It’s finally autumn! And you know what that means: carving pumpkins, colorful leaves, kids going back to school, apple season and… the imminent threat of catching the stomach flu. Yep, it’s already going around! And I think we can all agree that stomach bugs are absolutely no fun whatsoever.
Flu season tends to rev up this time of year due to the change in weather (common flu viruses as well as other viruses that cause stomach flu-like illness like rotavirus and norovirus all survive and transmit better in cool, low-humidity environments), as well as more pathogens circling among school-age children and getting passed on to their families. So, as summer fades away, it becomes extremely easy to pick up a virus—especially if your immune system is already compromised (hello stress, sleep deprivation, and low vitamin D levels from the vanishing sun!).
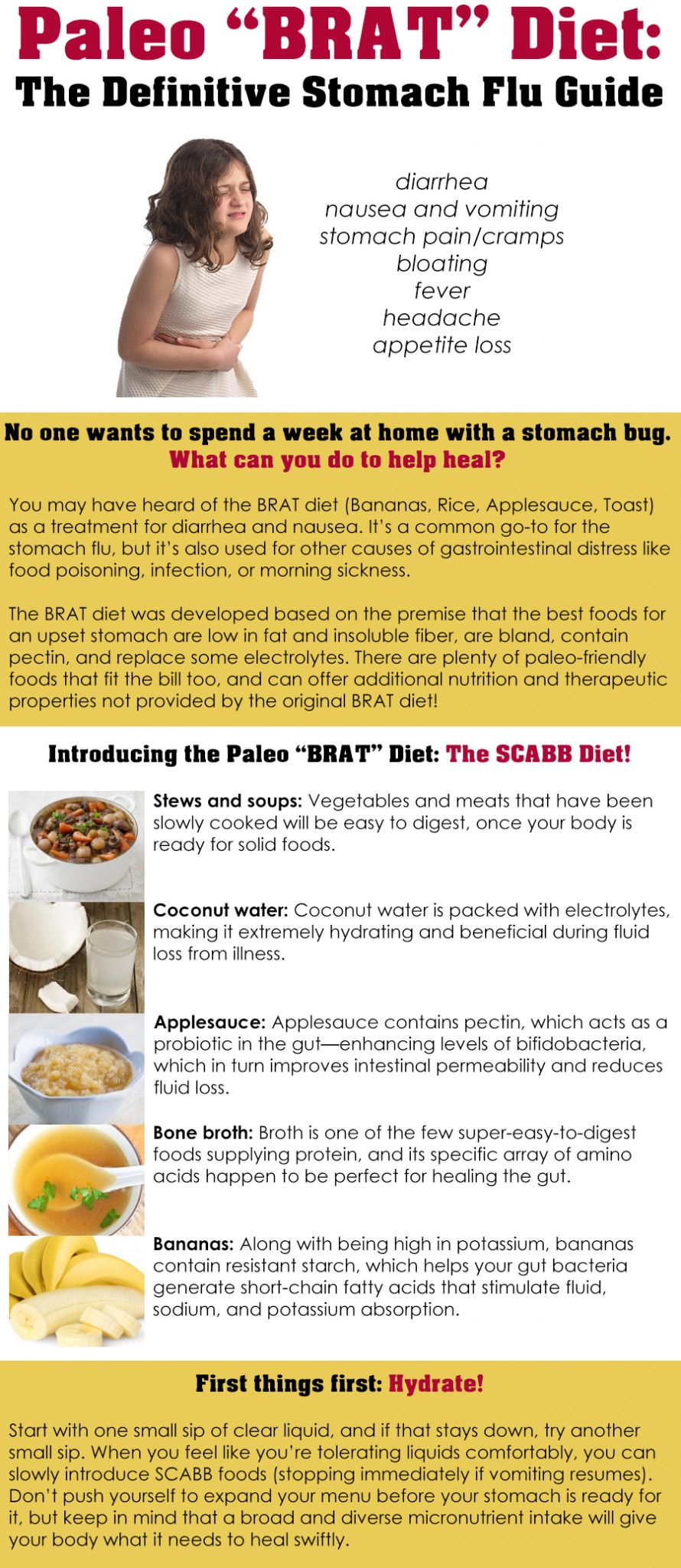
Obviously, no one wants to spend a week or more stuck at home with a nasty stomach bug. What can you do to help heal?
Apart from standard sick-time protocol (Rest! Sleep! Hydrate! Binge watch daytime TV!), nutrition plays a key role in getting better. Your body needs raw materials more than ever in order to repair damage and strengthen immunity. But, staying well-nourished during the stomach flu (technically called “gastroenteritis”) can be particularly challenging, because food tends to either exit rapidly or seem incredibly unpalatable. Plus, diarrhea can do a number on your intestinal mucosa—including blunting the villi, increasing mucosal inflammation, decreasing enzyme and nutrient transport activities, and decreasing absorptive function—which makes it harder to obtain nutrition from the foods you do keep down.
 Enter the BRAT diet! You may have heard of the BRAT diet (standing for Bananas, Rice, Applesauce, and Toast) as a treatment for diarrhea and nausea. It’s a common go-to menu for the stomach flu (especially for children–I even remember my mom following this when I was sick as a kid!!!), but it’s also used for other causes of gastrointestinal distress like food poisoning, infection, or morning sickness.
Enter the BRAT diet! You may have heard of the BRAT diet (standing for Bananas, Rice, Applesauce, and Toast) as a treatment for diarrhea and nausea. It’s a common go-to menu for the stomach flu (especially for children–I even remember my mom following this when I was sick as a kid!!!), but it’s also used for other causes of gastrointestinal distress like food poisoning, infection, or morning sickness.
The BRAT diet was developed based on the premise that the best foods for an upset stomach:
- Are low in fat (since fat delays gastric emptying and slows down digestion)
- Are low in insoluble fiber (low-fiber foods will be more “binding” and help make stools firmer, and are also less likely to irritate the stomach and intestines)
- Are bland (to be more palatable when you’re feeling queasy!)
- Contain pectin (a soluble fiber found in ripe fruits, which combats diarrhea by improving intestinal permeability and reducing fluid loss)
- Supply/replace some electrolytes lost through vomiting and diarrhea (potassium, magnesium, sodium, and calcium)
That said, living on only four foods obviously isn’t a great way to get an abundance and diversity of nutrients, which is why the BRAT diet is only intended as a temporary treatment for acute diarrhea and as a first entrance back into the world of solid foods after vomiting has ceased (until a wider range of foods can be tolerated). In fact, some pediatricians and other doctors are no longer recommending the BRAT diet due to fears that its low protein and micronutrient content will impair healing rather than expedite it.
Of course, if you’re eating Paleo (which I generally assume you are if you’re reading my articles) and avoiding grains (and therefore rice and toast), the BRAT diet gets whittled down even further into, yes, the BA diet (bananas and applesauce). And, no offense to fruit, is a pretty depressing menu for someone who already isn’t feeling well!
Aside: Although Paleo-friendly toast might seem like a tempting addition (if only for the comfort food vibe), Paleo breads tend to be made with extremely hard-to-digest, high-fiber ingredients that will probably aggravate intestinal inflammation instead of quelling it. So, it’s better to save the toast for when you’re on the mend and your stomach doesn’t need so much pampering.
The good news is there’s nothing inherently magical about bananas, rice, applesauce, and toast; they just happen to be already-familiar items from the Standard American Diet that meet the criteria from the list above. There are plenty of Paleo-friendly foods that fit the bill too, and can offer additional nutrition and therapeutic properties not provided by the original BRAT diet.
In fact, we know a lot more about gut health now than when the BRAT diet was originally developed, so we can apply our scientific advancements to improve the diet even more. For instance, we have growing research showing the beneficial effects of certain amino acids in healing the gut (especially glycine, glutamine and arginine), the importance of protein for contracting the lower esophageal sphincter (which helps stop vomiting! Also take note that protein can help quell morning sickness!), as well as the role of certain nutrients in maintaining gut integrity and immune function (like my favorite mineral, and the second most abundant mineral in the human body, zinc).
All that said: how can we design a Paleo-friendly diet with the same soothing effects as the BRAT diet, and with an even better nutritional profile? Here are some great options!
 Soup/stew. Vegetables and meats that have been slowly, gently cooked in a soup or stew will be tender and easy to digest, once your body is ready for solid foods. This is a great way to get in a wide variety of micronutrients, and if you include stewed beef or lamb, a decent amount of zinc (which boosts immune function and is associated with reduced intestinal permeability and diarrhea duration). Go easy on seasonings (although ginger can be helpful for an upset stomach), and make sure everything has been cooked long enough to become nice and soft—which means no crunchy vegetables or extra-chewy meats! Go ahead and get extra bang for your buck by including some organ meats (adding pureed chicken or rabbit liver is actually a French cooking technique for thickening soups!)
Soup/stew. Vegetables and meats that have been slowly, gently cooked in a soup or stew will be tender and easy to digest, once your body is ready for solid foods. This is a great way to get in a wide variety of micronutrients, and if you include stewed beef or lamb, a decent amount of zinc (which boosts immune function and is associated with reduced intestinal permeability and diarrhea duration). Go easy on seasonings (although ginger can be helpful for an upset stomach), and make sure everything has been cooked long enough to become nice and soft—which means no crunchy vegetables or extra-chewy meats! Go ahead and get extra bang for your buck by including some organ meats (adding pureed chicken or rabbit liver is actually a French cooking technique for thickening soups!) Coconut water. Coconut water is basically nature’s Gatorade, packed full of electrolytes (particularly potassium and magnesium), making it extremely hydrating and beneficial during periods of fluid loss from illness. It’s even been used intravenously in lieu of medical hydration fluid (though I definitely don’t recommend trying that at home!). Maple water is another great option here with many of the same electrolytes and a little less sugar.
Coconut water. Coconut water is basically nature’s Gatorade, packed full of electrolytes (particularly potassium and magnesium), making it extremely hydrating and beneficial during periods of fluid loss from illness. It’s even been used intravenously in lieu of medical hydration fluid (though I definitely don’t recommend trying that at home!). Maple water is another great option here with many of the same electrolytes and a little less sugar. Applesauce. Applesauce contains a special soluble fiber called pectin, which acts as a probiotic in the gut—enhancing levels of bifidobacteria, balancing the gut microflora, and reducing inflammation, which in turn improves intestinal permeability and reduces fluid loss. Because fresh apples (especially their skin) contain cellulose, cooking them into applesauce will be easier on your stomach than eating them raw, due to heat’s ability to break down cellulose (peeling is clearly helpful too!).
Applesauce. Applesauce contains a special soluble fiber called pectin, which acts as a probiotic in the gut—enhancing levels of bifidobacteria, balancing the gut microflora, and reducing inflammation, which in turn improves intestinal permeability and reduces fluid loss. Because fresh apples (especially their skin) contain cellulose, cooking them into applesauce will be easier on your stomach than eating them raw, due to heat’s ability to break down cellulose (peeling is clearly helpful too!). Bone broth. Bone broth can play an incredibly important role during the stomach flu for two reasons: it’s one of the few super-easy-to-digest foods supplying protein, and its specific array of amino acids (particularly glycine, glutamine and arginine) happen to be perfect for healing the gut. Glycine aids digestion by regulating synthesis of bile salt and secretion of gastric acid, and can help regulate the immune system. Arginine can help reduce mucosal inflammation related to gastroenteritis (as well as from other conditions, like irritable bowel disease). Glutamine serves as important fuel for intestinal cells, assisting in the maintenance and repair of gastrointestinal mucosa—especially during periods of low food intake and high metabolic demands, when glutamine becomes a conditionally essential amino acid. And in case that wasn’t enough, bone broth also contains minerals (including calcium, phosphorus, and magnesium, although it’s a myth that bone broth has more calcium than milk) to help boost micronutrient intake on a limited diet.
Bone broth. Bone broth can play an incredibly important role during the stomach flu for two reasons: it’s one of the few super-easy-to-digest foods supplying protein, and its specific array of amino acids (particularly glycine, glutamine and arginine) happen to be perfect for healing the gut. Glycine aids digestion by regulating synthesis of bile salt and secretion of gastric acid, and can help regulate the immune system. Arginine can help reduce mucosal inflammation related to gastroenteritis (as well as from other conditions, like irritable bowel disease). Glutamine serves as important fuel for intestinal cells, assisting in the maintenance and repair of gastrointestinal mucosa—especially during periods of low food intake and high metabolic demands, when glutamine becomes a conditionally essential amino acid. And in case that wasn’t enough, bone broth also contains minerals (including calcium, phosphorus, and magnesium, although it’s a myth that bone broth has more calcium than milk) to help boost micronutrient intake on a limited diet. Bananas. Although the original BRAT diet was based more on theory than controlled trials, bananas’ place in an anti-diarrhea diet is well deserved! Along with being high in potassium (an electrolyte easily lost during episodes of vomiting and diarrhea), bananas contain resistant starch, which helps your gut bacteria generate short-chain fatty acids that stimulate fluid, sodium, and potassium absorption (more on resistant starch here). Bananas can therefore help with hydration and electrolyte replenishment in a big way.
Bananas. Although the original BRAT diet was based more on theory than controlled trials, bananas’ place in an anti-diarrhea diet is well deserved! Along with being high in potassium (an electrolyte easily lost during episodes of vomiting and diarrhea), bananas contain resistant starch, which helps your gut bacteria generate short-chain fatty acids that stimulate fluid, sodium, and potassium absorption (more on resistant starch here). Bananas can therefore help with hydration and electrolyte replenishment in a big way.
So there you have it: soup, coconut water, applesauce, broth, and bananas. The SCABB diet! That’s pretty catchy, right?
As with the standard BRAT diet, it’s better not to jump immediately from an episode of vomiting and diarrhea straight into solid foods. Baby steps are key! When you’re in the throes of major digestive distress, focus first on staying hydrated—since you’ll be losing lots of fluid and need to replenish both water and electrolytes. Start with one small sip of clear liquid (coconut water or broth are great here), and if that stays down, wait a while (my rule with my kids is 20 minutes) and then try another small sip. When you feel like you’re tolerating liquids comfortably, you can slowly introduce other SCABB foods (stopping immediately if vomiting resumes). As your stools become more solid, you can also begin introducing non-SCABB foods, saving very high-fiber items (like raw vegetables) for last. Don’t push yourself to expand your menu before your stomach is really ready for it, but keep in mind that a broad and diverse micronutrient intake will give your body what it needs to heal swiftly.
And lastly, an important disclaimer! While most stomach flus will subside on their own without complication, be sure to seek medical attention if you’re experiencing diarrhea that lasts more than three days, a sustained fever of 102F or higher, blood in your stools or in your vomit, or symptoms of dehydration (reduced urine, weakness lightheadedness, heart palpitations, very dry mouth or no tears). Those can all be signs of something more serious, and severe dehydration can land you in the hospital if left untreated.
I won’t pretend that getting the stomach flu is ever a walk in the park, but eating a Paleo-ified SCABB diet (and giving yourself plenty of time to sleep and take it easy!) can help shortening the duration of your symptoms and get you back on your feet in record time. So, sip that bone broth and turn on The Price is Right, and let your body do the rest!
Citations
Adams W & Bratt DE. “Young coconut water for home rehydration in children with mild gastroenteritis.” Trop Geogr Med. 1992 Jan;44(1-2):149-53.
Binder HJ, et al. “Oral rehydration therapy in the second decade of the twenty-first century.” Curr Gastroenterol Rep. 2014 Mar;16(3):376.
Campbell-Falck D. “The intravenous use of coconut water.” Am J Emerg Med. 2000 Jan;18(1):108-11.
“Diet for Nausea, Vomiting, or Diarrhea (BRAT diet).” The Oregon Clinic. Accessed September 2015.
Duggan C, et al. “Protective nutrients and functional foods for the gastrointestinal tract.” Am J Clin Nutr. 2002 May;75(5):789-808.
Duro D & Duggan C. “The BRAT Diet for Acute Diarrhea in Children: Should it Be Used?” Practical Gastroenterology. 2007 Jun;51:60-68.
Rabbani GH, et al. “Green banana and pectin improve small intestinal permeability and reduce fluid loss in Bangladeshi children with persistent diarrhea.” Dig Dis Sci. 2004 Mar;49(3):475-84.
Ruppin H, et al. “Absorption of short-chain fatty acids by the colon.” Gastroenterology. 1980 Jun;78(6):1500-7.
Xu L, et al. “Efficacy of pectin in the treatment of diarrhea predominant irritable bowel syndrome.” Zhonghua Wei Chang Wai Ke Za Zhi. 2015 Mar;18(3):267-71.