NOTE: This is no longer the most up-to-date version of the autoimmune protocol. You can see the most current version here.
Autoimmune conditions and a leaky gut go hand in hand. In fact, in every autoimmune condition that has been tested, a leaky gut is present and is a contributing factor to the illness (not all autoimmune conditions have been tested, but many in the Paleo community assume that leaky gut is a factor in all autoimmune conditions). For individuals with suspected or diagnosed autoimmune disease, additional dietary guidelines exist to help address the disease. In many cases, autoimmune conditions can be put into full remission by following these guidelines. There is some variability to these guidelines depending on who you ask, so I have reviewed them and compiled a comprehensive list of not only dietary restrictions but also food recommendations using information from The Paleo Solution, The Paleo Answer
, and various podcast and YouTube interviews with Robb Wolf, Prof. Mat Lalonde and Dr. Terry Wahls (author of Food As Medicine
and Minding My Mitochondria
). These are all great sources for more information.
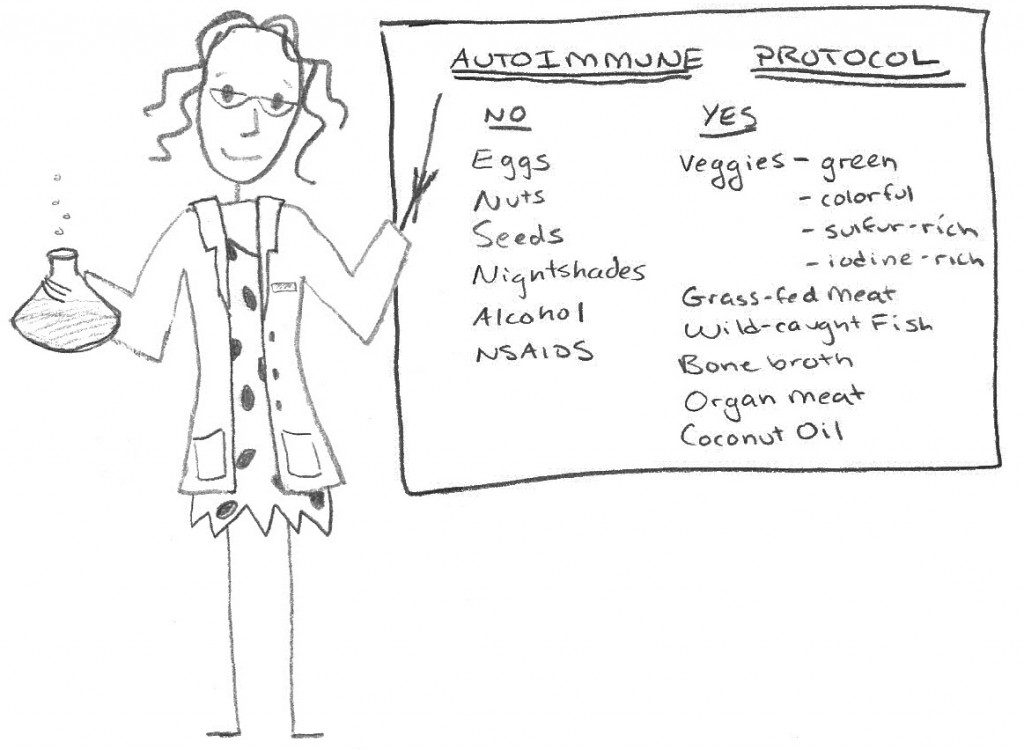
It is vitally important to adhere to a strict Paleo diet with no cheating. While other people may be able to enjoy the occasional bowl of rice, if you suffer from an autoimmune condition you are not one of these people. Grains and legumes should never be consumed. Dairy of any kind (even grass-fed ghee which can still have trace lactose and dairy proteins!) should be avoided initially (most people will not be able to successfully reintroduce dairy, although some will be okay with grass-fed butter and ghee). This may be true for the rest of your life. In addition, if you have an autoimmune condition, you should completely avoid:
- Eggs
- Nuts
- Seeds (including cocoa, coffee and seed-based spices)
- Nightshades (potatoes, tomatoes, eggplants, sweet and hot peppers and spices derived from peppers)
- Potential Gluten Cross-Reactive Foods
- Alcohol
- NSAIDS (like aspirin or ibuprofen)
The reason is that each of these causes gut irritation and/or increased gut permeability (and in the super sensitive gut of those with autoimmune conditions, they just aren’t tolerated). There is also some evidence that hormonal birth control can contribute to hunger and digestive hormone disregulation, leading to inflammation. However, you may wish to address the other elements in this post before going off birth control, depending on your personal circumstances.
Dr. Terry Wahls lays out a very convincing argument for increased vegetable intake. Her focus is on eating vegetables from four main groups: green veggies (for the vitamin B, A, C and K content and the mineral content), colorful veggies (for the flavonoids and polyphenols; at least 3 colors per day but this includes brightly colored fruit like berries), sulfur-rich veggies (cruciferous veggies, veggies from the onion family, mushrooms and asparagus), and iodine-rich foods (seaweed). Dr. Wahls recommends eating 3 cups per day of each of green veggies, colorful veggies and sulfur-rich veggies as well as at least once serving per week of seaweed. Note: If you have Grave’s Disease or Hashimotos Thyroiditis, you must also avoid goitrogenic foods, which include raw cruciferous veggies, radishes, spinach, peaches, and strawberries (cooking reduces the goitrogens; fermentation increases them). I also recommend an extra serving of seaweed each week as well as at least three servings per week of oily cold-water fish to support thyroid function (except in the case of Hashimotos Thyroiditis as there are mixed reports of iodine taken either as a supplement or in iodine-rich foods actually worsening the disease).
Meat quality is very important as this profoundly impacts the types of fat that you consume. It is extremely important to be mindful of your omega-3 to omega-6 fatty acid intake ratio, aiming for between 1:1 and 1:3, as this is essential for regulating inflammation in your body. The best way to do this is to ensure that all of your meat, poultry and fish comes from grass-fed, pastured or wild sources. Oily cold-water fish (like salmon, mackerel, sardines, herring, kipper, anchovies, trout, fresh tuna, and carp) should be consumed at least three times per week for their high omega-3 content, easily absorbed protein, vitamin D and selenium content. Grass-fed meat also contains Conjugated Linoleic Acid (CLA), known to reduce inflammation, promote healing and even fight cancer. The nutrient profile of pastured/wild meat and fish is superior as well. My post on the importance of grass-fed meat contains some suggestions for incorporating it into your diet in a budget-conscious way. It is also extremely helpful to incorporate organ meat into your diet at least twice per week due to its high nutrition density (including some amino acids, vitamins and minerals that are not as concentrated in muscle meats). Note that the high vitamin A content of liver may be contraindicated in anyone consuming foods that they are allergic or sensitive/intolerant to as it has potential adjuvant activity (it may be better to add liver into the diet after 3-4 weeks of following this protocol). It is also more important to eat organic produce as much as possible. Whole9Life has a wonderful chart on when fruits and vegetables are in season including which fruits and vegetables are important to buy organic and which aren’t, if budget is an important concern.
Autoimmune conditions are also typically associated with disruption of normal gut microflora, often including Small Intestinal Bacterial Overgrowth (SIBO). For individuals with suspected or confirmed SIBO, avoidance of starches and sugars other than monosaccharides (like glucose and fructose) is very important (read my post Fruits and Starchy Vegetables with Small Intestinal Bacterial Overgrowth for a list of which starchy vegetables are okay and which to avoid), although this is one aspect of the autoimmune protocol which is highly individual. Some people do extremely well with the inclusion of starchy vegetables in their diet. For those with gut dysbiosis (any condition in which the type, amount or location gut bacteria are not normal), it is also important to help repopulate the gut microflora by eating raw fermented foods (like sauerkraut, coconut milk kefir, or kombucha) or taking a dairy-free probiotic supplement. Some people may need to avoid high FODMAP fruits and vegetables (which I discuss in this post) as FODMAP sensitivities are common in those with leaky guts and/or gut dysbiosis (when the lining of the gut is damaged, there tends to be fewer fructose transporters so any sugar or starch containing alot of fructose is harder to digest). Others will need to limit themselves to cooked vegetables, which are typically easier to digest.
Healing the gut becomes very important. I highly recommend consuming bone broth, organ meat (note the caution against consuming liver initially described above), oily fish, and coconut oil on a fairly routine basis as well as making sure that you are getting adequate vitamin D, whether you are taking a supplement, food sources like liver and fish, or spending lots of time outside. Note that coconut oil does not contain the phytic acid or inulin fiber (both gut irritants) that other coconut products contains (a little coconut is typically tolerated, but I urge caution). Stress management is very important and I highly recommend doing at least one of the following: go for daily walks, take up yoga or tai chi, take a class on meditation, or make time for an activity/hobby that you absolutely love. And I cannot emphasize enough the importance of getting lots of good quality sleep. Aim for 8-10 hours of sleep in a cool, pitch-black room, preferably waking up without the use of an alarm. It may help both stress hormone regulation and improve sleep quality to drastically reduce your caffeine intake. Aim for no caffeine if you can. It is also very helpful to drink plenty of water and to make sure you are consuming enough food. The body is not very efficient at healing itself when you are running a caloric deficit (you shouldn’t have to gain weight to heal, but losing weight may be a competing goal for now).
I know from experience that this is a very challenging task. I also know from experience that 90% is not good enough (and the more serious your condition, the more important compliance is). I know from experience that this increases your food budget (although perhaps this can be negated by decreasing your medical expenses). I try and focus on the delicious foods that I do get to eat. I try and focus on the fact that I have a strategy for improving my health that is far more powerful than any prescription medication (Note that in many cases you will still need to be on prescription medications although you may be able to reduce your dose. Please work with your doctor on this one!). And, compliance gets easier once you start to see improvement. Are these restrictions for ever? Some may be and others might be successfully reintroduced after you see improvement in your symptoms. What foods you can reintroduce when if highly individual and will be the topic of a future post.