Health is impacted by much more than what you eat. Health is also influenced by how you live. How active you are, how much you sleep, how much stress you’re under, how much time you spend outside and in nature…. all these things have just as much of an impact on your physical and emotional health as the foods on your plate.
I cannot stress enough (pardon the pun) the negative impact that chronic stress has on your health. In fact, stress contributes to the development and/or worsens all disease, from increasing susceptibility to the common cold to being a major contributor to stimulating the immune system in autoimmune disease. Stress is a bigger predictor of cardiovascular disease than any other factor.
Chronic stress is known to affect health in a variety of ways, including causing the development of metabolic syndrome (the nasty combination of obesity, insulin resistance, and high blood pressure), dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis along with sympathetic nervous system activation, sleep disturbances, systemic inflammation, impaired immunity functions, blood coagulation and fibrinolysis, and poor health behaviors (chronic stress causes increased appetite, cravings for energy-dense foods, and uninhibited eating behaviors). Whether you’re looking to lose a few pounds, increase performance at the gym, or manage a chronic health problem, stress management is critical for your success.
Save 80% Off the Foundations of Health
Expand your health knowledge on a wide range of topics relevant to you, from how to evaluate scientific studies, to therapeutic diet and lifestyle, to leaky gut and gut microbiome health, to sustainable weight loss, and much more!!!

What Is Stress?
The hypothalamic-pituitary-adrenocortical axis (the HPA axis) is responsible for the flight-or-fight response, i.e., how the body responds to stress. And, a stressor is a chemical or biological agent, environmental condition, external stimulus or an event that activates the hypothalamic-pituitary-adrenal axis (HPA axis), causing the release of stress hormones.
The HPA axis is made up of the complex communication between three organs:
- The hypothalamus: The part of the brain located just above the brain stem and responsible for a variety of activities of the autonomic nervous system, such as regulating body temperature, hunger, thirst, fatigue, sleep, and circadian rhythms
- The pituitary gland: A pea-shaped gland located below the hypothalamus that secretes a variety of important hormones, such as thyroid-stimulating hormone, human growth hormone, and adrenocorticotropic hormone
- The adrenal glands: Small, conical organs on top of the kidneys that secrete a variety of hormones, such as cortisol, epinephrine (also known as adrenaline), norepinephrine, and androgens
The hypothalamus (which receives signals from the hippocampus, the region of the brain that amalgamates information from all the senses and can thus perceive danger and make decisions) releases a hormone called Corticotrophin Releasing Hormone (CRH), which signals to the pituitary gland to release a hormone called Adrenocorticotropic Hormone (ACTH), which signals to the adrenal glands to secrete cortisol as well as catecholamines (like adrenalin).
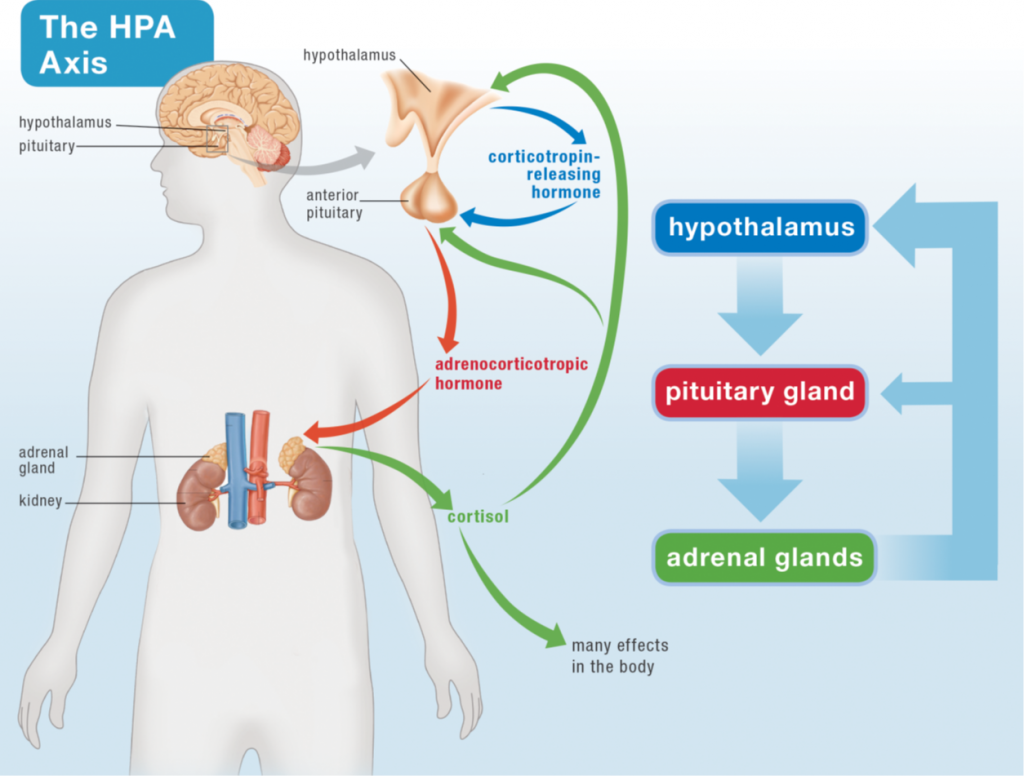
Cortisol has a huge range of effects in the body, including controlling metabolism, affecting insulin sensitivity, affecting the immune system, and even controlling blood flow. If you’re running away from a lion, all these effects (including the combined effects of catecholamines and some direct effects of CRH) combine to prioritize the most essential functions for survival (perception, decision making, energy for your muscles so you can run away or fight for your life, and preparation for wound healing) and inhibit non-essential functions (like some aspects of the immune system especially not in the skin, digestion, kidney function, reproductive functions, growth, collagen formation, amino acid uptake by muscle, protein synthesis and bone formation).
Cortisol also provides a negative feedback to the pituitary and the hypothalamus. It’s the body’s way of saying “hey, we got the signal that we’re supposed to be stressed now, thanks, we’re on it!”. If the stressful event has ceased (the lion gave up and left), this is what deactivates the HPA Axis. Of course, if a stressor is still being perceived (that lion is still there), the HPA axis remains activated. And this is why chronic stress (deadlines, traffic, sleep deprivation, teenagers, divorce, being sick, being inflamed, alarm clocks, bills, and internet trolls) is such a problem. All those essential functions suppressed by high cortisol never get a chance to be prioritized.
Stressors can be categorized in terms as follows:
- Physical (e.g., injury, a vigorous workout, sitting for prolonged periods, not getting enough sleep, extreme environmental temperatures)
- Sensory (e.g., loud noises, too-bright lights, overcrowding)
- Chemical (e.g., tobacco, alcohol, drugs, allergens)
- Psychological (e.g., deadlines, traffic, bills, societal and family demands)

It’s also important to differentiate between acute stress and chronic stress.
Historically, all stress was acute and would include situations such as being chased by a lion or slipping off the edge of a cliff. During these events, the fight-or-flight response is activated, and cortisol and adrenaline work together to ensure survival. At the end of the event, you are either dead (because you fell from the cliff onto craggy rocks four hundred feet below) or alive and safe (because you grabbed onto a branch as you slipped off the cliff and pulled yourself back up to safety). In either case, there is no need for the body to continue producing adrenaline and excess cortisol (more on this below). Levels return to normal (unless you’re dead, of course), and you go on your merry way.
Chronic stress is that unrelenting stress that never goes away. It can be at a low level, perhaps the stresses we all experience from having a job, raising kids, and having to make ends meet. It can be moderate, perhaps from an impending deadline or exam, your kids getting into trouble at school, or ripping your favorite shirt. It can also be high, such as illness, divorce, or a death in the family. What’s different about chronic stress is that it’s never over. There’s no big relief at the end before you go on your merry way. It’s always there, having its insidious effects that build up over time. How quickly and severely the effects of chronic stress are felt depends on the severity of the stress and your resilience (more on that below too).
How Stress Contributes to Disease
Chronic stress increases the risk of depression and anxiety, cardiovascular disease, obesity, diabetes, autoimmune diseases, chronic headaches, memory problems, digestive problems, and infections and is linked with poor wound healing. These effects are believed to be mediated by the activation of the HPA axis and the impact that cortisol and other adrenal hormones have on immune function. Plus, chronic stress influences other behaviors, influencing our food choices (due to cravings for energy-dense foods and increased appetite) and making us more vulnerable to addiction.
The best understood mechanism is the impact of stress on the immune system. Inflammation is a component of every disease, or every health condition. Worse, it’s part of the pathogenesis–meaning how a disease develops–of every chronic health condition. Inflammation is controlled (or at least is supposed to be controlled) by the immune system. This doesn’t mean that inflammation is the sole causes of chronic disease, but that it is necessary for chronic disease to develop. If you regulate the immune system so that there is not inflammation, you prevent the disease.
The same is true of stress. It’s not the sole cause (at least, there isn’t any research to prove that it is). Bur rather, it contributes to the development of disease, so if you suffer from chronic stress, you increase your risk of getting sick. In order to understand how being stuck in traffic or a deadline at work can directly impact how your immune system functions, it helps to describe what’s happening physiologically inside your body when you’re late for an important meeting at work.
Cortisol and the Immune System
 Cortisol has profound effects on the immune system and is required for normal wound healing and for fighting infection. Studies have shown that acute (short-duration and intense) stressors (like running away from a lion) induce a redistribution of immune cells in the body, resulting in enhanced immune function in organs like the skin. White blood cells are released from bone marrow and travel to the skin during acute stress, most likely in preparation for wound healing. Other aspects of the immune system are activated in anticipation of being needed. In this situation, cortisol enhances the immune system response.
Cortisol has profound effects on the immune system and is required for normal wound healing and for fighting infection. Studies have shown that acute (short-duration and intense) stressors (like running away from a lion) induce a redistribution of immune cells in the body, resulting in enhanced immune function in organs like the skin. White blood cells are released from bone marrow and travel to the skin during acute stress, most likely in preparation for wound healing. Other aspects of the immune system are activated in anticipation of being needed. In this situation, cortisol enhances the immune system response.
However, what is beneficial in acute stress becomes quite the troublemaker during chronic stress. There is a spectrum of responses by the immune system to a high-cortisol environment, probably reflecting different effects at different cortisol levels and in the presence of other chemicals produced by the body and in the context of different levels of sensitivity to cortisol. The waters are murky in terms of the details, but what is universally accepted is that chronic stress causes immune system dysfunction.
Cortisol alters the chemical messengers of inflammation (called cytokines) secreted by cells in the immune system. This changes how the immune system communicates with itself, turning on some aspects of the immune system (like the parts of the immune system that attack foreign invaders or that produce generalized inflammation), while turning off other aspects of the immune system. There are a wealth of studies to show that high cortisol causes inflammation.
The exact response of the immune system to chronic stress seems to depend on other physiologic factors, such as hormones, cytokines, and neurotransmitters, as well as the state of activation of the immune system (like if you’re already fighting a cold virus, for example). Even genes may play a role in how the immune system responds to chronic stress. The immune system is complex and only just beginning to be understood, but the bottom line is that chronic stress greatly diminishes its effectiveness.
Chronic stress has been unequivocally shown to increase susceptibility to a variety of conditions, including autoimmune disease, cardiovascular disease, metabolic syndrome, osteoporosis, depression, infection, and cancer.
Cortisol, CRH and Leaky Gut
What exactly is a “leaky gut”? The gut is a barrier between the inside of your body and the outside world. Yes, as unintuitive as it may be, the stuff inside your digestive tract is actually outside your body. But, the gut is a very unique barrier. Its job is to let important nutrients inside the body while keeping everything else out. This makes it a highly selective semi-permeable barrier. Nutrients enter the body through a variety of tightly controlled mechanisms. See What Is A Leaky Gut? (And How Can It Cause So Many Health Issues?).
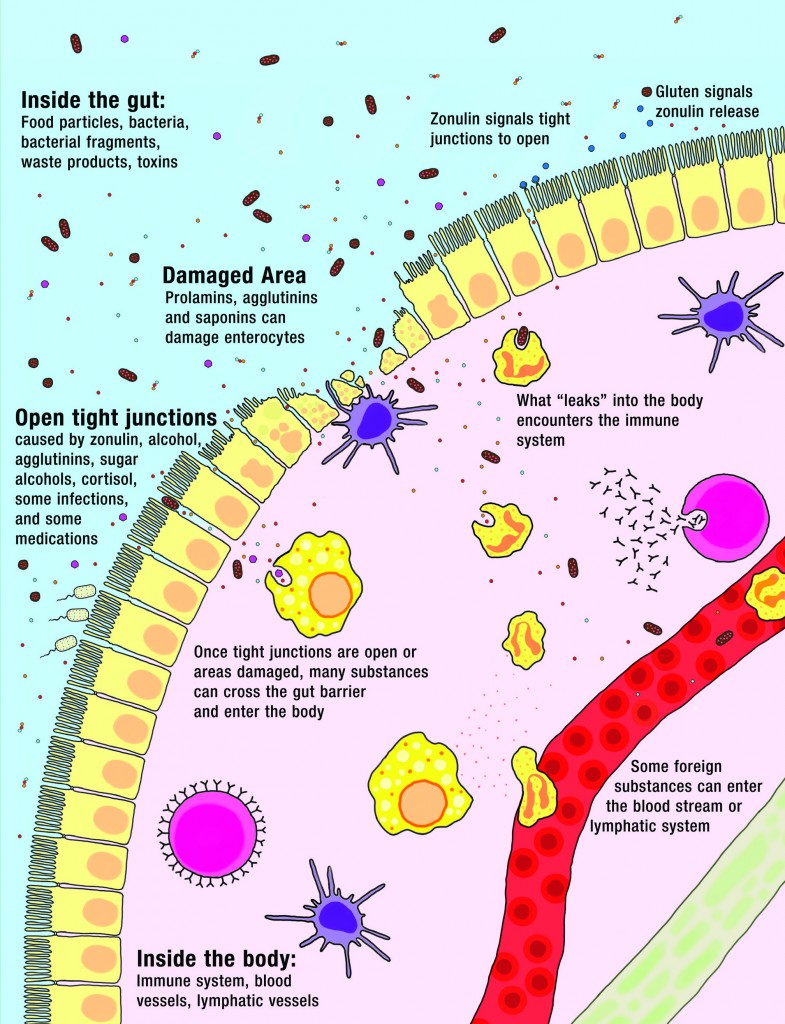
What forms this highly selective semi-permeable barrier is a single layer of highly specialized cells called enterocytes. And right on the other side of that barrier is 80% of our body’s immune systems, acting as a sentinel, ready to attack anything that might try to cross the barrier.
When a person has a leaky gut, or, more technically, “increased intestinal permeability,” things can get across the gut barrier that aren’t supposed to (see also What Should You Eat To Heal a Leaky Gut?). This happens when either the enterocytes or the complex structures that glue the enterocytes together are damaged. The things that leak into the body aren’t big chunks of food, but a variety of small substances—like incompletely digested proteins, bacteria or bacterial fragments, infectious organisms, and waste products—all of which stimulate the immune system on the other side of the barrier. Some of these substances cause generalized bodywide inflammation; for example, bacterial fragments from those good bacteria that live and are supposed to stay in our digestive tracts can travel and stimulate inflammation throughout the body. Others stimulate targeted attacks by the immune system; for example, a food intolerance or allergy could result from incompletely digested proteins leaking into the body. The many symptoms and health conditions related to leaky gut are caused by this stimulation of the immune system.
Chronic stress is detrimental to our health in large part due to the direct effect of both cortisol and CRH on gut health. Chronic stress increases intestinal permeability, decreases gut motility (intestinal muscle contractions), decreases mucus production by goblet cells in the gut, decreases secretory IgA production, inhibits digestion (by inhibiting pancreatic enzyme secretion and gallbladder function), and decreases intestinal blood flow. Both a leaky gut and gut dysbiosis are consequences of these actions.
Cortisol’s actions on the gut epithelial tight junctions are complicated. Low cortisol causes tight junctions to open, whereas normal or high cortisol causes them to close (this implies that cortisol plays a normal role in digestion, which is supported by the fact that cortisol goes up every time we eat). But at very high levels of cortisol, there’s a change in tight junction assembly that makes the gut barrier more permeable to low-molecular-weight substances (small molecules) and less permeable to high-molecular-weight (large molecules) substances.
CRH is the stress hormone that does the biggest damage to our guts. It is known to increase epithelial permeability, not just in the gut, but also in other barrier tissues like the lungs, the skin, and the blood-brain barrier. This appears to be due to a direct effect of CRH on tight junction assembly; CRH increases the expression of a tight junction protein called claudin-2, which opens up tight junctions. CRH also stimulates the release of histamine, a blood thinner called heparin, and proinflammatory cytokines from mast cells (a type of innate immune cell characteristically found in connective and barrier tissues that are major players in allergic reactions, including anaphylaxis), all of which contribute to inflammation.
CRH is perpetually produced by the hypothalamus if the perceived stress continues. This becomes an even bigger problem in the context of adrenal fatigue (discussed in the next section), where the adrenal glands can no longer keep up with demand and cortisol levels begin to fall in proportion to psychological stress. Since cortisol is an important negative feedback signal for CRH production (meaning that cortisol signals to the hypothalamus to produce less CRH), adrenal fatigue and chronic stress lead to even higher levels of CRH.
Given the growing list of health conditions linked to a leaky gut, including the further impact that a leaky gut has on the immune system, this is another checkmark in the need-to-manage-stress column.
Chronic Stress and the Microbiome
We’re also learning that stress can also cause changes to our gut microbiome (see also What Is the Gut Microbiome? And Why Should We Care About It?). Stress-induced shifts in microflora appear to be due largely to hormones and antimicrobial agents produced or mediated by our gut microbes.
In both animal and human studies, the most consistent consequence of stress on the gut is a reduction in Lactobacilli. Physical, physiological, and psychological stressors all lower the abundance of this bacteria in the gut, and some research shows that stress causes Lactobacillus species to translocate to the spleen, where it primes the innate immune system for enhanced reactivity. In a study of 6-month-old rhesus monkeys, separation from the mother (in order to induce stress) caused a significant reduction in Lactobacilli levels, and the magnitude of that reduction among individual monkeys directly corresponded to the magnitude of behavioral changes they exhibited (suggesting the more that stress impacts the gut, the stronger the effect on behavior is).

Stress can also lead to microbiome changes that increase our susceptibility to infection. For example, some pathogenic microbes respond to stress-related hormones with enhanced growth and adhesion to the intestinal lining. The hormones norepinephrine and epinephrine significantly enhance the growth of pathogens Yersinia entercolitica and Escherichia coli, and norepinephrine increases both the growth of enterohemmoraghic E. coli and its ability to adhere to the intestinal epithelium (enterohemmoraghic E. coli is a subset of E. coli that can cause diarrhea or bleeding colitis). In other studies, as early as 24 hours after norepinephrine levels are deliberately elevated, the levels of commensal bacteria that can be cultured from the intestines increase approximately 1000 to 100,000 fold!
Stress during a mother’s pregnancy can affect an infant’s microbiome. In a study of monkeys, maternal stress (in the form of startling noise) caused significant microflora changes during the child’s first six months of life—in particular, a reduction in the overall numbers of Bifidobacteria and Lactobacilli. In humans, mothers with high cumulative stress during pregnancy (gauged in terms of high reported stress and high cortisol concentrations) had significantly higher proportions of bacterial groups known to contain pathogens (including Serratia, Enterobacter, and Escherichia species), as well as lower abundances of Bifidobacteria and lactic acid bacteria (including Lactobacillus, Lactoccus, and Aerococcus). Along with indicating potentially increased levels of inflammation, these microbiota patterns corresponded with higher rates of gastrointestinal symptoms and allergic reactions in the infants after birth.
In one study, researchers likened stress-induced changes in the gut to the “Anna Karenina Principle,” taken from author Leo Tolstoy’s dictum that “all happy families look alike; each unhappy family is unhappy in its own way.” Whereas healthy gut microbiomes tend to have somewhat consistent features, individual gut microbiomes change in unique, non-predictable ways when the host is in a state of stress, exhibiting more individual variation than healthy gut microbiomes.
Managing Chronic Stress
Managing chronic stress is best handled from two sides: reducing stressors and increasing resilience. You can think of it this way: if you have too many apples to fit in your bucket, you can either get rid of some apples (that’s reducing stressors in this analogy) or you can get a bigger bucket (increasing resilience)—or you can do both!
Reducing Stressors
Reducing stressors is a matter of setting boundaries to protect our mental and physical well-being, which can include:
- Reevaluating our goals and priorities to make sure we aren’t taking on more commitments than we really need to
- Saying no to optional activities that would drain us more than benefit us
- Asking for help from our spouse, friends, family, coworkers, or others in our social support network when we’re feeling overwhelmed
- Limiting the presence of negative, stressful people in our lives
- Making more time for sleep (which has the added benefit of increasing resilience)
- Reducing physical and mental stress at work (such as by taking time to stretch and breathe deeply throughout the day, discussing the possibility of a deadline extension or a more flexible schedule, leaving work at work, and finding ways to get up and move—for instance, taking the stairs instead of the elevator)
It’s also helpful to understand that stress is additive. So, that tough workout (physical stressor) adds to your stress load after a tough day at work (psychological stressor). Winding down in the evening with a glass of wine adds a chemical stressor to the equation. Waking up to an alarm clock adds a sensory stressor (not to mention the physical stress of not getting enough sleep). This is why balancing load and recovery is important, see Balancing Physical Activity with Rest: How Do We Get It Right?
Increasing Resilience
Resilience is the ability to adapt in the face of adversity. Because we can never completely eliminate stress from our lives, actively making choices that help bolster our bodies against the effects of stress is an extremely important habit and skill. This doesn’t mean stressful events won’t affect us, but rather that we can handle them without the wheels falling off our cart.
Resilience helps us deal with the unavoidable stressors we encounter throughout life—everything from bad traffic to a massive deadline at work to the death of a loved one. Without resilience, an unexpected or unavoidable stressor could take a serious toll on our health. Certainly, certain personality traits are associated with resilience. However, developing resilience is also about developing coping strategies, establishing healthful routines, and approaching life with a positive attitude.
The healthy habits that increase our resilience to stress can easily be distilled as follows:
- Sleep: Get enough of it and make choices during the day that improve sleep quality, see Sleep and Disease Risk: Scarier than Zombies! and 5 Biohacks for Better Sleep
- Move: Avoid being sedentary and make time for more moderately intense activity (but avoid strenuous activity and overtraining), see The Importance of Exercise, The Benefits of Gentle Movement and Why Exercising Too Much Hurts Your Gut
- Meditate: Take up a daily mindfulness practice (read more below!)
- Play: Make time every day for fun, laughter, and other breaks from stressors like work, see Smile! Better Yet, Laugh!
- Nature: Spend time in nature, even a yard or urban greenspace, see The Health Benefits of Nature
Mindful Meditation
 Meditation may not strike you as a likely subject of scientific investigation, but it’s been thoroughly documented in the scientific literature that mindful meditation dramatically reduces stress and boosts cognitive abilities.
Meditation may not strike you as a likely subject of scientific investigation, but it’s been thoroughly documented in the scientific literature that mindful meditation dramatically reduces stress and boosts cognitive abilities.
Mindful meditation—sometimes called mindful breathing practice or mindfulness—may be one of the most powerful stress management tools we have in our arsenal. Besides the fact that we can reap huge benefits with a relatively short time commitment (studies show benefits even with only 10 minutes of mediation), it can be practiced anywhere at any time by just about anybody. Essentially, mindful meditation entails sitting and focusing on your breath for a set amount of time. You concentrate on your breath so that your mind doesn’t wander.
Mindful meditation is fairly simple. Choose a comfortable position—sitting, reclining, or lying down. Keep your attention on your breath. You might find it easier to maintain focus by doing a breathing technique that requires mental control, like equal breathing, diaphragmatic breathing, or alternate-nostril breathing. Alternatively, you can simply breathe as deeply and slowly as possible or “watch” your breath while trying not to control it (which is harder than it sounds). As thoughts come to you and vie for your attention, acknowledge them (“Yes, I know I have to do the dishes when I’m done” or “Yes, yellow would be the perfect color for the kitchen walls”) and then consciously let them go and bring your attention back to your breath. In many ways, mindful mediation is the practice of stopping repetitive or obsessive thoughts. It may help you become aware of which issues truly need your attention and which ones are less important. It may also help you become more in tune with your body.
You can practice mindful meditation in silence, outdoors with the sounds of nature, or with music playing in the background (typically a soothing instrumental track). While studies generally show that 10 to 15 minutes a day are beneficial, even 5 minutes will probably help you tremendously with stress management and your overall mood. You can either block off a time of day for meditation or do it as you feel the need throughout the day (or both).
Mindful meditation has even been evaluated as an adjunct therapy for a variety of chronic illnesses, including some autoimmune conditions. For example, clinical trials evaluating mindful practices in patients with cancer, fibromyalgia, chronic pain, rheumatoid arthritis, type 2 diabetes, chronic fatigue syndrome, multiple chemical sensitivity, and cardiovascular disease all showed benefits (albeit sometimes modest benefits). Meditative exercises have also been shown to decrease oxidative stress and increase levels of two important antioxidants, glutathione and superoxide. One of the best things about this stress management technique is that nearly everyone can do it.
There are a wealth of guided meditations and meditation courses that can help you ease into mindfulness practice. Apps such as Insight Timer, Headspace, and Calm are all excellent resources to get started. Another great option is Heartmath Inner Balance, which guides you to breathe in sync with your heartbeat, a meditative state called coherence.
Citations
Barbadoro, P., et al., Fish oil supplementation reduces cortisol basal levels and perceived stress: a randomized, placebo-controlled trial in abstinent alcoholics, Mol Nutr Food Res. 2013;57(6):1110-4
Bassett SM et al. Sleep quality but not sleep quantity effects on cortisol responses to acute psychosocial stress. Stress. 2015;18(6):638-44
Broussard JL, et al. “Sleep restriction increases free fatty acids in healthy men.” Diabetologia. 2015 Apr; 58(4): 791–798.
Cohen, S et a., Psychological Stress and Disease, JAMA. 2007;298(14):1685-1687. doi:10.1001/jama.298.14.1685.
Cohen, S., et al., Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk, Proc Natl Acad Sci U S A. 2012;109(16):5995-9
Dhabhar, F. S. and McEwen, B. S., Acute stress enhances while chronic stress suppresses immune function in vivo: a potential role for leukocyte trafficking, Brain Behav Immun. 1997;11:286-306
Dimsdale, J.E. Psychological Stress and Cardiovascular Disease, J Am Coll Cardiol. 2008;51(13):1237-1246. doi:10.1016/j.jacc.2007.12.024
Giebels V, Repping-wuts H, Bleijenberg G, Kroese JM, Stikkelbroeck N, Hermus A. Severe fatigue in patients with adrenal insufficiency: physical, psychosocial and endocrine determinants. J Endocrinol Invest. 2014;37(3):293-301.
Glaser, R., et al., Evidence for a shift in the Th1 to Th2 cytokine response associated with chronic stress and aging, J Gerontol A Biol Sci Med Sci. 2001;56:M477-M482
Guyton AC, Hall JE. Textbook of Medical Physiology. Philadelphia, US; Saunders Medical; 2000.
Head KA, Kelly GS. Nutrients and botanicals for treatment of stress: adrenal fatigue, neurotransmitter imbalance, anxiety, and restless sleep. Altern Med Rev. 2009;14(2):114-40.
Jefferies, W. M., Cortisol and immunity, Med Hypotheses. 1991;34(3):198-208
Kumar V, Abbas AK, Aster JC. Robbins Basic Pathology. Elsevier Health Sciences; 2012.
Lane JD et al. “Caffeine affects cardiovascular and neuroendocrine activation at work and home”. Psychosom Med. 2002 Jul-Aug;64(4):595-603.
Lane, J.D et. Al. “Caffeine effects on cardiovascular and neuroendocrine responses to acute psychosocial stress and their relationship to level of habitual caffeine consumption. Psychosomatic Medicine”. 1990. 52(3):320-36.
Lovallo WR et al. “Stress-like adrenocorticotropin responses to caffeine in young healthy men” Pharmacol Biochem Behav 1996;55:365–9.
Lovallo, W. et. a. “Caffeine Stimulation of Cortisol Secretion Across the Waking Hours in Relation to Caffeine Intake Levels”. Psychosomatic Medicine. 2005. 67:734-739
Melamed, S., et al., Burnout and risk of cardiovascular disease: Evidence, possible causal paths, and promising research directions Psychological Bulletin, Vol 132(3), May 2006, 327-353.
Owen, et al. “Too Much Sitting: The Population-Health Science of Sedentary Behavior.” Exerc Sport Sci Rev. 2010 Jul; 38(3): 105–113.
Panter-Brick. “Sexual division of labor: energetic and evolutionary scenarios.” Am J Hum Biol. 2002 Sep-Oct;14(5):627-40.
Peet A. Marks’ Basic Medical Biochemistry. Lippincott Williams & Wilkins; 2012.
Tanriverdi F, Karaca Z, Unluhizarci K, Kelestimur F. The hypothalamo-pituitary-adrenal axis in chronic fatigue syndrome and fibromyalgia syndrome. Stress. 2007;10(1):13-25.
Wu, G. coffee, et al., Understanding resilience, Front Behav Neurosci. 2013;7:10
Zampelas A et al. “Associations between coffee consumption and inflammatory markers in healthy persons: the ATTICA study”. Am J Clin Nutr. 2004 Oct;80(4):862-7.