Table of Contents[Hide][Show]
Nutrient Deficiencies Associated with Autoimmune Disease+−
- Vitamin A – 56% of Americans rarely meet the RDA
- Vitamin B6 – 54% of Americans rarely meet the RDA
- Vitamin B9 – 75% of Americans rarely meet the RDA
- Vitamin B12 – 30% of Americans rarely meet the RDA
- Vitamin C – 38% of Americans rarely meet the RDA
- Vitamin D – An estimated 75% of Americans are deficient
- Vitamin E – 60% of Americans rarely meet the RDA
- Copper – 31% of Americans rarely meet the RDA
- Iodine – 74% of Americans rarely meet the RDA
- Iron – 39% of Americans rarely meet the RDA
- Magnesium – 68% of Americans rarely meet the RDA
- Selenium – 15% of Americans rarely meet the RDA
- Zinc – 73% of Americans rarely meet the RDA
- DHA & EPA – 70% of Americans rarely meet the RDA
- Phytochemicals – No RDA established
- The Common Denominator
Many micronutrients are immune modulators, meaning that sufficient amounts of these substances are required to regulate the immune system. Although epidemiological studies reveal a correlation between dietary intake of specific nutrients and increased risk of autoimmune disease, these studies are mostly designed to direct future research rather than to insinuate causality. In truth, in most cases, we don’t know if nutrient deficiency is a precursor to autoimmune disease or if nutritional deficiency is a result of autoimmune disease. Dietary insufficiency or malabsorption issues contribute to the immune system’s becoming overstimulated in autoimmune disease. However, the need for many micronutrients also increases when there is inflammation. It could be that those with autoimmune disease become deficient because their bodies need more of these vitamins, minerals, and antioxidants to help control inflammation when their immune systems go into overdrive. Either way, there is a need for increased intake of these important nutrients to help control inflammation, regulate the immune system, and heal the body.
Unfortunately, getting all of our required nutrients from food is easier said than done. Many of the staple foods of the typical American diet have very little nutritional value. Even worse, the more a food is refined and processed and manufactured, the more the nutrients inherent to the raw ingredients are leached out, removed, or degraded. Processed foods, refined foods, fast food, and junk food all contribute next to nutrient deficiency (plus, they’re often problematic for our health in other ways). But even foods that many people think are healthy, like whole grains and low-fat dairy, are pretty weak when it comes to essential nutrients. And every time a nutritionally weak food displaces a nutritional powerhouse, the overall nutritional value of the diet suffers.
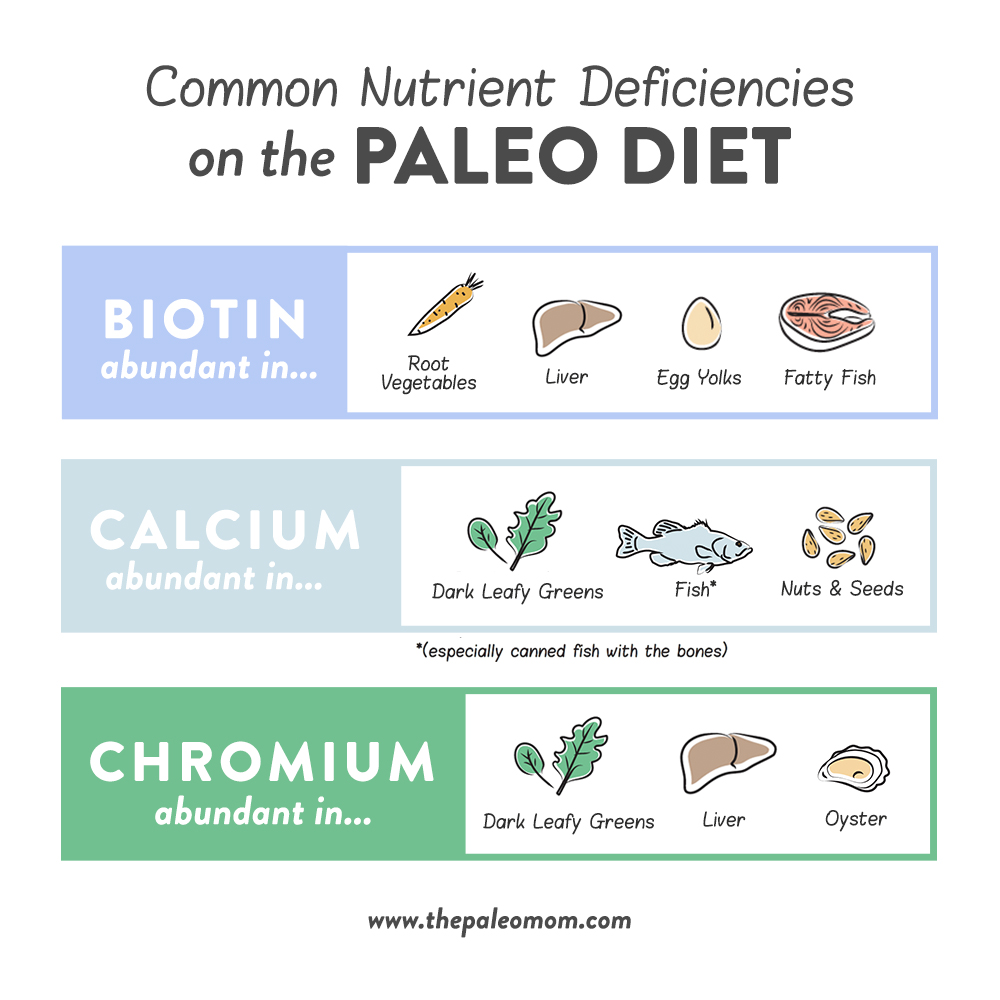
Even following a healthy dietary template, such as the standard Paleo diet, as defined in the last decade of books and websites, is not a guarantee that you’re getting all the micronutrients you need to be healthy. And while the foods endorsed by the Paleo diet represent the most nutrient-dense foods in our food supply, reaching micronutrient sufficiency still requires commitment. In fact, analyses of typical Paleo food choices reveal that biotin (abundant in liver and root vegetables), calcium (abundant in its most bioavailable form [meaning that our bodies can easily digest and use it] in dark leafy greens like kale, as well as in whole fish like sardines), and chromium (abundant in dark leafy greens, oysters, and liver) are commonly deficient on the Paleo diet. While the Paleo diet far outstrips other approaches in terms of micronutrient sufficiency, if you just stick to the stereotypical meat, veggies, and coconut oil, you may miss out on important nutrients for optimal health.
That’s why the Autoimmune Protocol is a nutrients-first approach, also called nutrivore, with the goal of choosing the most nutrient-dense foods available in order to reach dietary nutrient sufficiency, meaning that we are consuming adequate amounts of all of the essential and non-essential nutrients required for human health.
To further emphasize why nutrient sufficiency is such an important tenet of the AIP, let’s examine the link between nutritional insufficiency and autoimmune disease incidence.
Nutrient Deficiencies Associated with Autoimmune Disease
Dietary insufficiency of the following essential vitamins and minerals is shockingly common. Each of these nutrients is important for normal immune system function, which is why insufficiency is strongly linked to autoimmune disease. Additional associations are likely as this is an emerging field of scientific research.
 Vitamin A – 56% of Americans rarely meet the RDA
Vitamin A – 56% of Americans rarely meet the RDA
Vitamin A is essential for maintenance and normal regeneration of mucosal barriers, such as the gut epithelium. It is also critical for normal function of inflammatory cells, such as neutrophils, macrophages, and natural killer cells. Vitamin A levels have a profound effect on different T cell subpopulations, cytokines (chemical mediators of inflammation), and production of various antibody subclasses. In particular, vitamin A supports regulatory T cell formation, which may be the key to the benefits observed in vitamin A supplementation studies. See also Genes to Know About: Vitamin A Conversion Genes
Vitamin A deficiency is strongly associated with impaired immunity and susceptibility to infectious disease and has been associated with several autoimmune diseases, including alopecia areata, multiple sclerosis, and autoimmune hepatitis.
 Vitamin B6 – 54% of Americans rarely meet the RDA
Vitamin B6 – 54% of Americans rarely meet the RDA
Vitamins B6, B9, and B12 are also critical for supporting the methylation cycle (see Genes to Know About: MTHFR). Importantly, changes in DNA methylation (both too much and too little) have been implicated in autoimmune diseases, such as systemic lupus erythematosus, so it is not surprising that these three B vitamins in particular are the ones that have been linked to autoimmune disease.
Vitamin B6 is converted into the coenzyme form pyridoxal 5 ‘-phosphate (PLP), which is used in the metabolism of amino acids and lipids and is required for gluconeogenesis (the creation of glucose from amino acids or fatty acids). PLP is also involved in the synthesis of neurotransmitters and hemoglobin. PLP deficiency has been linked to type 1 diabetes.
Save 70% Off the AIP Lecture Series!
Learn everything you need to know about the Autoimmune Protocol to regain your health!
I am loving this AIP course and all the information I am receiving. The amount of work you have put into this is amazing and greatly, GREATLY, appreciated. Thank you so much. Taking this course gives me the knowledge I need to understand why my body is doing what it is doing and reinforces my determination to continue along this dietary path to heal it. Invaluable!
Carmen Maier
 Vitamin B9 – 75% of Americans rarely meet the RDA
Vitamin B9 – 75% of Americans rarely meet the RDA
Vitamin B9 (folate) is is converted into the coenzyme tetrahydrofolate (THF), which is involved in the metabolism of nucleic acids and amino acids. THF is also necessary for normal cell division and for the production of red blood cells. Activated macrophages and some T cells involved in some autoimmune diseases do have folate receptors in their cell membranes, which is why the folate agonist methotrexate has been used to treat rheumatoid arthritis.
Vitamin B9 deficiency has been associated with cerebral folate deficiency syndrome, rheumatoid arthritis, Sjogren’s syndrome, celiac disease, Crohn’s disease and ulcerative colitis.
 Vitamin B12 – 30% of Americans rarely meet the RDA
Vitamin B12 – 30% of Americans rarely meet the RDA
Vitamin B12 is essential for the metabolism of carbohydrates, proteins, and lipids in every cell of the body. It is particularly important for DNA synthesis and regulation, fatty acid synthesis, and energy production, and plays a key role in the production of blood cells, nerve sheaths, and proteins. Vitamin B12 is a necessary factor for two important enzymes in the methylation cycle: methylmalonyl-CoA mutase (MCM) and 5-methyltetrahydrofolate-homocysteine methyltransferase (MTR, which is also sometimes called methionine synthase).
Vitamin B12 deficiency has been associated with multiple sclerosis, celiac disease, Sjogren’s syndrome, Crohn’s disease, ulcerative colitis, autoimmune atrophic gastritis, alopecia areata and type 1 diabetes.
 Vitamin C – 38% of Americans rarely meet the RDA
Vitamin C – 38% of Americans rarely meet the RDA
Vitamin C is an extremely important antioxidant that is also a key regulator of the stress response (see TWV Podcast Episode 446: Nutrient Deficiencies Caused by Stress). Adequate levels are essential for preventing gastritis (whether the cause is autoimmune, chemical, or infectious) and are helpful in controlling persistent infections like H. pylori.
Vitamin C deficiency is associated with lichen planus and idiopathic thrombocytopenic purpura.
 Vitamin D – An estimated 75% of Americans are deficient
Vitamin D – An estimated 75% of Americans are deficient
In addition to all its other roles (see Vitamin D), vitamin D is crucial for regulating several key components of the immune system, including formation of important antioxidants and controlling subpopulations of T cells. Most important, regulatory T cell function is dependent on vitamin D (meaning that regulatory T cells can’t perform their duties without vitamin D).
Vitamin D deficiency is strongly linked to autoimmune disease and has been implicated as an environmental trigger for systemic lupus erythematosus, type 1 diabetes, autoimmune interstitial lung disease, multiple sclerosis, rheumatoid arthritis, celiac disease, psoriasis, and inflammatory bowel disease.
 Vitamin E – 60% of Americans rarely meet the RDA
Vitamin E – 60% of Americans rarely meet the RDA
Vitamin E’s main role in the immune system appears to be its antioxidant activity, but it has also been shown to promote maturation of T cells in the thymus.
Vitamin E deficiency has been implicated in psoriasis, vitiligo, alopecia areata, and rheumatoid arthritis. Vitamin E supplementation reduced inflammation in patients with rheumatoid arthritis.
 Copper – 31% of Americans rarely meet the RDA
Copper – 31% of Americans rarely meet the RDA
Copper is required by the immune system to support the production of some cytokines by T cells and regulate T cell proliferation (cell division), and dietary copper is important in resistance to infection.
Copper deficiency is associated with rheumatoid arthritis and pemphigus vulgaris.
 Iodine – 74% of Americans rarely meet the RDA
Iodine – 74% of Americans rarely meet the RDA
Iodine is important for the development and proper function of the thyroid and is an essential component of thyroid hormones. Iodine may also have a role in immune function because phagocytosing (eating of pathogens) white blood cells produce various iodoproteins (proteins containing iodine), including T4 thyroid prohormone.
Both excess and deficiency of iodine are associated with Hashimoto’s thyroiditis and Grave’s disease.
 Iron – 39% of Americans rarely meet the RDA
Iron – 39% of Americans rarely meet the RDA
Iron is a critical component of hemoglobin, the protein in red blood cells responsible for carrying oxygen from the lungs to every other cell in the body. Specifically, iron is part of a molecule called heme: four heme molecules are part of a hemoglobin protein, and it is the iron itself that binds to oxygen. Hemoglobin is not the only protein in the body that contains heme. Heme is also a critical component of a family of proteins involved in protection from oxidative damage. Iron is also needed to metabolize B vitamins, is a necessary cofactor for a variety of enzymes, and is important in protein metabolism.
Iron deficiency is a hallmark of autoimmune hemolytic anemia, autoimmune aplastic anemia, and pernicious anemia. Deficiency is also associated with rheumatoid arthritis, autoimmune gastritis, systemic lupus erythematosus, Sjogren’s syndrome and celiac disease.
 Magnesium – 68% of Americans rarely meet the RDA
Magnesium – 68% of Americans rarely meet the RDA
More than three hundred different enzymes in our cells need magnesium to work, including every enzyme that uses or synthesizes ATP and including enzymes that synthesize DNA and RNA. It is important for the metabolism of phosphorus, calcium, potassium, sodium, B-complex vitamins, and vitamins C and E. Magnesium is also a cofactor in methylation and is necessary for detoxification functions. Importantly, magnesium depletion has been shown to have a profound impact on the thymus gland, which has implications for all autoimmune diseases. See also TWV Podcast Episode 409: Let’s Talk About Magnesium
Deficiency is associated with systemic lupus erythematosus.
 Selenium – 15% of Americans rarely meet the RDA
Selenium – 15% of Americans rarely meet the RDA
Selenium is very important in several aspects of the immune system. Selenium deficiency increases risk of viral infections, it appears to be essential for T cell function (this has been best studied in the context of HIV infection) and activation of neutrophils and natural killer cells, and it protects against several inflammatory cytokines and modulates the production of several key inflammation-signaling molecules. Selenium helps protect against the toxic effects from arsenic, cadmium, and mercury. Selenium is important for absorption of vitamin E, and has been shown to prevent some forms of cancer, lower the risk of cardiovascular disease, and lower the risk of complications in critical-care units.
Deficiency is associated with Hashimoto’s thyroiditis, Grave’s disease, pemphigus vulgaris and lichen planus.
 Zinc – 73% of Americans rarely meet the RDA
Zinc – 73% of Americans rarely meet the RDA
Zinc is the second most abundant metal in the body, after iron, and is necessary for the activity of approximately three hundred different enzymes. Zinc has been shown to directly affect the immune system through control of T cell development and activation. It has also been shown to reduce cytokine production by Th1 and Th17 cells (typically overactive in autoimmune disease). And, zinc is an important regulator of intestinal permeability, see 8 Nutrients for Leaky Gut. Zinc deficiency is arguably the most common micronutrient deficiency in autoimmune disease.
Deficiency is associated with rheumatoid arthritis, multiple sclerosis, pemphigus vulgaris, Alzheimer’s disease, autoimmune hepatitis, primary biliary cirrhosis, autoimmune thyroid disease, systemic lupus erythematosus, celiac disease and type 1 diabetes.
 DHA & EPA – 70% of Americans rarely meet the RDA
DHA & EPA – 70% of Americans rarely meet the RDA
The long-chain omega-3 fatty acids, DHA and EPA, are stored in the cell membrane, including many immune cells such as monocytes, macrophages, granulocytes (like neutrophils), and lymphocytes. When needed, they can be internalized and metabolized into prostaglandins, thromboxanes, and leukotrienes, which mediate inflammation. In addition, the incorporation of DHA and EPA into the cell membrane affects cell membrane properties, such as fluidity, flexibility, and permeability, and alter the activity of enzymes that are embedded in the membrane. These effects are beneficial to the health and function of the cell. For example, having a more flexible and fluid membrane for a phagocytic cell (an “eater” cell like a macrophage, dendritic cell, or a neutrophil) means that it is efficient at doing its job of “eating up” pathogens. See also The Importance of Fish in Our Diets and TWV Podcast Episode 415: Fish oil, Healthy or not?
Supplementation of DHA and EPA has been shown to be beneficial in rheumatoid arthritis, Crohn’s disease, ulcerative colitis, psoriasis, systemic lupus erythematosus, multiple sclerosis, autoimmune-mediated glomerulonephritis.
 Phytochemicals – No RDA established
Phytochemicals – No RDA established
Phytochemicals, such as polyphenols, are important antioxidants, many with anti-inflammatory properties and known to improve the composition of the gut microbiome. See The Amazing World of Plant Phytochemicals: Why a diet rich in veggies is so important! and Polyphenols: Magic Bullet or Health Hype?
Supplementation has been shown to be beneficial in autoimmune thyroiditis, type 1 diabetes, and rheumatoid arthritis.
The Common Denominator
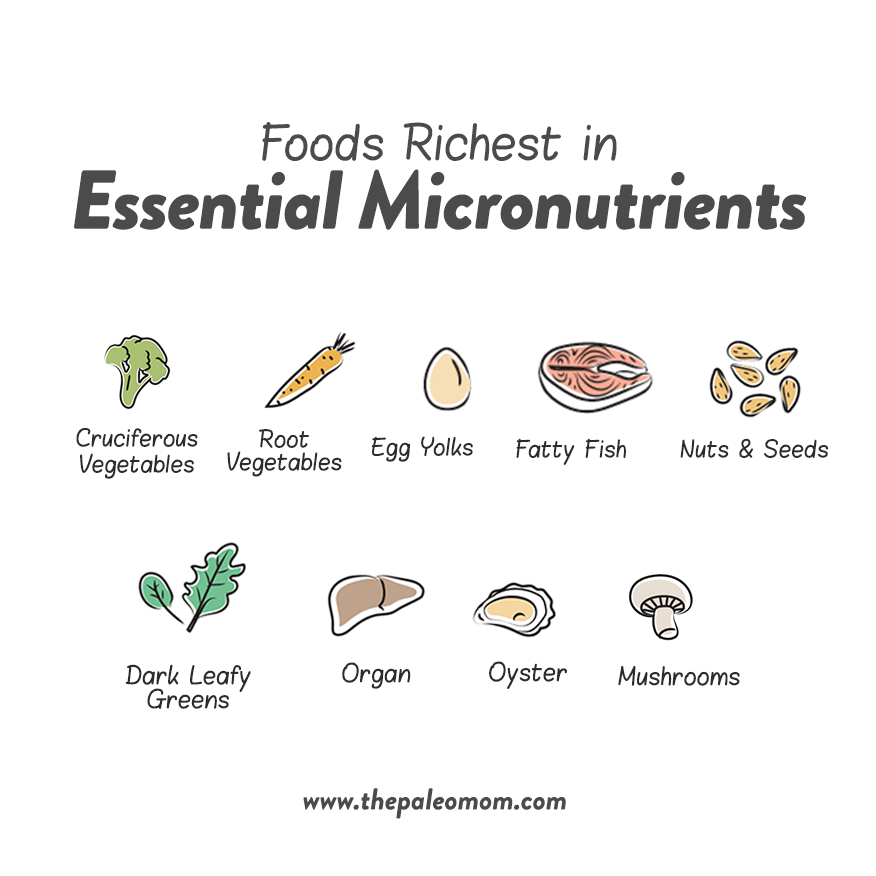
When we consider the foods richest in essential micronutrients, certain foods come up again and again as powerhouses of nutrition, especially liver and other organ meat, seafood (especially shellfish, but also fatty fish), and vegetables of all kinds, but notably leafy greens, vegetables from the cruciferous family (which includes cabbage, broccoli, and kale) and mushrooms.
Achieving nutrient-sufficiency is achieved by making these nutrient-dense powerhouse foods the basis of every meal. This means that every meal would be centered around organ meats, shellfish, brightly pigmented fruit, sea vegetables, fatty fish, cruciferous vegetables, leafy greens, mushrooms, fermented veggies, fresh herbs, and fibrous roots. Other fruit, vegetables, whitefish, grass-fed and pasture-raised meats, and healthy fats like extra virgin olive oil round out the diet. Eating 8 or more servings of vegetables per day, seafood most days, and organ meat 3 to 5 times per week is important for nutrient sufficiency. This forms the basis of the Autoimmune Protocol.
Learn More About the AIP
I firmly believe that a thorough understanding of the details is key to utilizing the AIP successfully, whether adopting a more relaxed version for general health or adapting the AIP for non-autoimmune chronic illness. Understanding nutrient deficiency are a big part of that.
Below, I’ve ordered my AIP educational resources geared at autoimmune disease sufferers and their caregivers from introductory quick-start to detailed deep-dive, as well as from independent to interactive.
Intro to AIP’ free e-mail series
I recently completely revamped my 15-part Intro to AIP e-mail series. This is a great starting point if you’re curious about the AIP but don’t feel the need to rush in (you’ll be delivered the e-mails over a month, but you’ll also get my AIP Quickstart Guide as a free download right away). You can sign up for the series here.

The Autoimmune Protocol e-book
With this all-in-one e-book, you’ll be able to hone in on the information that matters most, including 300+ pages of quick-access information on the AIP, new information on why nutrient sufficiency and gut health are a primary focus of the AIP, 4 weeks of meal plans with shopping lists, over 80 family-friendly recipes, and more! This is a great starting point if you want everything you need to jump right in all in one place, but without diving deep into the why’s. Get it here.
The Paleo Approach book
The Paleo Approach is the definitive guidebook on the Autoimmune Protocol. With over 400 pages of scientific explanations of the why’s, what’s, and how’s behind diet and lifestyle recommendations to help regulate the immune system and provide the body with the opportunity to heal. This encyclopedic resource also contains tons of practical information including tips for transitions, working with your doctor, medical test and treatments that might be helpful, troubleshooting, and when and how to reintroduce foods. This is a great starting point if you need to know the why’s to be motivated to make positive changes, or if you learn better reading an actual physical book (highlighters and postits welcome!). Get it here.

Therapeutic Paleo Approach online course
The Therapeutic Paleo Approach online course features 5 hours of video lecture that covers nutrient requirements of biological systems, prevalence and sources of nutrient deficiencies, top sources of nutrients commonly deficient, designing a nutrient-sufficient diet, sleep as a linchpin of health, impact of stress on health, activity balance and health, connection and health, links to the top mortality- and morbidity-causing chronic illnesses, and an introduction to the Autoimmune Protocol! This is a great starting point if you learn better with videos and visual guides than reading a book, and are looking for a broad overview with a positive what-to-eat focus. Get instant access here.
The AIP Lecture Series interactive online course
In this 6-week, video-based, intensive and interactive online course, I teach the scientific foundation for the diet and lifestyle tenets of the Autoimmune Protocol, plus provide tons of tips and strategies for implementation, refinement and troubleshooting! It’s also my opportunity to provide individualized guidance and support, and I connect with every single student within a private Facebook group for the course and answer every single question posed during the session.
This course is perfect if you learn better in an interactive, supportive multimedia environment, want to dive deep into the why’s, and want the most comprehensive understanding of the full AIP possible. I gear this course at all levels, from the person completely new to the AIP all the way to the seasoned pro who is looking to take their AIP to the next level.
You can learn more about the AIP Lecture Series here.