As many of us know first-hand, asthma and allergies affect huge portions of the population (about 8% of Americans have asthma, and allergies affect as many as 30% of adults and 40% of children!). Unfortunately, the drugs prescribed to treat these conditions can have serious side effects, and in some cases, become rapidly less effective with repeated use (a phenomenon known as tachyphylaxis). The good news? Dietary changes that reduce inflammation and regulate the body’s immune response can improve asthma and allergies without harmful side effects. And while we don’t have any studies looking specifically evaluating the merits of Paleo for asthma and allergies (yet! see Paleo Diet Clinical Trials and Studies), we can use the available evidence to modify the Paleo diet in ways that give asthma and allergy sufferers some relief!
Table of Contents[Hide][Show]
Dietary Fiber
 In case we need yet another reason to embrace fiber, here it is! The short-chain fatty acids produced when our gut microbes metabolize fiber may suppress airway inflammation, leading to improvements in asthma symptoms. One study in mice found that a high-fiber diet increased the production of acetate (a short-chain fatty acid) in the gut, in turn enhancing in the number and function of T-regulatory cells (acetate increases acetylation at the Foxp3 promoter) and suppressing the animals’ allergic airway disease (the equivalent of human asthma). Another rodent study found that increasing the fermentable fiber content of the diet altered the gut and lung microbiomes, leading to higher levels of circulating short-chain fatty acids, and in turn protecting against allergic inflammation in the lung (in contrast to a low-fiber diet, which increased allergic lung inflammation). Likewise, the immune-regulating effects of short-chain fatty acids appear to benefit both food allergies and environmental allergies. Although we’re just beginning to understand the role of our bodies’ resident microbes in asthma and allergies, the evidence so far is compelling!
In case we need yet another reason to embrace fiber, here it is! The short-chain fatty acids produced when our gut microbes metabolize fiber may suppress airway inflammation, leading to improvements in asthma symptoms. One study in mice found that a high-fiber diet increased the production of acetate (a short-chain fatty acid) in the gut, in turn enhancing in the number and function of T-regulatory cells (acetate increases acetylation at the Foxp3 promoter) and suppressing the animals’ allergic airway disease (the equivalent of human asthma). Another rodent study found that increasing the fermentable fiber content of the diet altered the gut and lung microbiomes, leading to higher levels of circulating short-chain fatty acids, and in turn protecting against allergic inflammation in the lung (in contrast to a low-fiber diet, which increased allergic lung inflammation). Likewise, the immune-regulating effects of short-chain fatty acids appear to benefit both food allergies and environmental allergies. Although we’re just beginning to understand the role of our bodies’ resident microbes in asthma and allergies, the evidence so far is compelling!
So, what does this mean for our food choices? Although a well-designed Paleo diet will naturally be loaded with fiber, emphasizing sources of fermentable fiber (the type of fiber our gut microbes can metabolize into short-chain fatty acids) is the best bet for battling asthma and allergies. Rich sources include allium vegetables (garlic, onions, leeks, scallions, shallots), bananas (especially green or under-ripe bananas), Jerusalem artichokes, potatoes (especially potatoes that have been cooked and cooled down to room temperature), nuts, berries, plantains, and cassava. See also 5 Reasons to Eat More Fiber.
Vitamin D
 Low vitamin D levels have been convincingly linked to increased risk of asthma attacks in both children and adults (and, although the evidence is much less clear, might impact allergy risk due to vitamin D’s role in immune function). One study found that Canadians with vitamin D levels lower than 20 ng/mL were 50% more likely to have asthma than people with vitamin D levels between 20 ng/mL and 30 ng/mL. A 2016 Cochrane Review (involving seven studies of children and two studies of adults, lasting six months to a year) found that vitamin D supplementation significantly reduced the number of asthma attacks requiring a hospital visit, and also reduced the number of asthma attacks that needed to be treated with steroids. In addition, vitamin D may indirectly benefit asthmatics by helping protect against colds and flus, both of which can trigger or worsen asthma.
Low vitamin D levels have been convincingly linked to increased risk of asthma attacks in both children and adults (and, although the evidence is much less clear, might impact allergy risk due to vitamin D’s role in immune function). One study found that Canadians with vitamin D levels lower than 20 ng/mL were 50% more likely to have asthma than people with vitamin D levels between 20 ng/mL and 30 ng/mL. A 2016 Cochrane Review (involving seven studies of children and two studies of adults, lasting six months to a year) found that vitamin D supplementation significantly reduced the number of asthma attacks requiring a hospital visit, and also reduced the number of asthma attacks that needed to be treated with steroids. In addition, vitamin D may indirectly benefit asthmatics by helping protect against colds and flus, both of which can trigger or worsen asthma.
So, how much vitamin D should we be taking? There’s no clear answer! The optimal dosage will vary depending on a person’s baseline vitamin D status, latitude, sun exposure, age, and other factors. In general, whatever intake is needed to boost vitamin D levels out of the deficiency range will likely have a positive effect on asthma (and potentially allergies). Although small amounts of vitamin D exist in some foods (such as fatty fish and liver), the levels are generally too low to meet our daily needs, especially for people living at high latitudes.
About 75% of Westerners are deficient in vitamin D, and correcting this deficiency is key for mitigating chronic disease risk across the board. Optimal serum vitamin D levels are between 50 and 70 ng/mL. It’s important to ask your health-care provider test your levels, and if you’re deficient, consider supplementing (your doctor may recommend anywhere from 500 IU to 5000 IU daily to address deficiency) and recheck every three months to make sure you don’t overshoot the mark. Vitamin D levels in excess of 100 ng/mL can also cause health problems. See also Vitamin D, Fructose and Vitamin D Deficiency: The Perfect Storm?, and Why Sun Exposure Is So Important.
Omega-3 Fats
 Due to their role in regulating inflammation, omega-3 fats (and the overall omega-3/omega-6 ratio of the diet) may influence the occurrence and severity of asthma and allergies. (In fact, some researchers speculate that the sky-high intake of omega-6 fats relative to omega-3 fats is one reason why America and other Western nations have such high rates of asthma!) Several trials have confirmed that omega-3 supplements (in the form of fish oil) can reduce exercise-induced bronchoconstriction in asthma, and research shows that an omega-3/omega-6 ratio of 1:5 has a beneficial effect on patients with asthma (whereas a ratio of 1:10 becomes detrimental). Likewise, omega-3 fats express an anti-allergic effect through conversion into certain metabolites (particularly 17,18-epoxyeicosatetraenoic acid) in the gut, helping explain the role of omega-3 in reducing allergy risk.
Due to their role in regulating inflammation, omega-3 fats (and the overall omega-3/omega-6 ratio of the diet) may influence the occurrence and severity of asthma and allergies. (In fact, some researchers speculate that the sky-high intake of omega-6 fats relative to omega-3 fats is one reason why America and other Western nations have such high rates of asthma!) Several trials have confirmed that omega-3 supplements (in the form of fish oil) can reduce exercise-induced bronchoconstriction in asthma, and research shows that an omega-3/omega-6 ratio of 1:5 has a beneficial effect on patients with asthma (whereas a ratio of 1:10 becomes detrimental). Likewise, omega-3 fats express an anti-allergic effect through conversion into certain metabolites (particularly 17,18-epoxyeicosatetraenoic acid) in the gut, helping explain the role of omega-3 in reducing allergy risk.
Although a number of studies on omega-3 fats, asthma, and allergies have used supplements such as fish oil to boost omega-3 intake, consuming these fats in whole-food form may offer even more benefit by providing a matrix of additional nutrients that can boost immunity and suppress inflammation (such as vitamin E in omega-3-rich walnuts). For combating asthma and allergies, fatty fish (including salmon, mackerel, tuna, sardines) and walnuts can be helpful dietary additions. See also Why Grains Are Bad – Part 2, Omega 3 vs. 6 Fats and The Importance of Fish in Our Diets.
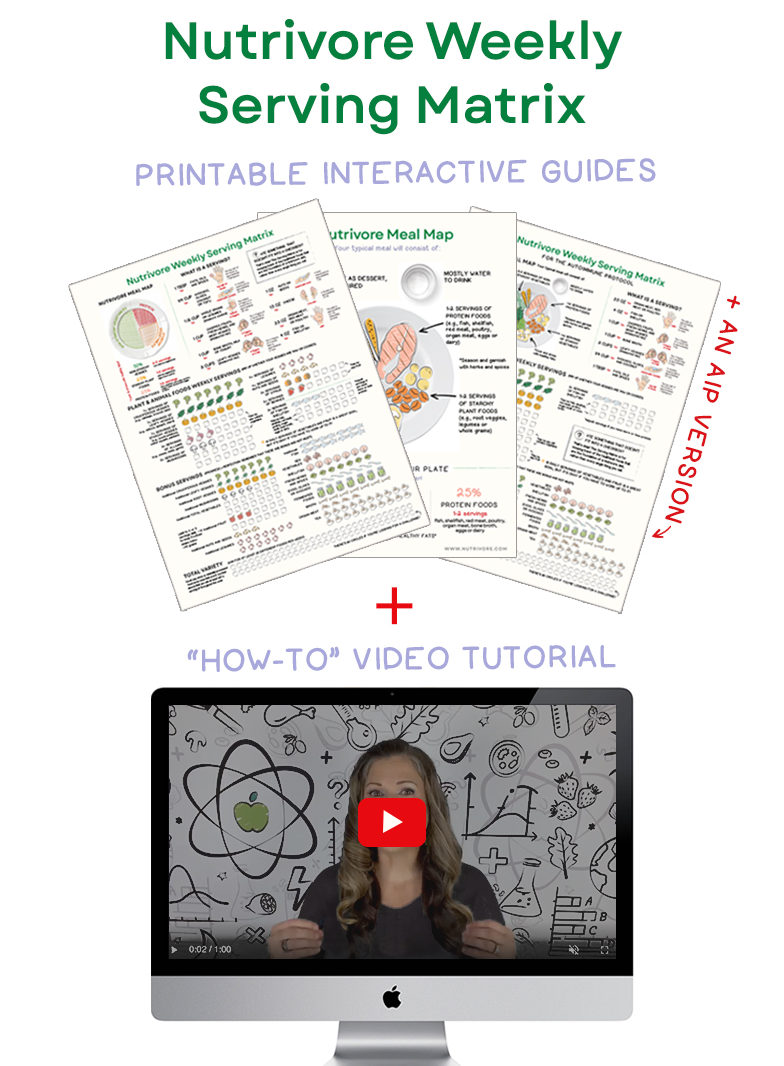
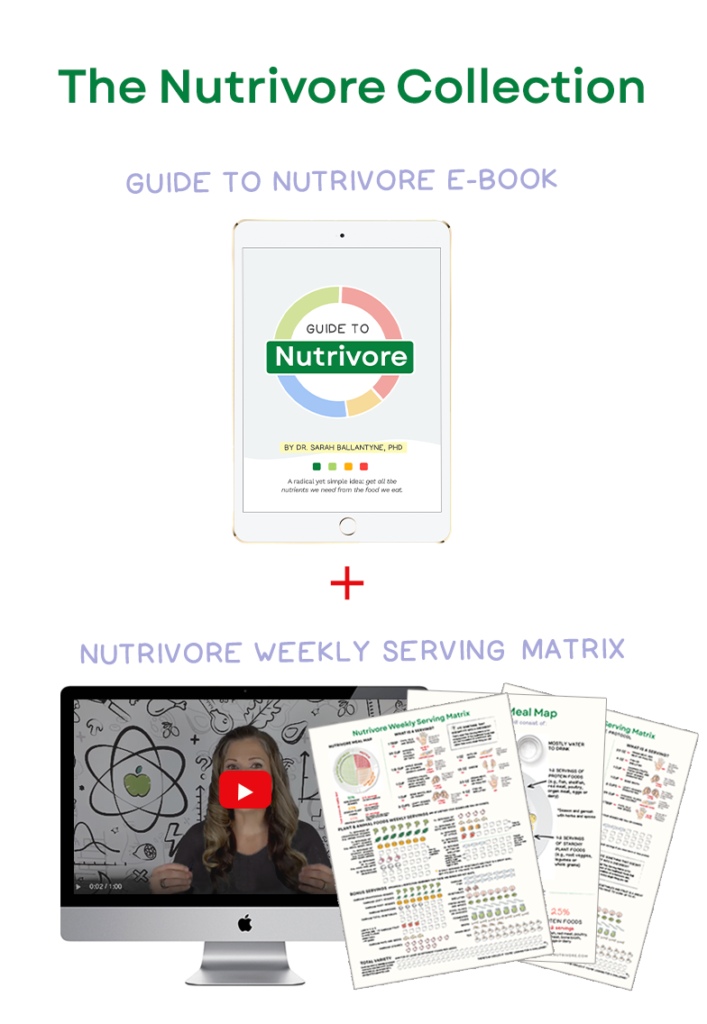
Nutrivore Weekly Serving Matrix
An easy-to-use and flexible weekly checklist
to help you maximize nutrient-density.
The Weekly Serving Matrix is very helpful! I’ve been eating along these lines but this really helps me know where to focus vs. which foods serve a more secondary role. It’s super helpful and has taken a lot of worry out of my meal planning. Thanks!
Jan
Diet During Pregnancy
 As the saying goes, “an ounce of prevention is worth a pound of cure,” and this might be particularly true when it comes to asthma and allergies! Reducing asthma and allergy risk prenatally can help protect against a lifetime of battling these conditions. Research continues to highlight the role of a mother’s diet during pregnancy on the immune and airway development of the fetus, and consequently, the risk of childhood asthma and allergies. Several studies suggest a link between low intake of vitamin D, vitamin E, zinc, selenium, and omega-3 fats during pregnancy and greater risk of asthma after the child is born. Expectant mothers may be able to reduce their child’s risk of asthma by eating a nutrient-dense diet during pregnancy, with a particular emphasis on low-mercury fatty fish (see The Mercury Content of Seafood: Should we worry?), vitamin D supplements, Brazil nuts (an extremely rich source of selenium!), and organ meats and shellfish (high in zinc).
As the saying goes, “an ounce of prevention is worth a pound of cure,” and this might be particularly true when it comes to asthma and allergies! Reducing asthma and allergy risk prenatally can help protect against a lifetime of battling these conditions. Research continues to highlight the role of a mother’s diet during pregnancy on the immune and airway development of the fetus, and consequently, the risk of childhood asthma and allergies. Several studies suggest a link between low intake of vitamin D, vitamin E, zinc, selenium, and omega-3 fats during pregnancy and greater risk of asthma after the child is born. Expectant mothers may be able to reduce their child’s risk of asthma by eating a nutrient-dense diet during pregnancy, with a particular emphasis on low-mercury fatty fish (see The Mercury Content of Seafood: Should we worry?), vitamin D supplements, Brazil nuts (an extremely rich source of selenium!), and organ meats and shellfish (high in zinc).
Although a number of genetic and environmental factors contribute to asthma and allergies, a modified Paleo diet may help bring relief for these conditions!
Citations
Allan K & Devereux G. “Diet and asthma: nutrition implications from prevention to treatment.” J Am Diet Assoc. 2011 Feb;111(2):258-68. doi: 10.1016/j.jada.2010.10.048.
“Allergy Facts.” American College of Allergy, Asthma and Immunology. http://acaai.org/news/facts-statistics/allergies. Accessed March 28, 2017.
“Asthma Statistics.” American Academy of Allergy, Asthma and Immunology. http://www.aaaai.org/about-aaaai/newsroom/asthma-statistics. Accessed March 28, 2017.
Devereux G. “Maternal diet during pregnancy: an emerging risk factor for childhood asthma.” Expert Rev Clin Immunol. 2008 Nov;4(6):663-8. doi: 10.1586/1744666X.4.6.663.
Kelley CP, et al. “Vitamin D as an adjunctive therapy in asthma. Part 2: A review of human studies.” Pulm Pharmacol Ther. 2015 Jun;32:75-92.
Kunisawa J, et al. “Dietary ω3 fatty acid exerts anti-allergic effect through the conversion to 17,18-epoxyeicosatetraenoic acid in the gut.” Sci Rep. 2015 Jun 11;5:9750.
McCoy KD & Köller Y. “New developments providing mechanistic insight into the impact of the microbiota on allergic disease.” Clin Immunol. 2015 Aug; 159(2): 170–176.
Mickleborough TD. “Dietary omega-3 polyunsaturated fatty acid supplementation and airway hyperresponsiveness in asthma.” J Asthma. 2005 Jun;42(5):305-14.
Mickleborough TD, et al. “Omega-3 Fatty acids and airway hyperresponsiveness in asthma.” J Altern Complement Med. 2004 Dec;10(6):1067-75.
Niruban SJ, et al. “Association between vitamin D and respiratory outcomes in Canadian adolescents and adults.” J Asthma. 2015 Sep;52(7):653-61.
Reuter S, et al. “Mast Cells in Allergic Asthma and Beyond.” Yonsei Med J. 2010 Nov 1; 51(6): 797–807.
Searing DA & Leung D. “Vitamin D in Atopic Dermatitis, Asthma and Allergic Diseases.” Immunol Allergy Clin North Am. 2010 Aug;30(3):397-409.
Simopoulos A. “Omega-6/Omega-3 Essential Fatty Acid Ratio and Chronic Diseases.” Food Reviews International. 2004;20(1):77-90.
Thorburn AN, et al. “Evidence that asthma is a developmental origin disease influenced by maternal diet and bacterial metabolites.” Nat Commun. 2015 Jun 23;6:7320. doi: 10.1038/ncomms8320.
Trompette A, et al. “Gut microbiota metabolism of dietary fiber influences allergic airway disease and hematopoiesis.” Nature Medicine. 2014;20:159-166.
Yamada K, et al. “Effect of dietary fiber on the lipid metabolism and immune function of aged Sprague-Dawley rats.” Biosci Biotechnol Biochem. 2003 Feb;67(2):429-33.
Zaknun D, et al. “Potential role of antioxidant food supplements, preservatives and colorants in the pathogenesis of allergy and asthma.” Int Arch Allergy Immunol. 2012;157(2):113-24.