Hey there! My name is Alissa and I am a blogger and owner of LissMS. I am a Nutritional Therapy Consultant, AIP Certified Coach, Certified Personal Trainer and Licensed Mental Health Counselor. I utilize a holistic approach in my work and give people the tools to get exactly what they want out of life; to feel their best and thrive. I am based near Boston, MA and live with my husband and three cats. I love being outdoors and can usually be found at the beach, at least when it’s warm out. Connect with me on Instagram and Facebook, or you can check out my website too.
Hey there! My name is Alissa and I am a blogger and owner of LissMS. I am a Nutritional Therapy Consultant, AIP Certified Coach, Certified Personal Trainer and Licensed Mental Health Counselor. I utilize a holistic approach in my work and give people the tools to get exactly what they want out of life; to feel their best and thrive. I am based near Boston, MA and live with my husband and three cats. I love being outdoors and can usually be found at the beach, at least when it’s warm out. Connect with me on Instagram and Facebook, or you can check out my website too.
I am a woman, a daughter, a sister, a wife, a business owner, a helper, a healer, a friend. A woman who is powerful, strong, determined and beautiful. And a woman who just so happens to have Multiple Sclerosis.
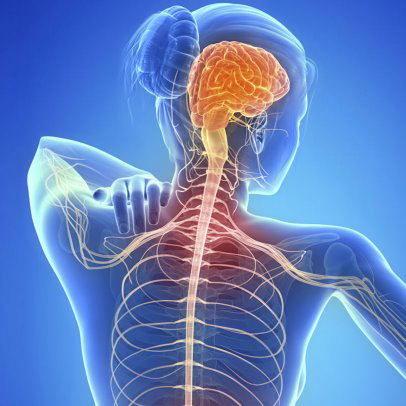
Multiple Sclerosis (MS) is an autoimmune disease that attacks the Central Nervous System (CNS). The Central Nervous System is comprised of the brain, spinal cord and optical nerves. The immune system causes inflammation that will damage the myelin- which is the outer coating that protects nerve fibers, the inflammation can also damage the nerves and the cells that make myelin as well. When this damage occurs, the signals that are sent along the nerves are interrupted or stopped completely. Due to this damage occurring in any area of the CNS, there is possibility for a wide variety and severity of symptoms to occur in MS patients.
Potential Causes
 Anyone can get MS, but there are several things that seem to contribute to an individual’s risk of getting MS more than others. These things are sex, genetics, geographic location and previous infections. There are several other things that have been thought to go into an individual’s risk factor including age and ethnicity.
Anyone can get MS, but there are several things that seem to contribute to an individual’s risk of getting MS more than others. These things are sex, genetics, geographic location and previous infections. There are several other things that have been thought to go into an individual’s risk factor including age and ethnicity.
Women get MS almost four times more than men. To me, that’s a staggering number. Up until just recently, it was not clear as to why. But there have been a few recent studies pointing out the differences in brains between women and men with MS. It seems that women have a higher incidence of a blood vessel receptor protein that allows immune cells to cross the blood brain barrier.
Multiple sclerosis is not a 100% genetically inherited disease, but there is evidence that genes do play a role. When scientists and researchers have looked at patterns within families, they find that an individual that has a first, second or third degree relative who also has MS, they have an increased risk of developing the disease also. It’s also noted that if a sibling has MS, the individual has about a 5% higher risk of developing it as well (compared to .1%). There are several genes that are believed to predispose someone to having MS and when an individual has these genes, the first piece of the MS puzzle is put into place. This is an interesting piece of the puzzle for me. I’m adopted. I don’t know ANY history or information since it was a closed adoption. I’ve tried to get my medical records, but it is an uphill battle.
With the genetic predisposition present, certain environmental triggers can make our bodies express those genes in certain ways. One of these environmental triggers is geographic location. MS is more prevalent in areas that are farther away from the equator. One possible reason for this is individuals who live further from the equator are exposed to less Vitamin D than individuals who are living near the equator. High vitamin D status is thought to be a protective factor for MS. I definitely agree with this! I lived in Ohio until I was 12, then moved to Massachusetts and have lived here since. In both locations, the few months of summer were the only times it was pleasant enough to be outdoors. I never had an affinity for winter sports, so I was indoors for much of the winter.
There are numerous infections, viruses and bacteria that have been investigated as a possible trigger to MS. Obviously viruses and bacteria cause inflammation and potentially the breakdown of myelin as well. Therefore, it makes sense that a virus, bacteria, infection could all be involved in the cause of MS. The infections that are being investigated for their link to MS are Herpes Virus, Epstein-Barr, Measles, Mumps and Rubella. This was aligned with my history as well. As a child, I had routine ear infections, which meant routine antibiotics as well. Unfortunately, antibiotics will wipe out gut bacteria and it can take months to recover from just one course of antibiotics. How was I recovering? With chicken nuggets and cottage cheese! Not the most nutrient dense things to be repopulating my gut bacteria.
Eventually in high school, things caught up to me again. I caught mononucleosis in 9th grade, which kicked off a slew of “viruses” that no one ever really figured out. I was sick all the time, my hair was falling out and in horrible shape and I could barely make it to school. During this time my mood changed as well. I had already had mood instability and depression, but this is when my depression became severe. I never connected it to what was going on with my immune system, but knowing what I know now, I’m sure it was all related.
Save 70% Off the AIP Lecture Series!
Learn everything you need to know about the Autoimmune Protocol to regain your health!
I am loving this AIP course and all the information I am receiving. The amount of work you have put into this is amazing and greatly, GREATLY, appreciated. Thank you so much. Taking this course gives me the knowledge I need to understand why my body is doing what it is doing and reinforces my determination to continue along this dietary path to heal it. Invaluable!
Carmen Maier
 Types of Multiple Sclerosis
Types of Multiple Sclerosis
There are four main types of Multiple Sclerosis. Clinically isolated syndrome (CIS), Relapsing Remitting MS (RRMS), Primary Progressive MS (PPMS) and Secondary Progressive MS (SPMS).
Clinically Isolated Syndrome
Clinically isolated syndrome or CIS is diagnosed when someone experiences the first episode of symptoms caused by inflammation and demyelination of either the brain or spinal cord but are missing all the criteria for a full MS diagnosis. It’s MS no man’s land if you will. Individuals who are diagnosed with CIS, have a higher chance of being diagnosed with MS later in life but it’s not always the case that they will be. I was “technically” given a diagnosis of CIS at my first appointment with my neurologist. I remember reading the MRI report and having it say, “probable demyelinating disease”. I knew what that meant.
Relapsing Remitting MS
Relapsing remitting MS type is the most common form of MS. This is when an individual has two distinct periods of their disease, disease progression and disease remission. During disease progression, an individual will have a relapse and subsequent symptoms, then the symptoms will eventually fade, and they will return to their baseline state. The two periods are very clearly defined and switch back-and-forth as the years go on. During the remission phase, all symptoms may disappear completely, or some may linger and become permanent as more relapses occur and more damage is accumulated. About 85% of people are initially diagnosed with RRMS. I don’t think there was a singular moment where I got diagnosed with MS. At least not in some grand fashion that I remember. I had many, frequent follow ups with my neurologist in that year after my symptoms started. Then a year later I had my repeat MRI. I remember the conversation changing, from “what if’s” to “when”. It wasn’t a question anymore of if I had it, I did. I knew it, even before I got through with the testing. Everything added up and the dots connected. Now it was more about moving forward and staying functional.
I fit the picture of a “relapsing remitting” MSer. Over the past 9 years, I’ve had a total of 3 relapses, all within a year and a half. Which is fairly quick as far as relapses go. I was “fine” and “stable” for the first few years of my diagnosis. I had chosen the med Copaxone, which had a pretty good track record, and few side effects. I was doing well, until I wasn’t. Those three relapses sent me into a tail spin. My stability was pulled out from under me and I could no longer find my center. I was still in the dark about AIP and paleo during this time, so off to the hospital I went, and high doses of steroids were my mainline of defense. They helped, sort of. I didn’t get the high energy, voracious appetite and insomnia that so many others get with steroids. They wiped me out. I couldn’t stay awake, I couldn’t work, living was hard. Eventually the symptoms faded, and life returned to normal. But each relapse there was a little bit left over. A few nagging symptoms that will present themselves when I’m stressed, hot or anytime they damn well please.
Primary Progressive MS
Primary progressive MS type is defined by the persistent worsening of function without experiencing the relapses or remissions. This form will progress steadily from the time of onset. Individuals will experience worsening of their symptoms at varying rates, but the progression will be constant. At times the progression my reach a plateau as well, then will pick up again. About 15% of people are diagnosed with PPMS.
Secondary Progressive MS
Secondary progressive MS type initially starts out as relapsing remitting then will begin to follow a progressive course. Many people who start out with relapsing remitting will eventually transition to secondary progressive. At one point in time it was thought that after about 10 years of having relapsing remitting you would progress into secondary progressive. However, this data was taken before the widespread use of medications. I just recently asked my own neurologist about this statistic, as I just reached my nine-year anniversary. He was very adamant that this was not the case anymore due to having such a wide array of medications and treatments available for so many people. This was very encouraging to me! He also stated that due to my lifestyle factors, diet and exercise, I’m also doing myself a world of good at preventing any further progression. Go AIP!
Diagnosis
 Getting diagnosed with Multiple Sclerosis can be a confusing and complicated process. There are multiple tests involved and the fact that each person has different symptoms, makes the process that much harder. However, there are a few symptoms that tend to show themselves first before others. Vision issues, including optic neuritis (inflammation of the optic nerve), muscle issues and fatigue. The first symptom that led me to the doctor was optic neuritis. When I went to the eye doctor for my odd blurry vision issue, he checked out my vision and said I was “fine” and had 20-20 vision. But the way I was describing my symptoms, he wanted me to get an MRI. Odd next step I thought. A few days later he called with the MRI results.
Getting diagnosed with Multiple Sclerosis can be a confusing and complicated process. There are multiple tests involved and the fact that each person has different symptoms, makes the process that much harder. However, there are a few symptoms that tend to show themselves first before others. Vision issues, including optic neuritis (inflammation of the optic nerve), muscle issues and fatigue. The first symptom that led me to the doctor was optic neuritis. When I went to the eye doctor for my odd blurry vision issue, he checked out my vision and said I was “fine” and had 20-20 vision. But the way I was describing my symptoms, he wanted me to get an MRI. Odd next step I thought. A few days later he called with the MRI results.
“You don’t have a brain tumor, but you need to see a neurologist, today”
Alright then. Not quite the news you expect to be hearing when you’re 24, and at work! None the less, I made an appointment, and started down the diagnostic journey.
There is no one test that will tell you that you have MS. Instead, there is a variety of tests that will point you and your doctor in a direction, then inferences can be made from there. The criteria for an MS diagnosis are involved as well. An individual needs to have damage in at least two different areas of their CNS, that damage had to happen at different points in time, and you have to rule out all other possible diagnoses (!). That last part is a tall order. In 2017 the criteria were revised to make the diagnosis processed quicker. I’m glad they did, being in the no man’s land of a CIS diagnosis is an uncomfortable place.
The tests needed for diagnosis are complex and time intensive too; blood tests to look at inflammation status and levels of red and white blood cells, a lumbar puncture to look at the cerebral spinal fluid, an evoked potentials test to measure the brains response time and obviously, MRIs.
After I met with the neurologist to go over my initial MRI, he set me up with the rest of the tests. I had my initial blood tests, then a few more MRIs to look at my spinal cord too, since my original MRI only looked at my optic nerves and brain. I never did the evoked potentials test, but in this test, the brains response to certain stimuli (light, touch and sound) is tested and recorded. Since damage can occur in the brain that would affect how quickly and effectively this information is processed by the brain, this test can be very helpful. Within this test, there are three different types, a visual, brainstem auditory and sensory evoked potentials. When these tests are run, wires are placed on the scalp to measure brain activity and it takes a few hours to complete all three tests.
The lumbar puncture, otherwise known as a spinal tap, was the worst part of the diagnosis process for me. Cerebrospinal fluid (CSF) is a clear liquid that surrounds the brain and spinal cord. It serves as a shock absorber for the CNS, circulates nutrients and helps to remove waste products from the brain. It helps to diagnose many other diseases of the nervous system-not only MS. Getting CFS is a bit tricky though, it’s obtained through a procedure called a lumbar puncture. Where the patient lays on their side, usually with their feet up, (think fetal position) and a long needle is inserted between two vertebrae where the CFS moves up and down the spinal cord. A few tablespoons are removed and voila! All set. In a routine situation, this procedure should only take about 10 minutes from start to finish, and enough numbing agent should be used where the patient remains comfortable.
When I had my procedure done, we ran into issues. About a year before this diagnostic journey, I had lower back surgery, which left me with a lot of scar tissue on and near my spinal cord. This scar tissue prevented the needle from being inserted cleanly and would re-direct the needle when it was halfway to Its destination. What should have taken 10 minutes, took 45 minutes. What should have been a relatively pain free experience, was excruciating. Lidocaine only lasts for so long.
Afterwards, you are encouraged to rest and lay down for the rest of the day and a few days after, or your body might not heal and seal the wound properly and you could end up leaking CFS fluid. This results in a horrendous headache and having to go back into the hospital for a blood patch. I was lucky enough to experience this as well. I remember my father driving me back to the hospital, getting to the hospital, immediately laying on the floor because standing would result in getting sick within 30 seconds. To say it was a traumatic experience would be an understatement. Right after I got admitted, the doctor took a ridiculous amount of blood and inserted it into my back. I felt almost an instantaneous relief from my headache. I’m not sure if it was a placebo effect, or actual healing, but I didn’t care. It was the worst headache of my life and it was going away.
After that, I didn’t know what else I could take. I didn’t know what else I wanted to take! I don’t remember the exact order of all the tests, but eventually they were all completed, around the middle of August. I had started the journey the beginning of June. Some people get diagnosed with MS in a day, some don’t get diagnosed for 10 or 20 years, or even more. However, with medical and testing advancements over the last 5-10 years, those long waiting times are fewer and far between now. When I met with my neurologist to talk about the findings, he said what I knew was coming, MS. MS had been one of the few possibilities on the table from the beginning. So, it wasn’t a total shock to me. I had been doing my research throughout the past few months and connecting the dots, it did seem to make sense with my history.
I left that appointment with a stack of potential medication binders up to my eyes. He wanted me to start treatment right away. I had to look over the options in my arms and let him know in a few weeks. Off I went into the world of chronic illness and autoimmunity. Equipped with drug company binders as my armor. I don’t think I quite grasped the gravity of the situation at that time. But how could I have really? I was 24, a year away from finishing graduate school, and in “the best years of my life”. I didn’t know what the next few years would bring. I just wanted my next research paper done and over with!
My Journey to AIP
Eventually, many years down the road, I found a way of healing that would transform everything I understood about medicine up until that point. I knew I was being called for a higher purpose. I knew I was given MS for a reason. I started another journey, an educational journey. I wanted to help others that were in the same place that I was years ago. That’s why I became a Nutritional Therapy Consultant and AIP Certified Coach. I wanted to be able to help others along in their healing journey, be a sense of support, because that’s what 24-year-old me needed as well, support and guidance from someone who had been there. You know that saying, be who you needed when you were younger? I changed it a little, be who you needed when you were healing.
I invite you to come on that journey with me! Head on over to my blog at www.liss-ms.com or find me on Instagram @Liss.MS and send me a message! I love to connect with others who have MS and chronic illnesses. While you’re there, you’ll find a free download I created called The 5 Best Foods to Eat if You Have Multiple Sclerosis. I think you’ll like it!
There are many factors that contributed to my MS diagnosis, so there is no blame to be put anywhere or on anyone. The only thing that truly matters is how I move forward with the knowledge I have now. My passion is spreading my knowledge to others like you and help you as I have been helped as well.