Along with saturated fat, few nutrients have gotten as much flack over the years as a certain essential mineral: sodium! Or more specifically, salt (sodium chloride), the most abundant source of sodium in most people’s diets.
Table of Contents[Hide][Show]
- The Importance of Salt
- Salt and Blood Pressure
- Salt and Kidney Function
- Salt, Inflammation and Autoimmune Disease
- Salt and Cancer
- But, Is Salt Paleo?
- Should You Still Worry About Eating Too Much Salt?
- If Low-Sodium is Good, Is No-Sodium Better?
- How Do You Know if You Need More Salt?
- The Benefits of Unrefined Salt
- The Verdict?
- Citations
 Far from a newcomer on the menu, salt has been mined (and cherished) for thousands of years across the globe. It was once so valuable that the Roman legions were paid with it (hence the word salary, which comes from the word salt!). In fact, we could even argue that salt made modern civilization possible: it gave us the ability to preserve food without refrigeration—allowing us to store (and trade) perishable items, prevent meat from rotting, travel long distances with a secure food supply, and release our dependence on seasonal eating. That’s a pretty impressive résumé for one little ionic compound, right?
Far from a newcomer on the menu, salt has been mined (and cherished) for thousands of years across the globe. It was once so valuable that the Roman legions were paid with it (hence the word salary, which comes from the word salt!). In fact, we could even argue that salt made modern civilization possible: it gave us the ability to preserve food without refrigeration—allowing us to store (and trade) perishable items, prevent meat from rotting, travel long distances with a secure food supply, and release our dependence on seasonal eating. That’s a pretty impressive résumé for one little ionic compound, right?
But, that hasn’t stopped salt from getting a bad rap in various health communities. Even opinions in the Paleo world are divided, with some leaders claiming salt is harmful and shouldn’t be considered Paleo.
And of course, the idea that salt raises blood pressure and contributes to disease risk is still a common belief. So, should you nix the salt in the name of health? Let’s evaluate the evidence!
The Importance of Salt
Salt has a remarkably simple molecular structure, being made predominantly of just two elements: sodium and chloride (in fact, pure salt is the molecule sodium chloride, NaCl).
Sodium is an essential nutrient: living in a moderate climate and not sweating very much, your body would need about 115 mg of it per day just to stay alive (the safe lower limit is generally given at 500 mg per day). It’s vital for cellular function, nutrient absorption in the digestive tract, kidney health, adrenal function, and cardiac health. And, because sodium is an electrolyte (a special type of mineral that carries an electrical charge), it also plays a role in maintaining a normal blood pH, regulating the amount of water in your body, conducting nerve impulses, and controlling muscle contractions (including those of your heart!).
Salt isn’t just made of sodium. While “low-sodium diet” has reached buzzword status, it’s important to also discuss the other half of the salt molecule: chloride. Chloride (the ionic form of chlorine, i.e., a single chlorine atom with a net electric charge due to the loss of an electron) is required for the production of hydrochloric acid in the stomach and is important for electrolyte balance, as well as fluid balance in the body. The effects of excess chloride have not been extensively studied (although you could argue that all studies that simply look at high salt intake are really looking at what happens when you eat both too much sodium and too much chloride). There’s an interesting interplay between chloride levels and potassium levels, which may explain some interesting effects of high chloride intake, such as increasing the hypertensive effects of high sodium intake, but also decreasing the kidney damage associated with high sodium.
The studies all point to sodium as being “the bad part” of salt, and that’s what I’ll be focusing on here. But, right off the bat, I encourage you to stop thinking of sodium (or salt) as an unconditional bad guy, and recognize its contribution to human health.
Salt and Blood Pressure
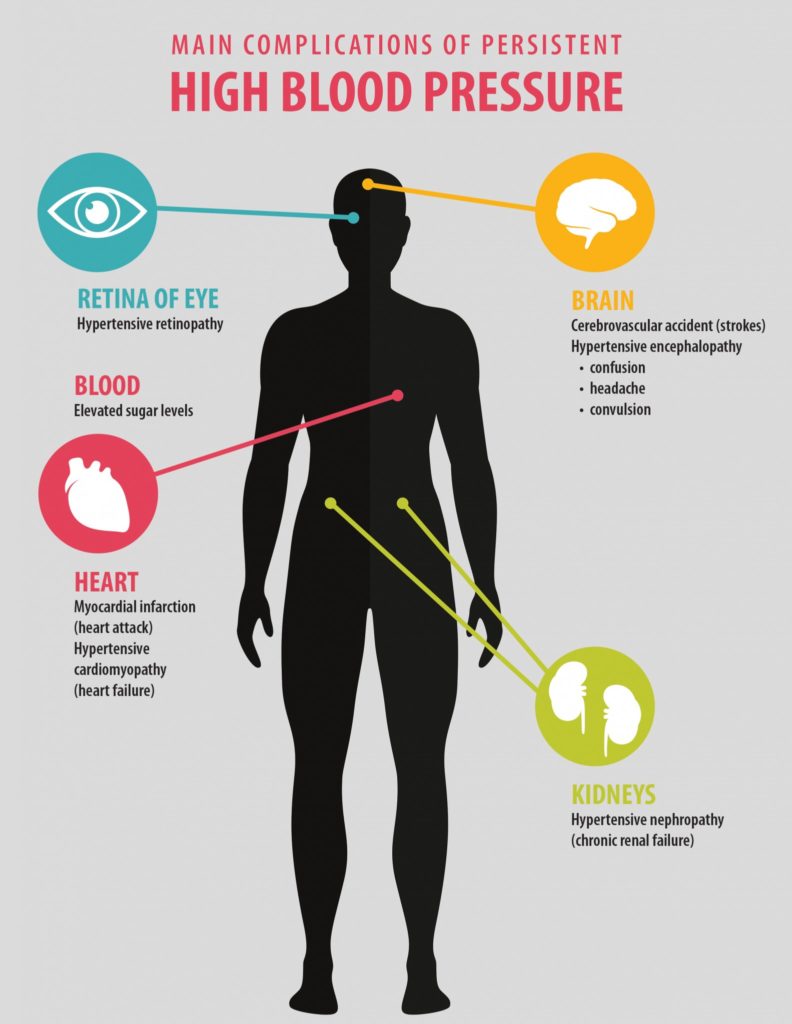
High blood pressure is a risk factor for disease, including the well-known link with cardiovascular disease (including heart disease, heart attack and stroke), but also hypertensive retinopathy, chronic renal failure, and even diabetes.
Nutrivore Weekly Serving Matrix
An easy-to-use and flexible weekly checklist
to help you maximize nutrient-density.
The Weekly Serving Matrix is very helpful! I’ve been eating along these lines but this really helps me know where to focus vs. which foods serve a more secondary role. It’s super helpful and has taken a lot of worry out of my meal planning. Thanks!
Jan
The most common criticism against salt is that too much of it raises blood pressure, in turn elevating your risk of having a heart attack or stroke. But, this isn’t exactly true! Research shows that sodium reduction only has a modest impact on blood pressure (and cardiovascular outcomes).
A 2014 Cochrane review (using eight different trials) found that salt restriction had no significant benefit for overall mortality, and only weak benefit for cardiovascular events and deaths. And, the researchers noted that the “benefit” was due almost entirely to a single trial of retirement home residents, which drove the results when all eight studies were pooled together. In fact, a 2011 Cochrane review on the same topic (using seven different studies) showed “no strong evidence of any effect of salt reduction” on cardiovascular disease mortality for either hypertensive people or people with normal blood pressure.
When we talk about minerals that influence blood pressure, sodium usually steals the spotlight. But, potassium also plays a significant role in regulating blood pressure and protecting against cardiovascular disease risk. For example, an analysis of 19 clinical trials found that potassium supplementation significantly reduces both systolic and diastolic blood pressure—to a greater degree than most salt-restriction trials show!
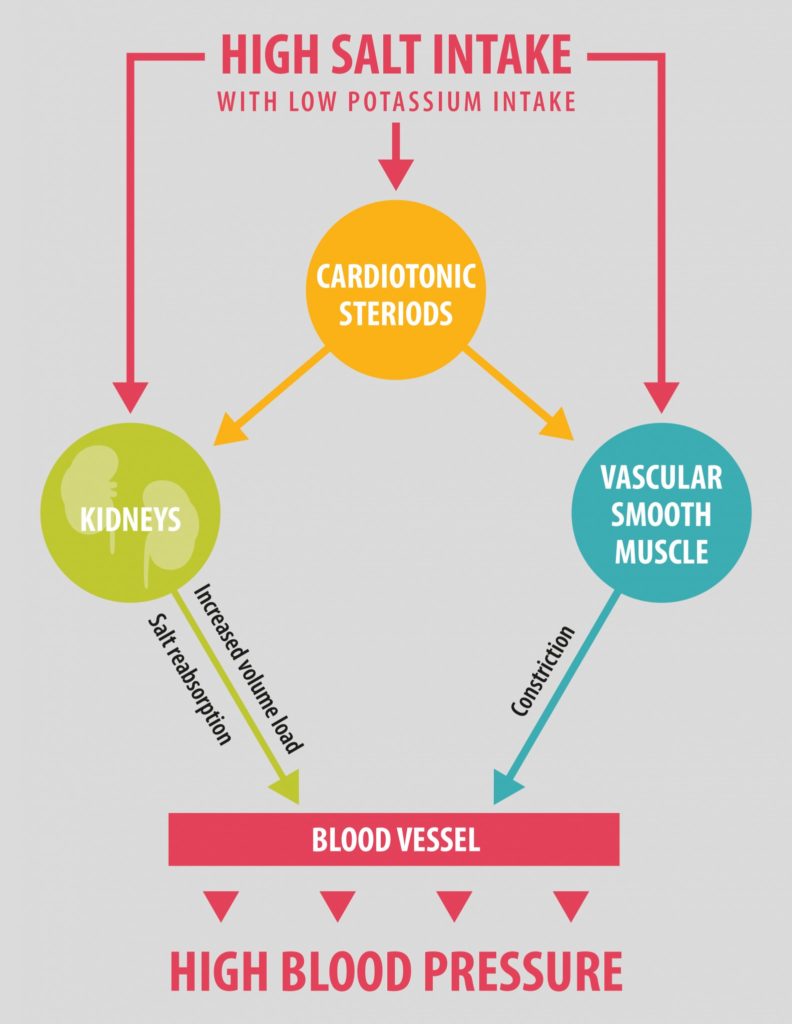
More recent research has confirmed that the sodium-to-potassium ratio may be more important than just sodium or potassium intake alone. A trio of papers in the New England Journal of Medicine in 2014 pointed towards an interaction between sodium and potassium, where higher sodium intake was mostly harmful in the presence of low potassium intake (as measured by excretion levels of both minerals). An editorial accompanying the papers summarized, “The authors suggested that the alternative approach of recommending high-quality diets rich in potassium might achieve greater health benefits, including blood-pressure reduction, than aggressive sodium reduction alone.”
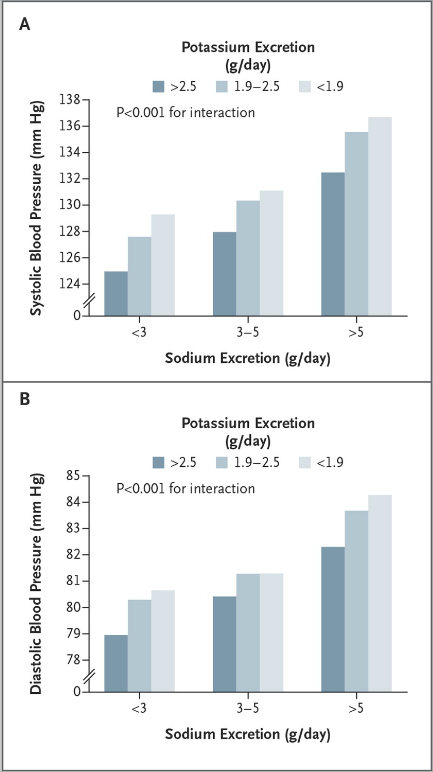 (Image from Mente, et al, 2014)
(Image from Mente, et al, 2014)
So, what foods have potassium? Here’s where eating a nutrient-dense Paleo diet comes in handy! A number of tasty plant foods are high in potassium, including:
 Beet greens
Beet greens- Tomatoes
- Avocados
- Sweet potatoes
- Bananas
- Potatoes
- Spinach
- Swiss chard
- Apricots
- Squash
- Broccoli
- Coconut water
Salt and Kidney Function
High salt intake has long been known to worsen kidney disease and there’s some evidence that high salt intake also increases risk for kidney disease in the first place. Why is there a link? The kidneys are responsible for maintaining the balance between water and electrolytes (like sodium!) in the body, as well as removal of water-soluble waste products from the body (which are excreted in urine). In the production of urine, the kidneys remove water from the blood via osmosis (meaning the water moves from an area of low concentration of electrolytes across a semi-permeable barrier of cells to an area of high concentration of electrolytes, sodium and potassium being especially important for regulating this filtration process). A high salt diet alters the gradient of sodium concentration, causing the kidneys to have reduced function and remove less water resulting in higher blood volume (and therefore pressure). Strain on the kidneys comes not just from hypertension and a reduced ability to perform its filtering job, but also from direct tissue damage from high sodium levels.
Contrary to what the high salt-kidney disease correlations would imply, long-term adoption of reduced salt diets (whether that’s defined as under 3g daily or under 5g daily) don’t improve mortality from or disease progression of chronic kidney disease. However, they do improve the response to several drug options for mitigating kidney disease, and are still a recommendable option for anyone battling established kidney problems.
Because kidney function has a direct effect on bone mineralization (due to acid/base balance), one would expect high salt intake (and therefore hindered kidney function) to be correlated to incidence of osteoporosis and/or hip fracture. However, even at intake levels of 9g per day, studies show no clear link between high salt intake and bone health.
Salt, Inflammation and Autoimmune Disease
High salt intake stimulates the immune system. Seminal research from 2013 revealed that the higher the concentration of salt in the diet, the greater the number of Th17 cells (a major culprit in autoimmune disease) that are activated and the greater the amount of proinflammatory cytokines that are secreted by those Th17 cells (causing generalized inflammation). In a study of mice with multiple sclerosis, mice that were fed a high-salt diet had significantly exacerbated symptoms, directly attributable to increases in Th17 cell differentiation (maturation), proliferation (division), and activation. Subsequent research showed that females are more susceptible to this effect than males (at least in mice).
Very recent research expands the link between high salt intake and inflammation by showing that high dietary salt also activates macrophages (resident immune cell sentinels present in nearly every tissue in the human body). It appears that high salt intake primes the immune system to attack. However, there is a paucity of human data. One recent study showed that high dietary salt intake increased risk of rheumatoid arthritis in smokers (but not non-smokers). And, asthmatics are more likely to have exercise-induced asthmatic attacks if they eat a high-salt diet, and see improvements in their symptoms with a low-sodium diet.
In people, high salt intake is considered above 9 grams per day (that’s 4 teaspoons of salt every day!). Importantly, these studies (both animal and human) don’t compare high salt intake against the absence of salt, but rather standard low-sodium recommendations (for humans, that’s 2.4g of salt, or 1 teaspoon, per day).
Salt and Cancer
Any factor that influences how the immune system works is also a candidate for increasing cancer risk. Some research does suggest that cancer incidence rises with very high salt intake—and this is especially true of stomach (gastric) cancer. For instance, a meta-analysis of seven prospective studies, encompassing almost 270,000 people, found that “high” and “moderately high” salt intakes were both associated with significantly increased risk of stomach cancer over the span of at least four years of follow-up.
What explains this association? As it turns out, salt can play multiple roles in the etiology of stomach cancer. First, it tends to affect both the risk and the outcome of H. pylori infection (a bacteria that grows in the intestinal tract and can attack the stomach lining), which is a major risk factor for stomach cancer. Mucosal damage from salt can increase the susceptibility to H. pylori infection, and H. pylori reacts to high-salt environments with an increase in growth, cell morphology, survival, and virulence—all of which result in a more aggressive infection that becomes an even stronger promoter of stomach cancer. In addition, rodent models show that for cagA+ H. pylori strains (CagA, or cytotoxin-associated gene A, is a bacterial oncoprotein that can bind to proteins and deregulate them thus potentially causing cancer), a high-salt diet leads to increased expression of interleukin 1β in gastric cells, more severe stomach inflammation, higher gastric pH, and an upregulation of CagA synthesis—all of which suggest a high-salt diet increases the carcinogenic effects of certain H. pylori strains.
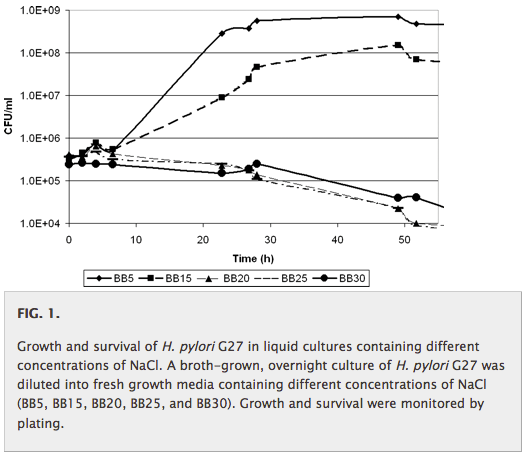 (Image from Gancz, et al., 2008)
(Image from Gancz, et al., 2008)
Apart from the role of H. pylori, salt can increase stomach cancer risk through two other avenues: increasing exposure to gastric carcinogens such as nitrates, and causing inflammation that leads to increased cell proliferation and mutation (which boosts the risk of cancer developing). This happens because a high salt intake can alter the quality of the stomach’s mucous barrier, leading to direct exposure to harmful compounds and also making the stomach more susceptible to mucosal damage.
There’s some evidence that a high salt intake can increase overall cancer risk as well. For instance, a 2015 study found that older men who reported “always” adding salt to their food were 20% more likely to die of cancer-related causes over the course of a 12.5-year (on average) follow-up, compared to men who reported “never” adding salt to their food. In absolute terms, 21.3% of men who always added salt and 16.8% of men who never salted their food died of cancer-related causes by the end of the study.
 (Image from Golledge, et al, 2015)
(Image from Golledge, et al, 2015)
(Although the researchers tried to adjust for confounders, we can’t rule out the possibility that the men who never added salt to their food had other protective dietary or lifestyle factors working in their favor.)
Theoretically, a reason salt could increase overall cancer risk involves its effects on intracellular electrolytes and pH. In several studies (such as this one), dietary salt loading increased intracellular sodium and calcium, decreased intracellular potassium and magnesium, and lowered intracellular pH—all factors that may support cancer progression.
 (Image from Resnick, et al., 1994)
(Image from Resnick, et al., 1994)
But, as always, context matters! Note that all of these correlations are with high salt intake. And, these effects are highly dependent on the level of other electrolytes in the diet. For example, although salt loading can decrease intercellular pH, potassium loading has been shown to increase it (thus counteracting the potential pro-cancer effects from the salt). Likewise, the sodium/potassium and calcium/magnesium ratios will vary based on the dietary intake of all minerals involved, not just sodium from salt.
And, another component of salt (iodine, found in large amounts in iodized salt and in smaller amounts in unrefined salts) may actually reduce the risk of thyroid cancer. So, the relationship between salt intake and cancer is highly context-dependent, and more complex than first meets the eye.
But, Is Salt Paleo?
In general, the question “Is it Paleo?” is less important than the question, “Is this item beneficial for human health?” Looking at our evolutionary diet is a great place to start when forming theories about what’s best for our bodies, but it’s not until we perform controlled trials, mechanistic studies, and other forms of structured science that we can really evaluate the healthfulness of different foods. (And in the case of salt, those studies fail to show that it’s harmful at normal levels of intake!)
That being said, some voices in the health community have claimed that salt “isn’t Paleo,” and that early humans (or any other land animals, for that matter) wouldn’t have consumed it. So, it’s still worth assessing this claim.
While there’s no evidence that early humans actively mined and collected salt in the way we do today (the oldest salt mine dates back about 6500 years), chances are good that salt was available and at least occasionally consumed. One clue comes from wild animals. As it turns out, a huge variety of creatures—including moose, African elephants, mountain goats, deer, bats, woodchucks, squirrels, porcupines, tapirs, and a number of non-human primates—regularly flock to mineral licks (AKA deposits of salt and other minerals) to supplement their diets with sodium and other nutrients. (Herbivores in particular seek out salt licks for supplementary sodium, because inland plant foods generally don’t supply enough of it to meet their nutritional needs.) Mineral licks also contain smaller amounts of other nutrients (like phosphorus, magnesium, selenium, calcium, magnesium, and manganese) that can improve the nutritional quality of a diet.
 (Wild Indian bison at a salt lick)
(Wild Indian bison at a salt lick)
What does that mean for humans? While it’s possible that we’re one of the few mammals that never capitalized on salt licks when we encountered them in the wild, it seems unlikely. For one, we have evidence that Paleolithic humans scavenged mammoth bones from natural salt licks (where mammoths flocked!), so we clearly interacted with salt-rich areas in the past.
Likewise, given the tendency for early humans to cluster around coastal and other aquatic regions, salt from the water probably made it onto our menu unintentionally. There’s evidence that, when near the coast, Paleolithic man ate seaweed, which is rich in salt and other valuable minerals. Even natural freshwater sources (lakes, rivers, streams, etc.) contain some salt, some as much as 0.4% salt (which is quite a lot especially knowing that the ocean is only about 9 times higher at 3.5% salt!). We might not have had access to as much salt as we do today, but salt was definitely present in the Paleolithic era!
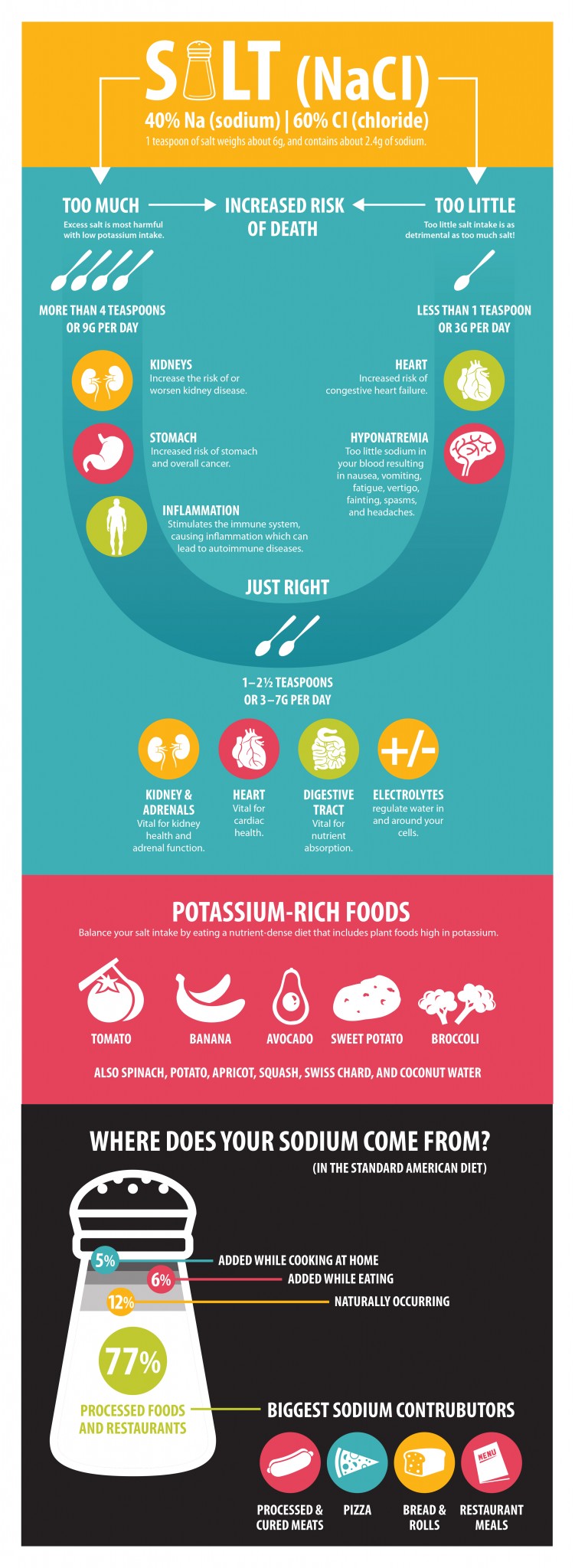
Should You Still Worry About Eating Too Much Salt?
It’s true that in studies of salt consumption mentioned earlier, very high intakes were associated (albeit modestly, in most cases) with higher risk of certain cardiovascular events, cancer and death. But, how high is too high? A recent survey across all European Member States (plus Norway and Switzerland) showed that daily sodium consumption is between 8 and 12 g/day, and these are the levels in which we start to see statistically significant correlations between salt intake and health problems in large epidemiological studies. The cusp for negative health impacts of sodium (in the context of the Standard American Diet, since effects of high salt intake has never been studied in more nutrient-dense [potassium-rich] anti-inflammatory diets, like the Paleo diet), is about 7g of sodium per day. What people are consuming on average, 3-4 teaspoons of salt per day, is way higher than the World Health Organization recommended target of 5–6 g of sodium per day and way, way higher the low-sodium diet target of 3g/day. At these more modest amounts of 1-2 teaspoons per day, salt consumption is not linked to health problems.
Chemistry aside: table salt is roughly 40% sodium by weight and 60% chloride by weight. So, it works out that there’s about 2.4g of sodium in 1 teaspoon of salt (which weighs about 6g). Unrefined salt has less sodium per teaspoon (thanks to sodium being displaced by other minerals), but it varies.
And, if you’re eating Paleo, you probably don’t need to obsessively monitor the salt shaker. Here’s why:
For people eating the Standard American Diet (the population studied in many of the salt trials we have), the biggest source of salt is processed foods. In fact, according to the Centers for Disease Control and Prevention, the three biggest sodium contributors in America are bread/rolls, processed and cured meats, and pizza (not exactly Paleo staples!). Over 75% of the sodium most people eat comes from prepackaged foods, processed store-bought foods, and restaurant meals. By contrast, only 11% of dietary sodium comes from salt added at home (during cooking OR at the table). If you do the math, that automatically puts anyone who cooks their own food from whole food ingredients in a low-sodium diet category.
 When you ditch the heavily processed, low-nutrient foods dominating most Western diets, your salt intake will naturally go way down (and as you eat more tasty vegetables and fruits, your potassium intake will tend to go up!). And, as your taste buds adjust to the more diverse and subtle flavors of whole plant and animal foods, you may find yourself wanting to add less salt to your meals than you used to. In other words, it’s pretty hard to eat dangerous levels of salt on a Paleo diet unless you really try! Most of us naturally find ourselves easily under 3-5g of sodium per day.
When you ditch the heavily processed, low-nutrient foods dominating most Western diets, your salt intake will naturally go way down (and as you eat more tasty vegetables and fruits, your potassium intake will tend to go up!). And, as your taste buds adjust to the more diverse and subtle flavors of whole plant and animal foods, you may find yourself wanting to add less salt to your meals than you used to. In other words, it’s pretty hard to eat dangerous levels of salt on a Paleo diet unless you really try! Most of us naturally find ourselves easily under 3-5g of sodium per day.
If Low-Sodium is Good, Is No-Sodium Better?
Separate from the question of whether or not caveman sprinkled salt on their mammoth steaks (we all know how I feel about health recommendations made solely on the presumptions of what Paleolithic man did or did not eat), it’s an important question to answer. Since studies show benefits from salt intake at about 3g daily, does that mean that giving up salt altogether will make us even healthier?
As it turns out, eating too little salt can actually be just as detrimental as eating too much! Bold, for emphasis. We find this time and time again with nutrients, there’s a happy medium in which we thrive and both too much and too little cause problems.
Research has actually shown that restricting salt too much can increase risk of death. Another 2014 meta-analysis found that salt intake and mortality formed a U-shaped curve, with all-cause mortality increasing with both very low salt intake and very high salt intake.
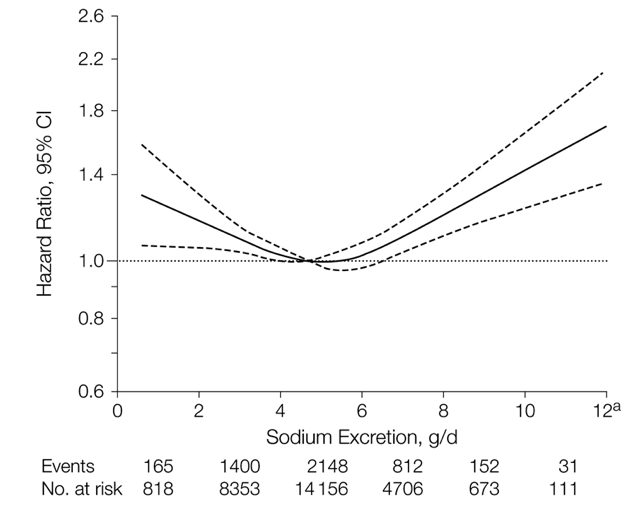 (Image from O’Donnell, et al, 2011)
(Image from O’Donnell, et al, 2011)
And a 2011 study that analyzed sodium excretion (a more accurate way to assess people’s sodium intake than recall surveys and food-frequency questionnaires) found that sodium excretion of more than 7g per day or less than 3g per day were both associated with worse health outcomes (in the case of less than 3g, higher rates of cardiovascular death and hospitalization for congestive heart failure). Yikes!
How Do You Know if You Need More Salt?
When you think of 3g per day being a minimum healthful amount of salt to consume, this raises some whole new questions in the context of a whole foods diet like the Paleo diet. While most people eating the Standard American Diet won’t have to worry about their salt intake dipping too low, this can actually be a problem for people who eliminate processed and pre-packaged foods from their diet and don’t use much salt while cooking (which can definitely include Paleo adherents)!
Hyponatremia is the technical term for having too little sodium in your blood, and it can result in symptoms such as nausea and vomiting, confusion, fatigue, muscle weakness, spasms, vertigo, fainting and headaches. Hyponatremia becomes even more likely if you’re also heavily sweating (from heat or exercise), if you’re sick and losing fluids through vomiting or diarrhea, if you have an underactive thyroid, or if you’re taking diuretics or certain antidepressant medications. Worst of all, hyponatremia can be life-threatening if left untreated—making it imperative to watch out for early symptoms!
To lower your risk of hyponatremia on a Paleo diet, it’s best to consume some salt (rather than none).
The Benefits of Unrefined Salt
Although regular table salt is unlikely to be harmful in moderate amounts, you can get even more benefits by opting for unrefined salts—like Himalayan Pink Salt or “dirty” (French sel gris, or Celtic) sea salt—that contain naturally occurring trace minerals. Although exact micronutrient content varies between different types of unrefined salt (depending on where they were mined from), Himalayan Pink Salt, for one example, contains 84 minerals—including magnesium, calcium, chromium, manganese, iron, potassium, copper, zinc, cobalt, selenium, bromine, strontium, molybdenum, iodine, sulfur, phosphorus, scandium, and literally dozens of others.
 Although I’m a huge proponent of getting nutrition from whole foods, it’s also true that hunter-gatherers (both ancient and still existing) had a much higher micronutrient intake than most of us do today. Nutrient depletion in farmed soils, less access to truly wild/nutrient-dense plant foods, consumption of produce that’s been transported long distances and picked prematurely, and a variety of other factors all result in us having less nutritious food at our disposal, even when we’re eating the best of the best. In addition, hunter-gatherers typically consumed some dirt with their food—which might sound gross, but it’s another source of micronutrients (and probiotics!) we’ve lost from our diets due to greater cleanliness and food washing!
Although I’m a huge proponent of getting nutrition from whole foods, it’s also true that hunter-gatherers (both ancient and still existing) had a much higher micronutrient intake than most of us do today. Nutrient depletion in farmed soils, less access to truly wild/nutrient-dense plant foods, consumption of produce that’s been transported long distances and picked prematurely, and a variety of other factors all result in us having less nutritious food at our disposal, even when we’re eating the best of the best. In addition, hunter-gatherers typically consumed some dirt with their food—which might sound gross, but it’s another source of micronutrients (and probiotics!) we’ve lost from our diets due to greater cleanliness and food washing!
For these reasons, unrefined salt can be valuable for the trace minerals it provides, helping us achieve an intake that’s more optimal for our health. Another great option is seaweed flakes, which are also rich in many minerals and a great natural source of salt. You can also keep it super simple with combo unrefined salt and seaweed flakes!
The Verdict?
So, should you stop eating salt? The answer is definitely no! As long as you’re eating a moderate amount (3 to 7 grams of sodium per day, about 1 to 2.5 teaspoons of salt per day), are consuming a wide variety of potassium-rich foods (magnesium and calcium too!), and are choosing good quality salts for the extra trace minerals, there’s no reason to avoid salt (or actively worry about consuming too much). The literature reinforces the fact that salt and health risk form a U-shaped curve, with too little being just as harmful as too much. Your best bet is to keep some in your diet and enjoy both the flavor and micronutrient boost it gives your food!
Citations
Adler AJ, et al. “Reduced dietary salt for the prevention of cardiovascular disease.” Cochrane Database Syst Rev. 2014 Dec 18;12:CD009217.
Ares GR & Ortiz PA. “Direct Renal effects of a fructose-enriched diet: interaction with high salt intake.” Am J Physiol Regul Integr Comp Physiol. 2015 Oct 7
Boero R, et al. “Salt intake and kidney disease.” J Nephrol. 2002 May-Jun;15(3):225-9.
Burger H. “Osteoporosis and salt intake.” Nutr Metab Cardiovasc Dis. 2000 Feb;10(1):46-53.
Cappuccio FP & MacGregor GA. “Does potassium supplementation lower blood pressure? A meta-analysis of published trials.” J Hypertens. 1991 May;9(5):465-73.
Cohen AJ & Roe FJ. “Review of risk factors for osteoporosis with particular reference to a possible aetiological role of dietary salt.” Food Chem Toxicol. 2000 Feb-Mar;38(2-3):237-53.
Commission E. “Implementation of the EU Salt Reduction Framework.” 2012.
D’Elia L, et al. “Habitual salt intake and risk of gastric cancer: a meta-analysis of prospective studies.” Clin Nutr. 2012 Aug;31(4):489-98.
Dudley R, et al. “Lust for salt in the Western Amazon.” Biotropica. 2012;44(1):6–9.
Gaddy JA, et a. “High dietary salt intake exacerbates Helicobacter pylori-induced gastric carcinogenesis.” Infect Immun. 2013 Jun;81(6):2258-67.
Gancz H, et al. “Sodium chloride affects Helicobacter pylori growth and gene expression.” J Bacteriol. 2008 Jun;190(11):4100-5.
“Get the Facts: Sources of Sodium in Your Diet.” Centers for Disease Control and Prevention. June 2012.
Golledge J, et al. “Reported Amount of Salt Added to Food Is Associated with Increased All-Cause and Cancer-Related Mortality in Older Men in a Prospective Cohort Study.” J Nutr Health Aging. 2015;19(8):805-11.
Graudal N, et al. “Compared with usual sodium intake, low- and excessive-sodium diets are associated with increased mortality: a meta-analysis.” Am J Hypertens. 2014 Sep;27(9):1129-37.
Jansson B. “Geographic cancer risk and intracellular potassium/sodium ratios.” Cancer Detection and Prevention. 1986; 9:171-94
Kleinewietfeld M, et al. “Sodium chloride drives autoimmune disease by the induction of pathogenic TH17 cells.” Nature. 2013 Apr 25;496(7446):518-22.
Krementsov DN, et al. “Exacerbation of autoimmune neuroinflammation by dietary sodium is genetically controlled and sex specific.” FASEB J. 2015 Aug;29(8):3446-57.
Kuzmin YV, et al. “Human-mammoth (Mammuthus primigenius Blumenbach) inter-relationships in the Palaeolithic of Siberia: a review of current knowledge.” Beam Interactions with Materials and Atoms. 2000;172(1-4):745-750.
Lee AH & Tannock IF. “Heterogeneity of intracellular pH and of mechanisms that regulate intracellular pH in populations of cultured cells.” Cancer Res. 1998 May 1;58(9):1901-8.
Lin J, et al. “Associations of diet with albuminuria and kidney function decline.” Clin J Am Soc Nephrol. 2010;5:836-843.
McMahon EJ, et al. “Altered dietary salt intake for people with chronic kidney disease.” Cochrane Database Syst Rev. 2015 Feb 18;2:CD010070.
Marro C, et al. “Archaeological investigations on the salt mine of Duzdagi (Nakhchivan, Azerbaijan).” TÜBA-AR. 2010;13.
Mente A. “Association of Urinary Sodium and Potassium Excretion with Blood Pressure.” N Engl J Med. 2014;371:601-611.
Mickleborough TD & Gotshall RW. “Dietary salt intake as a potential modifier of airway responsiveness in bronchial asthma.” J Altern Complement Med. 2004 Aug;10(4):633-42.
Mijatovic T, et al. “Cardiotonic steroids on the road to anti-cancer therapy.” Biochim Biophys Acta. 2007 Sep;1776(1):32-57.
Moe SR. “Mineral content and wildlife use of soil licks in southwestern Nepal.” Canadian Journal of Zoology. 1993;71(5): 933-936.
Mozaffarian D, et al. “Global Sodium Consumption and Death from Cardiovascular Causes.” N Engl J Med. 2014;371:624-634.
Nakajima K, et al. “The association of serum sodium and chloride levels with blood pressure and estimated glomerular filtration rate.” Blood Press. 2015 Oct 5:1-7.
O’Donnell M, et al. “Urinary sodium and potassium excretion and risk of cardiovascular events.” JAMA. 2011 Nov 23;306(20):2229-38.
O’Donnell M, et al. “Urinary Sodium and Potassium Excretion, Mortality, and Cardiovascular Events.” N Engl J Med. 2014;371:612-623.
Oparil S. “Low sodium intake–cardiovascular health benefit or risk?” N Engl J Med. 2014 Aug 14;371(7):677-9.
Rajagopal M & Wallace DP. “Chloride secretion by renal collecting ducts.” Curr Opin Nephrol Hypertens. 2015 Sep;24(5):444-9.
Resnick, et al. “Intracellular ionic consequences of dietary salt loading in essential hypertension.” J Clin Invest. 1994;94:1269-76
Rice CG. “Mineral lick visitation by Mountain Goats, Oreamnos americanus.” Canadian Field-Naturalist. 2010;124(3): 225–237.
Sandle G & Butterfield I. “Potassium secretion in rat distal colon during dietary potassium loading: role of pH regulated apical potassium channels.” Gut. 1999 Jan; 44(1): 40–46.
Sundstrom B, et al. “Interaction between dietary sodium and smoking increases the risk for rheumatoid arthritis: results from a nested case-control study.” Rheumatology (Oxford). 2015 Mar;54(3):487-93.
Tatematsu M, et al. “Effects in rats of sodium chloride on experimental gastric cancers induced by N-methyl-N-nitro-N-nitrosoguanidine or 4-nitroquinoline-1-oxide.” J Natl Cancer Inst. 1975; 55: 101–6.
Taylor RS, et al. “Reduced dietary salt for the prevention of cardiovascular disease: a meta-analysis of randomized controlled trials (Cochrane review).” Am J Hypertens. 2011 Aug;24(8):843-53.
Tsugane S. “Salt, salted food intake, and risk of gastric cancer: epidemiologic evidence.” Cancer Sci. 2005 Jan;96(1):1-6.
Weir MR & Fink JC. “Salt intake and progression of chronic kidney disease: an overlooked modifiable exposure? A commentary.” Am J Kidney Dis. 2005 Jan;45(1):176-88.
Wu C, et al. “Induction of pathogenic TH17 cells by inducible salt-sensing kinase SGK1.” Nature. 2013 Apr 25;496(7446):513-7.
Yosef N, et al. “Dynamic regulatory network controlling TH17 cell differentiation.” Nature. 2013 Apr 25;496(7446):461-8.
Zhang WC, et al. “High salt primes a specific activation state of macrophages, M(Na).” Cell Res. 2015 Aug; 25(8): 893–910.
Zimmermann MB & Galetti V. “Iodine intake as a risk factor for thyroid cancer: a comprehensive review of animal and human studies.” Thyroid Res. 2015 Jun 18;8:8.