Eczema is a general term used to describe a collection of skin conditions (the most common being atopic dermatitis) in which the skin is inflamed and irritated. The inflammation in these skin conditions is in the epidermis, or outer layer of the skin, and this is the main distinction between eczema and other skin conditions. The presentation varies and can include any of the following symptoms: redness, skin edema (swelling), itching, dryness, crusting, flaking, blistering, cracking, oozing, or bleeding. It can affect any area of the body and areas can range in size from quite small to very large. Eczema affects about 10% to 20% of infants and about 3% of adults and children in the U.S.
What Causes Eczema?
It was once thought that eczema was a primary immune system disorder, where an overactive immune system, led by a type of white blood cell called T-Cells, responded to environmental factors by initiating an inflammatory response. This idea made sense because not only would inflammation produce the red, irritated skin characteristic of eczema, but this dysfunctional immune response also provided an explanation for the observed incidence of atopic dermatitis in conjunction with asthma, hay fever, and other allergies. However, the most up-to-date research does not support this explanation.
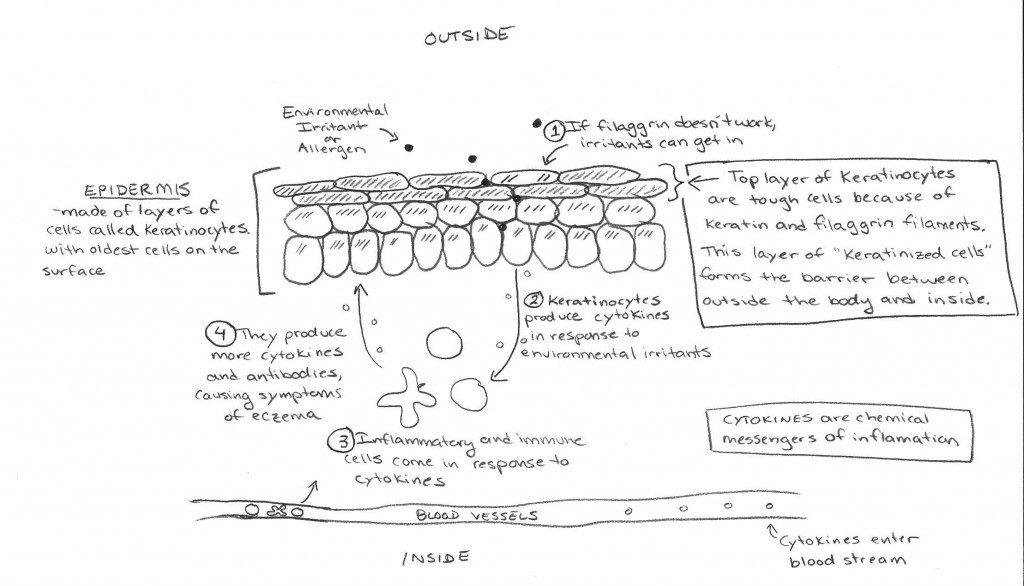
The most current research points to a different origin of eczema. It is now thought that eczema results from structural defects in the epidermis resulting in “impaired barrier function”. Essentially, abnormalities in the skin make it more permeable to toxins and antigens, which then causes an exaggerated immune response1.
Save 80% Off the Foundations of Health
Expand your health knowledge on a wide range of topics relevant to you, from how to evaluate scientific studies, to therapeutic diet and lifestyle, to leaky gut and gut microbiome health, to sustainable weight loss, and much more!!!

You could think of this as “leaky skin”, where the skin no longer is able to fulfill its primary role as the first line of defense between the body and the outside world. Once the barrier function of the skin is disrupted, various substances (like toxins, allergens, antigens; basically anything that the immune system views as a foreign invader) can “leak” in from the outside and this is what activates the immune response. This model is supported by recent isolation of specific mutations in the gene for filaggrin, a structural protein in the epithelial cells of the skin. This defective gene (and perhaps other similar gene mutations) may lead to a dysfunctional epidermal barrier and is likely the primary cause of eczema.
Conventional Approaches to Treating Eczema
What is your doctor likely to tell you about eczema? Your doctor will likely tell you that the exact cause of eczema is unknown, but it’s thought to be linked to an overactive response by the body’s immune system to an irritant. He or she may not be aware of the newest research on eczema, but that will not affect decisions on treatment. It’s fairly common and not life threatening.
Treatment of any skin condition should always start with proper care of your skin. In the case of eczema, you should avoid triggers such as heat, perspiration, and low humidity, and keep the skin well hydrated at all times. The standard pharmaceutical treatment is the application of topical corticosteroid creams, which can be purchased in your local pharmacy or prescribed in stronger strengths by your doctor. If allergies are suspected, a daily antihistamine such as loratidine (Claritin) may be suggested. In severe cases, your doctor may prescribe an oral corticosteroid, such as prednisone.
Now you may be asking “If eczema is no longer considered a primary immune disorder, why is the standard of treatment aimed at stopping inflammation and controlling the immune response?” The answer is that the symptoms of eczema are indeed caused by an immune response, but it is a response from environmental triggers entering the body through “leaky” skin as opposed to an immune system run wild and attacking itself.
What should you know that your doctor may not tell you?
As discussed above, the most current belief is that those with eczema carry a genetic predisposition to “disrupted epidermal barrier function” 1. This could be thought of as “leaky skin” and is a very analogous to a “leaky gut”. In fact, because of the similar roles of the skin and the gut to act as a barrier, it is no surprise that eczema is also associated with increased intestinal permeability 2, i.e., a leaky gut. It is still unknown whether a leaky gut contributes to the development of eczema, however.
Eczema is also often seen in conjunction with a multitude of autoimmune diseases. For example, eczema occurs about three times more frequently in celiac disease patients and about two times more frequently in relatives of celiac patients, potentially indicating a genetic link between the two conditions. For this reason, gluten sensitivity is suspected as a possible root cause for eczema, but that is still unconfirmed. Anecdotally, many people find that their eczema goes away when they adopt a gluten-free diet. Other people find elimination of additional foods, such as eggs, are required to see improvement. There also appears to be a strong link between eczema and immune hypersensitivity 3. For example, more than 50% of children with atopic dermatitis go on to develop asthma and allergies. This may be related to the association with increased intestinal permeability or may reflect an as yet unknown common causal mechanism (such as a gene mutation or environmental factors).
Although progress had been made toward understanding this complex condition and how it relates to other health issues, the cause of eczema remains unknown. We are certain the coming years will bring more information and we will try to update everyone as it is available.
A Comprehensive Approach to Treatment
A Paleo diet is an excellent initial approach to dealing with eczema. This is because a Paleo diet reduces inflammation and heals the gut. Certain nutrients can also be extremely helpful (in general, the same nutrients required for wound healing, see Nutritional Support for Injury and Wound Healing).
Including glycine-rich foods like homemade bone broth and organ meat can help speed the healing of both the gut and the skin. Glycine is an essential component of connective tissue and the extracellular matrix that acts as a scaffold for cells. See Why Broth is Awesome, The Health Benefits of Bone Broth, Broth: Hidden Dangers in a Healing Food? and Bone Broth Risks: Skim the Fat!).
Addressing vitamin D deficiency is also very important; see Vitamin D. Sun exposure and eating vitamin D-rich foods such as fish and organ meat can be very helpful in speeding healing (you might also consider a Vitamin D3 supplement, but check with your doctor first). Consuming plenty of oily cold-water fish (at least three times per week) as well as eating grass-fed and pastured meat will also help because the high omega-3 content of these foods (and low omega-6 content) could help resolve inflammation. See Why Grains Are Bad, Part 2, Omega 3 vs. 6 Fats
Anecdotally, most people report alleviation of their symptoms with adoption of a Paleo diet. In extreme cases, or in individuals who do not see alleviation of their symptoms with out-of-the-box Paleo, it may be worth trying the a more therapeutic version of the Paleo diet, such as the Autoimmune Protocol.
Prescription or over-the-counter topical corticosteroid creams may still provide some alleviation of symptoms (most notably the itching) and might be required initially (oral steroids may also be prescribed; see also Steroids: What To Do When You Need Them). Other moisturizers which may help heal the skin faster and relieve itching include extra virgin coconut oil and lotions containing calamine, aloe vera, arnica montana, Vitamin D and/or Vitamin E. I highly recommend the products from The Eczema Company, which are made with science-backed healing all-natural ingredients.
Citations
1 Elias PM and Steinhoff M “Outside-to-Inside” (and Now Back to “Outside”) Pathogenic Mechanisms in Atopic Dermatitis. J Invest Dermatol. 2008 May; 128(5): 1067–1070.
2 Pike MG et. al. Increased intestinal permeability in atopic eczema. J Invest Dermatol. 1986 Feb;86(2):101-4.
3 Boguniewicz M. Atopic dermatitis: beyond the itch that rashes. Immunol Allergy Clin North Am. 2005 May;25(2):333-51.
The original version of this post was written as a collaborative effort between The Paleo Mom Sarah Ballantyne, PhD, scientist turned stay-at-home-mom, and Paleolithic MD Dr. Ernie Garcia, MD, Internal Medicine and Sleep Medicine specialist.