’t a big deal, but for others, it’s a huge deal!). Like the other measurement techniques, it is probably a good idea to get help from someone trained to do this measurements.
- BMI. BMI isn’t actually a measure of body composition… we’ll get to it later.
So, we can see that there are a few valid approaches to keeping track of body fat. And, as we discussed in Part 1 of this series, we are really aiming to lose stored fat when we say “weight loss.” Keeping track of body fat percentage is one way to measure progress without focusing on the number on the scale, which we know can be detrimental for out mental health (I’ve talked about my complicated relationship with the scale before on The Paleo View Podcast before and in Should You Throw Out Your Scale?. In short, I need to keep the scale out to keep track of where I’m at personally, but there are known benefits to going on how your clothes feel and how your body is moving, etc. It’s all about individuality!). It’s true: “weight loss” is actually a complicated equation that includes losing stored fat, muscle mass, and water weight. Let’s pause for a moment to dispel some myths about how these three factors contribute to changing numbers on the scale.
 What is BMI?
What is BMI?
The standard when it comes to describing body composition from a scientific perspective is BMI: body mass index. The BMI, which is calculated from height and weight, was created to attempt to quantify someone’s mass (ALL of it, including fat, muscle, and bone) into several categories: underweight, normal weight, overweight, and obese. There is a huge, obvious limitation to this measurement of body composition: it doesn’t take composition into account at all! This creates the classic paradox of the ultra-lean body builder who has an obese BMI, or someone may be “overfat” with a normal BMI.
So, why do we even talk about BMI? One of the main reasons to talk about BMI is that it’s used in scientific research very, very often (and when you’re talking about average BMI of a population, it’s not as flawed of a measurement as when we’re using it to track our own progress). If we want to read scientific papers and translate them to real life, we need to accommodate BMI into our way of thinking. This is particularly important because of research about how elevated BMI might actually be health protective (see below! It’s pretty mind-blowing). So, in a lot of ways, understanding BMI is one method of increasing our own scientific literacy – we need to be able to translate the findings in scientific papers to digestible, manageable lifestyle choices, right? BMI is the standard when it comes to the science, because it’s an easy calculation taken from height and weight (pro tip: if you’re ever digging through scientific papers and see that the scientists didn’t take the height and weight of their participants, run the other way! Self-reported height and weight are really unreliable and a red flag when it comes to looking for high quality scientific work).
Utilizing BMI comes down to ease and convenience, but it’s important to take it with a grain of salt. When it comes to talking about body composition, I’ve found that overall adiposity (the amount of body fat we have relative to our lean tissue) might be a better indicator of healthy metabolism.
Nutrivore Weekly Serving Matrix
An easy-to-use and flexible weekly checklist
to help you maximize nutrient-density.
The Weekly Serving Matrix is very helpful! I’ve been eating along these lines but this really helps me know where to focus vs. which foods serve a more secondary role. It’s super helpful and has taken a lot of worry out of my meal planning. Thanks!
Jan
“Overweight” vs “Overfat”
 Considering how limited the BMI is, some researchers have begun to distinguish the difference between being overweight according to BMI versus being overfat (i.e., genuinely having “too much” or excess adipose tissue). While a lot of research is still presented in BMI findings, I think taking the concept of overfat into consideration can be really helpful when we think about our weight loss goals. Still, the concept of overfat doesn’t save a lot of concern: 90% of men and 80% of women in the developed world are overfat.
Considering how limited the BMI is, some researchers have begun to distinguish the difference between being overweight according to BMI versus being overfat (i.e., genuinely having “too much” or excess adipose tissue). While a lot of research is still presented in BMI findings, I think taking the concept of overfat into consideration can be really helpful when we think about our weight loss goals. Still, the concept of overfat doesn’t save a lot of concern: 90% of men and 80% of women in the developed world are overfat.
Still, this metric may give us more information than just the BMI, since it incorporates more information about body composition – and, as we discuss this issue of healthy weight loss, what we’re all talking about is fat loss. (Not a lot of people want to lose muscle and bone!)
There are guidelines for body fat that have been produced by the NIH; these take sex and age into consideration, making overfat a much more specific statement relative to BMI (in a great way). Obtaining body fat percentage from one of the body composition measures I mentioned above is probably the best way to go about managing weight loss, even relative to keeping track of pounds lost (and yes, doing both is probably the best option!).
Estimating Fat Percentage using BMI
Researchers have developed a relatively simple formula for estimating body fat percentage based on BMI for the average population (not bodybuilders or “skinny fat people”). The formula is
Body fat % = (1.39 x BMI) + (0.16 x age) – (10.34 x gender) – 9
with gender equal to 1 for men and 0 for women to account for the higher body fat percentage of women.
I’m not suggesting that we use this formula to track our body fat percentage, but rather that we can use this formula to convert some research findings that use BMI into body fat percentage.
Assuming you’re 35 years old, here’s how BMI, on average, corresponds to body fat percentage:
| Men | Women | ||
| BMI | Fat % | Fat % | |
| Underweight | <18.5 | <12% | <22% |
| Normal weight | 18.5-25 | 12% – 21% | 22% – 31% |
| Overweight | 25-30 | 21% – 29% | 31% – 38% |
| Obese | >30 | >29% | >38% |
From this, we can conclude that aiming to be a normal weight for a 35-year old woman would mean aiming for a body fat percentage between 22% and 31%. Of course, we still need to discuss whether aiming to be a normal weight is the right goal!
So, we know that body composition is an important consideration as we start or continue a weight loss journey, and we understand that the BMI is limited in its value, especially when it comes to goal-setting, but instructive in terms of understanding populations as a whole. Next, I want to take a step back and answer some “why” questions. That is, why should we aim to have lower body fat anyways? And are there any exceptions or additional considerations? (Spoiler alert: there are!).
Adipose Tissue: Some Physiology
 When it comes to the science of weight loss, there is value turning back to the absolute core concepts, i.e., physiology and biochemistry. We talked a lot about biochemistry in Part 1 of this series, in which we discuss some of the aspects of fat metabolism that can be supported with dietary modifications. But, I’m a huge fan of taking the “hows” and “whats” of basic physiology and using them to provide a rationale for behavioral changes, too – and this is one of the reasons why I decided to make this series of posts: because there are benefits to finding and maintaining a healthy weight.
When it comes to the science of weight loss, there is value turning back to the absolute core concepts, i.e., physiology and biochemistry. We talked a lot about biochemistry in Part 1 of this series, in which we discuss some of the aspects of fat metabolism that can be supported with dietary modifications. But, I’m a huge fan of taking the “hows” and “whats” of basic physiology and using them to provide a rationale for behavioral changes, too – and this is one of the reasons why I decided to make this series of posts: because there are benefits to finding and maintaining a healthy weight.
I don’t think I need to harp on the well-known health detriments of excess weight – we all hear about that all the time. We know that there are many chronic diseases associated with being obese, including heart disease, diabetes, nonalcoholic fatty liver disease, and cancer. That is enough reason to assess our body composition and work to be at our own individualized ideal body weight. Yet, there are some unique characteristics to adipose (fat) tissue that might be new to some of my readers and could provide additional insight as to why they face certain health issues or other challenges.
Excess body fat contributes to a vicious cycle of insulin resistance and chronic inflammation, which in turn makes it difficult to lose body fat (and makes it really easy to gain fat! We talked about this in much more detail in Part 1 of this series.). This cycle is basically responsible for all of the chronic health issues associated with obesity. Interestingly, I think that this also explains why there are plenty of people with excess fat who are able to maintain healthy bloodwork and avoid disease – my guess is that, for whatever reason, they are predisposed to carry more weight without suffering the consequence of inflammation and insulin resistance. However, until we understand these phenotypical differences in obesity, it’s crucial that we know the underlying possibilities for disease and act responsibly from a diet and lifestyle angle (because why not be a health overachiever, right?!).
The explanation for this obesity-insulin resistance-chronic inflammation cycle is actually pretty simple. It all boils down to the action of adipokines, the immune-modulating proteins that are released by fat cells (and yes, these are cousins of the cytokines that I discuss a ton in article related to immune function and in my books). There are a huge variety of adipokines – at least a thousand -, and they all have their own systemic effects. The best-known adipokine is leptin, known as one of the main long-term satiety signals (see The Hormones of Fat: Leptin and Insulin and The Hormones of Hunger). Fat cells release leptin to tell the brain that there are fat stores, down-regulating the amount of hunger that the individual feels. However, when too much leptin is produced chronically (from overeating and/or being overfat), we can develop leptin resistance – the brain becomes less responsive to the leptin! Interestingly, scientists have experimented with administering leptin to subjects with obesity, and the results were pretty disappointing (people didn’t lose weight, and they stopped doing trials like this in the 90s). But, establishing a normal weight tends to regulate leptin levels, so the cause and effect mechanism is a little unclear – we just know that leptin is important and released in direct proportion with the amount of body fat someone has.
Another adipokine is adiponectin, which is partially responsible for regulating blood sugar and fat metabolism. Surprisingly, this non-hormone protein may be found in larger concentrations in the blood than most hormones! Adiponectin stimulates the utilization of stored fats and promotes insulin sensitivity. It has been shown that individuals with obesity and eating disorders have disrupted adiponectin levels, and weight loss has been shown to restore serum levels to normal. Dysregulation of leptin, adiponectin, and other metabolically-active adipokines is almost certainly responsible for the incredibly frustrating weight loss resistance that many people with excess body fat experience.
Apart from these two adipokines specifically associated with metabolism, fat cells ALSO release immune-stimulating cytokines and other molecules, creating a natural tendency toward inflammation. Long-term “acute” inflammation becomes chronic inflammation, and the immune system can become suppressed. This contributes to an inflammatory milieu that makes weight loss more difficult (what a frustrating cycle!). This is one of the main reasons why I recommend an anti-inflammatory diet to promote weight loss (see Healthy Weight Loss with Paleo, Part 1: Modifying Dietary Choices to Support Fat Metabolism).
However, while some of the above could certainly be used to argue that we should avoid weight gain and promote low BMIs at all cost, there is substantial evidence to suggest that a few extra pounds could be protective for health (seriously. Keep reading).
What is the Obesity Paradox?
 There is one major point that I want to address as we discuss how to set appropriate goals: the obesity paradox. “The obesity paradox” refers to findings that suggest that people in the overweight and obese category may have some health protective effects (there are also some similar findings with high cholesterol, but that may be best discussed in another post!). While public consciousness of the obesity paradox is more recent, findings suggesting a benefit to obesity have been published since at least 1999.
There is one major point that I want to address as we discuss how to set appropriate goals: the obesity paradox. “The obesity paradox” refers to findings that suggest that people in the overweight and obese category may have some health protective effects (there are also some similar findings with high cholesterol, but that may be best discussed in another post!). While public consciousness of the obesity paradox is more recent, findings suggesting a benefit to obesity have been published since at least 1999.
Obesity Paradox Findings
Results suggesting that obesity has a protective effect first came out in a study of patients undergoing hemodialysis, suggesting that they have better outcomes in treatment. Since then, studies have demonstrated better health outcomes for people with overweight and obesity (compared to “normal” weight people) in patients with a variety of health conditions, ranging from severe to inconvenient, including:
- Heart failure
- Heart attack
- Acute coronary syndrome
- Chronic obstructive pulmonary disease (COPD)
- Chronic kidney disease
- Peripheral arterial disease
- Stroke
- Type 2 diabetes
- Post-operative complications and amputation risk
- Critical illness and hospitalization
- Osteoporosis
There’s also some some general mortality statistics: people with obesity may live longer when hospitalized with a serious illness. It seems that the protective effects are strongest in people who, despite their obese status, have maintained a normal metabolism (no metabolic syndrome or diabetes) and generally preserved their fitness. I think that last point is really critical, and worth visiting later, so hold onto it.
Altogether, this information is striking (just one study would be something – tons of studies is another!). However, like all research, there is a lot more context to consider here. If obesity is a disease epidemic, then how can it also health protective?! Let’s explore a little deeper.
Explanations and Mechanisms of the Obesity Paradox
- Selection bias. Since a lot of these studies are conducted to evaluate people with serious and chronic illnesses, they typically include older people. For example, one study had an average age of 54. This means that the results of the study can’t be applied to everyone but rather middle-aged people and older. Moreover, most studies don’t take into account how long people were obese: in all likelihood, most of the individuals with overweight or obesity had not had excess adiposity until late adulthood (but there is no way of knowing). The general consensus is that the detrimental effects of obesity are dose/time-dependent, meaning that duration of being overweight/obese matters. This is one of the many reasons that we are concerned about childhood weight.
- Body composition & muscle mass. As we discussed above, BMI is a metric that does not give insight into body composition – someone with obesity might be lean, and someone with a low BMI might have a few extra pounds of fat and little muscle. Researchers believe that these studies may be capturing a benefit to additional muscle mass. This is supported by the notion that sarcopenia (low muscle mass, which is more likely in someone with a low/underweight BMI). Likewise, more muscle mass is likely to be associated with more strength. Strength, in turn, is associated with better nutrition status.
- Changes in cardiovascular & endocrine function. There are also changes in cardiovascular function that may be protective against mortality from disease. For example, people with severe obesity produce more precursor cells to blood vessels, and this is protective against the damage that can happen to blood vessels as a result of type 2 diabetes. Similar changes to immune function and hormone production end up being protective against death from chronic disease – a really interesting contrast to the conventional wisdom that excess weight is practically a death sentence.
These findings have continued to stump researchers for years. Some scientists, including my friend Stephan Guyenet, PhD, have remained skeptical and proposed several criticisms of the so-called obesity paradox.
Criticisms of the Obesity Paradox
Though there is strong epidemiological evidence for the obesity paradox, there is also a lot of evidence that obesity isn’t exactly a health marker. So, what’s the deal? There is indeed some criticism of the obesity paradox. The most significant one is that smokers, who generally tend to have smaller BMIs, skew the data significantly – especially when we consider that smoking has a known detriment to every condition or effect listed above. Recalculations of relative risk that include only “never smokers” does change the finding. Another criticism is that, considering the data are generally cross-sectional, we are looking at data of people who are sick at that time (and not going back into time to see what made them sick in the first place). Why does this matter? Well, there’s always a chance that the sicker people are thinner due to the wasting that can be associated with severe chronic disease. So, it may not be the low BMI that is causing death, but rather these folk were doing poorly health-wise anyways. And maybe they were smokers.
Using the Obesity Paradox in Goal Setting
When we look at the entire body of evidence as a whole, we can state that there is certainly strong evidence that excess adiposity has a protective effect, at least in some individuals. While I think the obesity paradox criticisms are merited, it doesn’t cancel out the epidemiological effect seen on upwards of millions of data points. That’s a big deal, and very robust science!
Perhaps the conclusion in terms of using the obesity paradox to set weight loss goals is that there may be the most benefits to walking the line between normal weight and overweight. Recall that for a 35-year old woman, a normal BMI on average translates to a body fat percentage between 22% and 31%. Being overweight would translate, on average, to a body fat percentage between 31% and 38%. The “sweet spot” in terms of lower disease risk associated with being a normal weight and the protective benefits of some adiposity may be seen at the higher end of the normal weight range, i.e., say 27% to 31% body fat (again, assuming you’re a 35-year old woman). Yes, that means not fighting to lose that last 10 pounds and cut to the point of ripped muscles and 6-pack abs.
Set Point Theory & Weight Loss Goals: Treading with Caution When Necessary
 There is a final piece to the puzzle that I would like to discuss before we wrap up this series: body weight set point theory. This is another one of those concepts in which a lot of misconceptions exist. Set point theory is the long-standing argument that the body has a naturally-preferred weight, or “set point,” and it will facilitate physiological and behavioral changes (more hunger, food being more palatable, less thyroid hormone/slower metabolism) to maintain that weight when we attempt to lose it.
There is a final piece to the puzzle that I would like to discuss before we wrap up this series: body weight set point theory. This is another one of those concepts in which a lot of misconceptions exist. Set point theory is the long-standing argument that the body has a naturally-preferred weight, or “set point,” and it will facilitate physiological and behavioral changes (more hunger, food being more palatable, less thyroid hormone/slower metabolism) to maintain that weight when we attempt to lose it.
It appears that the set point exists every 30lbs or so, which is one theory as to why weight loss plateaus are so common. So, if our bodies are trying to maintain some set weight, are we “supposed” to tweak it? Unfortunately for us, our bodies have become confused by the inputs of excess that we give them with a standard American diet. The additives included in most processed foods trick the brain into establishing a higher set point (yes, this is very concerning). This makes eating real food absolutely essential during a weight loss attempt.
This issue, especially as someone who has lost a significant amount of weight and maintained that loss, always puzzles me just a bit. The psychological impact of weight loss can be all-consuming; many people going through some weight loss journey report some obsessive thoughts, either about the loss itself or about food, eating, or exercise (I have also been there). That is one of the reasons why I suggest maintaining a Paleo diet that is tuned to weight loss and portion control rather than a pure calories-in, calories-out model (see Healthy Weight Loss with Paleo, Part 1: Modifying Dietary Choices to Support Fat Metabolism but also New Scientific Study: Calories Matter and 10 Nutrients that Can Help You Burn Fat). That being said, I will always encourage someone with a disordered eating history to work through their psychological traumas first and put weight loss aside until they are able to make healthy goals.
Also of note is that weight cycling, especially in the realm of more than one set point (over 30lbs) should be avoided at all cost. Studies have demonstrated that an inconsistent lifestyle (i.e., yo-yo dieting), results in weight gain over time. You’ve probably heard that statistic that most people regain the weight plus 10% after just a few years, and that’s actually pretty muddy. In fact, some research suggests that weight fluctuation is a normal part of yearly cycles – but not fluctuations of 30, 50, or 100+ lbs! That being said, long-term restriction and yo-yo dieting does influence our basal metabolic rate, making it more difficult to impact our weight every time we try to lose it.
The solution? Set a reasonable goal for weight loss. Make a plan that includes all of the steps I’ve included in this series. Stick with the plan until a reasonable body composition goal is met. Refer to Part 3 if you experience weight loss resistance. Maintain a healthy lifestyle after your goal is met.
Part of why I have dedicated so much time to this resource is that I want to give my readers the tools to succeed in the long-term (and there aren’t any studies about long-term weight loss and Paleo, but I am clearly optimistic about it). Referring to the guidelines included in this series isn’t a guarantee, but it is a top-notch start.
Putting It All Together: The Wonders of Body Fat
So how can we use our understanding of body composition, the obesity paradox and set point theory to inform our weight loss goals?
Fat Loss vs Muscle Loss
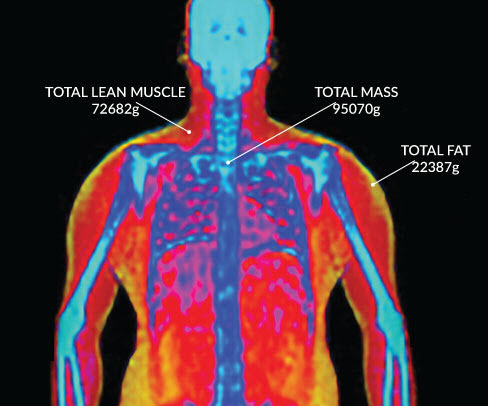 One reason to keep track of body fat is the commonly-mentioned by not-always-understood concept that weight loss almost always includes some muscle loss as well. In fact, one of the most common reasons that someone might be hesitant to lose weight is sacrificing muscle strength or “gains” in the gym (and I totally feel you! I love weightlifting). It’s true: the body is unlikely to participate in both catabolism (breaking down) of stored body fat while also participating in anabolism (building up) of muscle. This is controlled in part by the symphony of hormones that guide our metabolism and drive (like the drive to sleep, etc.). The hormones that promote fat loss are catabolic, while the hormones that promote muscle building are anabolic. When we create a caloric deficit, the body uses what it can to make energy: fat, carbohydrate, and – you guessed it – protein. Where does endogenous protein come from? The body uses the protein (broken down into amino acids) from muscles first, in addition to the proteins made in the liver. These amino acids are stripped of their carbon atoms and used to create energy in the citric acid cycle. In the end, this is a relatively small fraction of our energy metabolism, but the result is going to be some muscle loss in addition to fat loss in almost everyone working to lose weight.
One reason to keep track of body fat is the commonly-mentioned by not-always-understood concept that weight loss almost always includes some muscle loss as well. In fact, one of the most common reasons that someone might be hesitant to lose weight is sacrificing muscle strength or “gains” in the gym (and I totally feel you! I love weightlifting). It’s true: the body is unlikely to participate in both catabolism (breaking down) of stored body fat while also participating in anabolism (building up) of muscle. This is controlled in part by the symphony of hormones that guide our metabolism and drive (like the drive to sleep, etc.). The hormones that promote fat loss are catabolic, while the hormones that promote muscle building are anabolic. When we create a caloric deficit, the body uses what it can to make energy: fat, carbohydrate, and – you guessed it – protein. Where does endogenous protein come from? The body uses the protein (broken down into amino acids) from muscles first, in addition to the proteins made in the liver. These amino acids are stripped of their carbon atoms and used to create energy in the citric acid cycle. In the end, this is a relatively small fraction of our energy metabolism, but the result is going to be some muscle loss in addition to fat loss in almost everyone working to lose weight.
Science has investigated how this anabolic-catabolic dynamic impacts weight loss, and there are a couple quick take-home messages from the literature:
- Just because weight loss results in some modest muscle loss, we shouldn’t skip resistance training. As I mentioned in Part 2 of this series, which focused on lifestyle, incorporating a variety of movements is essential when it comes to weight loss – this doesn’t just impact our caloric deficit but also helps to preserve our muscle mass. Combined with the fact that muscle burns more energy throughout the day compared to muscle (meaning that having more muscle increases our basal metabolic rate), we know that resistance training is an absolute must when attempting weight loss!
- Adjusting goals to be within a moderate range are best for our muscles and our minds! Studies show that extreme, rapid weight loss – and even just speedy weight loss, greater than two pounds per week – may accelerate muscle loss and have an impact on the amount of muscle we lose. This includes both extreme calorie restriction and weight loss surgery. Plus, there’s mental/emotional and hormonal detriments of such rapid weight loss. So, setting the goal of less than 2 pounds per week, knowing there might be some variance from week to week, is the “right” pace for most people.
It’s also important not to freak out about losing some muscle! The great thing about the human body is that we are perfectly capable of building more muscle after reaching our target body fat percentage. The purpose of reviewing this information is to clarify why making gains in the gym might be harder during weight loss– and why we should still lift weights anyways!
What About Water Weight?
 Another term that is thrown around a lot in the weight loss community is “water weight.” As in, “you might lose a lot of weight fast, but that’s just water weight.” What does this phrase actually mean? Water weight is the presence of excess water that the body retains, in a variety of ways. Water is generally bound to muscle and liver glycogen, so use of glycogen stores results in loss of this water weight. Our bodies might hold onto some extra water if we consume too much salt or sugar (both of which are tough to do with a Paleo lifestyle, but it happens!), or it might be indicative of a hormonal imbalance in women (or just that time of the month). People can easily retain 10 or more pounds of water, depending on their lifestyle and habits.
Another term that is thrown around a lot in the weight loss community is “water weight.” As in, “you might lose a lot of weight fast, but that’s just water weight.” What does this phrase actually mean? Water weight is the presence of excess water that the body retains, in a variety of ways. Water is generally bound to muscle and liver glycogen, so use of glycogen stores results in loss of this water weight. Our bodies might hold onto some extra water if we consume too much salt or sugar (both of which are tough to do with a Paleo lifestyle, but it happens!), or it might be indicative of a hormonal imbalance in women (or just that time of the month). People can easily retain 10 or more pounds of water, depending on their lifestyle and habits.
All of this to say that significant changes in weight on the scale can easily be chalked up to water retention or loss – something to keep in mind is vigilance when it comes to weighing oneself. Some people like to step on the scale daily, and others prefer weekly or biweekly; my biggest suggestion is to figure out what works for you and stick with it including always weighing yourself at the same time of day, knowing that there might be fluctuations if you tend toward the daily measurements.
Is there a “Right Rate” of Weight Loss?
There is one more point that I have not had the opportunity to mention yet that I wanted to make sure to include in this series. There is a lot of discussion that weight loss should occur at a healthy pace of perhaps 1-2 pounds per week. Why? In part, because of the metabolic factors that I listed above. Namely, starvation diets that result in significant weight loss per week (3+ pounds) result in higher rates of muscle wasting and may trigger metabolic changes that conserve adipose and lower basal metabolic rate (how many calories we would burn if we just hung out in our beds all day and didn’t move). However, there is mixed evidence when we turn to the literature; for example, one study of 200 people found that rapid weight loss and gradual weight loss did not differ in their rate of weight regain after nearly 3 years – but they did find that the rapid weight loss group had more adverse events (notably, gallbladder stones and infection. This is a known effect of rapid weight loss, though). For that reason alone, it might be worthwhile to avoid rapid weight loss; at the least, one of those adverse side effects could offset a lot of your hard work!
Setting Target Weight Goals
While this is still a field of science in which new papers are released daily that add to our understanding, there seems to be strong evidence that aiming to have a body fat percentage in the higher end of the normal range is best of overall lifelong health. You can calculate what that means for you using the following formula:
Body fat % = (1.39 x BMI) + (0.16 x age) – (10.34 x gender) – 9
with gender equal to 1 for men and 0 for women. Although, this still represents a best guess based on current evidence, calculate your lower body fat percentage target with a BMI of 23 and your upper limit with a BMI of 25. Remember that your weight and body composition aren’t the only metrics of health. And of course, the advice of your healthcare provider always trumps this type of information.
Wrapping Up Weight Loss
Weight loss is an incredibly rewarding, challenging, and controversial endeavor – and with this post, we managed to dig through a lot of science. Fortunately or not, this topic is a reminder that sometimes, the science isn’t clear-cut. So, what do we do with this information and how do we move away from this series feeling content in our evidence-based lifestyle?! Well, there are a couple of major lessons to take away here:
- Not all measures of body composition are equal! If possible, start with the best available measure of composition and check in regularly to keep track of your progress.
- Aiming for the lowest body fat percentage isn’t going to do us all a disservice, but it’s likely not the best goal for most. Taking personal health history, natural set point, and aesthetic all into consideration is essential for long term success and happiness.
- An anti-inflammatory diet that tackles the obesity-insulin resistance-inflammation cycle is our best bet to tackle this physiologically-challenging state and maintain our results.
Wow, I’ve written about this all so much that it’s hard to believe that this series is over. What I can promise is that I’ll continue to keep an eye on the literature – because science is always changing! – and update these posts (or write more) as needed. Always keep me updated on your weight loss journeys in the comments below!
Citations
Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, Moore SC, Tobias GS, Anton-Culver H, Freeman LB, Beeson WL, Clipp SL, English DR, Folsom AR, Freedman DM, Giles G, Hakansson N, Henderson KD, Hoffman-Bolton J, Hoppin JA, Koenig KL, Lee IM, Linet MS, Park Y, Pocobelli G, Schatzkin A, Sesso HD, Weiderpass E, Willcox BJ, Wolk A, Zeleniuch-Jacquotte A, Willett WC, Thun MJ (2010). “Body-mass index and mortality among 1.46 million white adults”. The New England Journal of Medicine. 363 (23): 2211–9. doi:10.1056/NEJMoa1000367. PMC 3066051 . PMID 21121834.
Calabro P, Yeh ET. Obesity, inflammation, and vascular disease: the role of the adipose tissue as an endocrine organ. Subcell Biochem. 2007;42:63-91.
Cao, Chao; Wang, Ran; Wang, Jianmiao; Bunjhoo, Hansvin; Xu, Yongjian; Xiong, Weining; Simpson, Colin (24 August 2012). “Body Mass Index and Mortality in Chronic Obstructive Pulmonary Disease: A Meta-Analysis”. PLoS ONE. 7 (8): e43892. doi:10.1371/journal.pone.0043892.
Chrysant, Steven G.; Chrysant, George S. (January 2013). “New insights into the true nature of the obesity paradox and the lower cardiovascular risk”. Journal of the American Society of Hypertension. 7 (1): 85–94. doi:10.1016/j.jash.2012.11.008.
Diercks, Deborah B.; Roe, Matthew T.; Mulgund, Jyotsna; Pollack, Charles V.; Kirk, J. Douglas; Gibler, W. Brian; Ohman, E. Magnus; Smith, Sidney C.; et al. (2006). “The obesity paradox in non–ST-segment elevation acute coronary syndromes: Results from the Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the American College of Cardiology/American Heart Association Guidelines Quality Improvement Initiative”. American Heart Journal. 152 (1): 140–8. doi:10.1016/j.ahj.2005.09.024. PMID 16824844.
Habbu, Amit; Lakkis, Nasser M.; Dokainish, Hisham (2006). “The Obesity Paradox: Fact or Fiction?”. The American Journal of Cardiology. 98 (7): 944–8. doi:10.1016/j.amjcard.2006.04.039. PMID 16996880.
Harrington, Mary; Gibson, Sigrid; Cottrell, Richard (2009). “A review and meta-analysis of the effect of weight loss on all-cause mortality risk.”. Nutr Res Rev. 22 (1): 93–108. doi:10.1017/S0954422409990035. PMID 19555520.
Knuth ND, Johannsen DL, Tamboli RA, et al. Metabolic adaptation following massive weight loss is related to the degree of energy imbalance and changes in circulating leptin. Obesity (Silver Spring). 2014;22(12):2563-9.
Müller MJ, Bosy-westphal A, Heymsfield SB. Is there evidence for a set point that regulates human body weight?. F1000 Med Rep. 2010;2:59.
Niedziela, J; Hudzik, B; Niedziela, N; Gąsior, M; Gierlotka, M; Wasilewski, J; Myrda, K; Lekston, A; Poloński, L; Rozentryt, P (November 2014). “The obesity paradox in acute coronary syndrome: a meta-analysis.”. European Journal of Epidemiology. 29 (11): 801–12. doi:10.1007/s10654-014-9961-9. PMC 4220102. PMID 25354991.
Oreopoulos, Antigone; Padwal, Raj; Kalantar-Zadeh, Kamyar; Fonarow, Gregg C.; Norris, Colleen M.; McAlister, Finlay A. (2008). “Body mass index and mortality in heart failure: A meta-analysis”. American Heart Journal. 156 (1): 13–22. doi:10.1016/j.ahj.2008.02.014. PMID 18585492.
Padwal, R; McAlister, F A; McMurray, J J V; Cowie, M R; Rich, M; Pocock, S; Swedberg, K; Maggioni, A; Gamble, G; Ariti, C; Earle, N; Whalley, G; Poppe, K K; Doughty, R N; Bayes-Genis, A (31 October 2013). “The obesity paradox in heart failure patients with preserved versus reduced ejection fraction: a meta-analysis of individual patient data”. International Journal of Obesity. 38 (8): 1110–1114.
Philip B. Maffetone, Ivan Rivera-Dominguez, Paul B. Laursen. Overfat and Underfat: New Terms and Definitions Long Overdue. Frontiers in Public Health, 2017; 4 DOI: 10.3389/fpubh.2016.00279
Prentice AM, Jebb SA, Goldberg GR, et al. Effects of weight cycling on body composition. Am J Clin Nutr. 1992;56(1 Suppl):209S-216S.
Purcell K, Sumithran P, Prendergast LA, Bouniu CJ, Delbridge E, Proietto J. The effect of rate of weight loss on long-term weight management: a randomised controlled trial. Lancet Diabetes Endocrinol. 2014;2(12):954-62.
Schmidt, Darren S.; Salahudeen, Abdulla K. (2007). “CARDIOVASCULAR AND SURVIVAL PARADOXES IN DIALYSIS PATIENTS: Obesity-Survival Paradox-Still a Controversy?”. Seminars in Dialysis. 20 (6): 486–92. doi:10.1111/j.1525-139X.2007.00349.x. PMID 17991192.
Sharma, A; Lavie, CJ; Borer, JS; Vallakati, A; Goel, S; Lopez-Jimenez, F; Arbab-Zadeh, A; Mukherjee, D; Lazar, JM (15 May 2015). “Meta-analysis of the relation of body mass index to all-cause and cardiovascular mortality and hospitalization in patients with chronic heart failure.”. The American journal of cardiology. 115 (10): 1428–34.
Stout MB, Justice JN, Nicklas BJ, Kirkland JL. Physiological Aging: Links Among Adipose Tissue Dysfunction, Diabetes, and Frailty. Physiology (Bethesda). 2017;32(1):9-19.
Veronese, N; Cereda, E; Solmi, M; Fowler, SA; Manzato, E; Maggi, S; Manu, P; Abe, E; Hayashi, K; Allard, JP; Arendt, BM; Beck, A; Chan, M; Audrey, YJ; Lin, WY; Hsu, HS; Lin, CC; Diekmann, R; Kimyagarov, S; Miller, M; Cameron, ID; Pitkälä, KH; Lee, J; Woo, J; Nakamura, K; Smiley, D; Umpierrez, G; Rondanelli, M; Sund-Levander, M; Valentini, L; Schindler, K; Törmä, J; Volpato, S; Zuliani, G; Wong, M; Lok, K; Kane, JM; Sergi, G; Correll, CU (November 2015). “Inverse relationship between body mass index and mortality in older nursing home residents: a meta-analysis of 19,538 elderly subjects.”. Obesity Reviews. 16 (11): 1001–15. doi:10.1111/obr.12309. PMID 26252230.
Wang, L; Liu, W; He, X; Chen, Y; Lu, J; Liu, K; Cao, K; Yin, P (4 September 2015). “Association of overweight and obesity with patient mortality after acute myocardial infarction: A meta-analysis of prospective studies.”. International journal of obesity (2005). 40: 220–8. doi:10.1038/ijo.2015.176. PMID 26338077.