Infertility is clinically defined as the inability for a couple to conceive, with the pregnancy resulting in a live birth, after having unprotected intercourse for 12 months. And, it’s more common than many people realize. Approximately 10 to 15 percent of women aged 15 to 44 in the USA have difficulty getting or staying pregnant. And one of the chief drivers of this may be thyroid disorders, including autoimmune thyroid diseases (Hashimoto’s thyroiditis and Grave’s disease), non-autoimmune hypothyroidism, and subclinical hypothyroidism.
Infertility is clinically defined as the inability for a couple to conceive, with the pregnancy resulting in a live birth, after having unprotected intercourse for 12 months. And, it’s more common than many people realize. Approximately 10 to 15 percent of women aged 15 to 44 in the USA have difficulty getting or staying pregnant. And one of the chief drivers of this may be thyroid disorders, including autoimmune thyroid diseases (Hashimoto’s thyroiditis and Grave’s disease), non-autoimmune hypothyroidism, and subclinical hypothyroidism.
The thyroid gland produces hormones that control metabolism as well as influence other essential systems in the human body, such as the cardiovascular system, the immune system, and calcium homeostasis. Thyroid hormones increase our basal metabolic rate, control appetite, improve absorption of nutrients from the digestive tract, and control gut motility. They play an essential role in glucose metabolism and also stimulate the breakdown of fats.
Most relevant to this article, thyroid hormones directly impact the reproductive system in both women and men, influencing levels of sex hormone binding globulin (a glycoprotein that binds with testosterone and estrogen in the blood and renders them inactive), steroid sex hormones (most notably estrogen and testosterone), and gonadotropins (hormones produced by the pituitary gland that regulate gonad [ovary and testes] function, most notably luteinizing hormone). When the levels of these hormones are abnormal, whether it’s absolute levels, relative levels, or temporal regulation, conception can be inhibited.
In men, both hypo- and hyperthyroidism can cause changes to sperm motility and morphology as well as erectile dysfunction. In women, both hypothyroidism and hyperthyroidism can cause irregular menstrual cycles, and interfere with ovulation and embryo implantation. In fact, a 2014 study calculated that a whopping 52.3 percent of women suffering Grave’s disease and 47.0 percent of women suffering Hashimoto’s thyroiditis experienced infertility. These types of alarming statistics has led to more regular screening for thyroid function by fertility experts.
The impact of thyroid hormones goes beyond conception however.
Thyroid Disorders and Adverse Pregnancy Outcomes
 Thyroid disorders increase risk of adverse pregnancy outcomes (like miscarriage) because maternal thyroid hormones are essential for the formation of the fetal nervous system. While maternal thyroid hormones don’t cross the placental barrier easily, what does is an essential developmental regulator, especially in the first 11 weeks before the fetus’ thyroid (which is the first endocrine gland to develop in the fetus) can start producing some thyroid hormones. After the 11-week mark, fetal thyroid hormones take over driving development—including central nervous system, lung, and bones— for the remainder of gestation and into infancy.
Thyroid disorders increase risk of adverse pregnancy outcomes (like miscarriage) because maternal thyroid hormones are essential for the formation of the fetal nervous system. While maternal thyroid hormones don’t cross the placental barrier easily, what does is an essential developmental regulator, especially in the first 11 weeks before the fetus’ thyroid (which is the first endocrine gland to develop in the fetus) can start producing some thyroid hormones. After the 11-week mark, fetal thyroid hormones take over driving development—including central nervous system, lung, and bones— for the remainder of gestation and into infancy.
Hypothyroidism (whether caused by Hashimoto’s thyroiditis, radiofrequency or radioiodine ablation of the thyroid as a treatment for Grave’s disease, or other causes) during pregnancy increases the risks of low-birth weight by 15%, preterm birth by 34%, gravidic hypertension by 8%, preeclampsia by 47%, gestational diabetes by 57%, placental abruption by 4%, cesarean section after spontaneous labor by 38%, post-partum hemorrhage by 8%, post-partum thyroiditis by 19% and more than doubles risk of ICU admission.
Hyperthyroidism (typically caused by Grave’s disease) during pregnancy increases the risk of preeclampsia by 78%, preterm birth by 81%, and more than triples risk of ICU admission.
Close monitoring and thyroid hormone replacement lowers risk of all of these complications. This is why the standard of care for pregnant mothers with hypothyroidism is frequent testing and adjustment of exogenous thyroid hormone dose.
However, even when thyroid disorders are managed via thyroid hormone replacement, thyroidectomy or thyroid radioablation, or in the case of subclinical hypothyroidism, infertility problems and adverse pregnancy outcomes can persist.
Save 70% Off the AIP Lecture Series!
Learn everything you need to know about the Autoimmune Protocol to regain your health!
I am loving this AIP course and all the information I am receiving. The amount of work you have put into this is amazing and greatly, GREATLY, appreciated. Thank you so much. Taking this course gives me the knowledge I need to understand why my body is doing what it is doing and reinforces my determination to continue along this dietary path to heal it. Invaluable!
Carmen Maier
Thyroid Antibodies, Fertility and Pregnancy Outcomes
 When thyroid hormone levels are well-managed or normal thyroid function is maintained (this is called euthyroidism), elevated thyroid antibodies are still linked with miscarriage and complications during pregnancy.
When thyroid hormone levels are well-managed or normal thyroid function is maintained (this is called euthyroidism), elevated thyroid antibodies are still linked with miscarriage and complications during pregnancy.
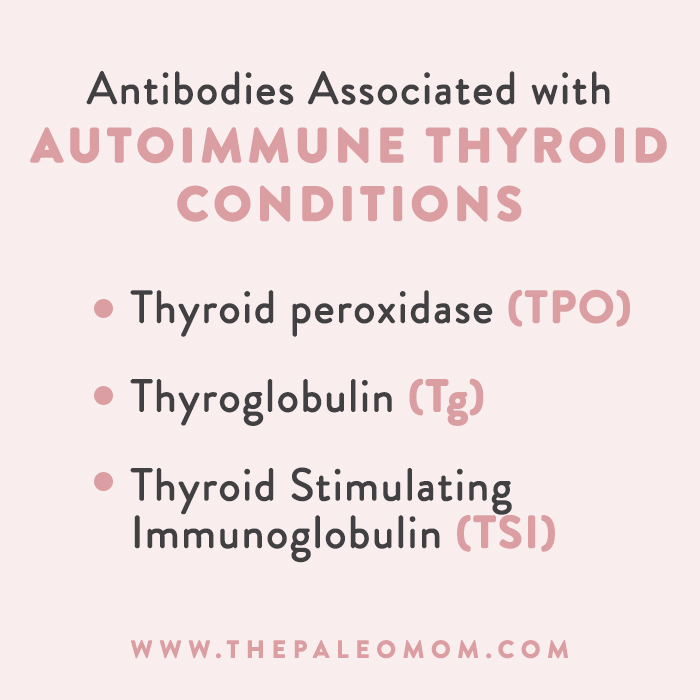
There are three different antibodies associated with autoimmune thyroid conditions.
Thyroid peroxidase (TPO; also called iodide peroxidase) is an enzyme important for thyroid hormone formation. Specifically, TPO catalyzes the production of thyroid hormones through “organification” of iodine, i.e., the conversion of iodide ions into iodine atoms (via oxidation) so they can be complexed with an amino acid (tyrosine) and then incorporated into thyroxine (T4), the thyroid prohormone. TPO antibodies are the most common test for autoimmune thyroid diseases because they can be detected in both Hashimoto’s thyroiditis and Grave’s disease. Most people with Hashimoto’s thyroiditis produce TPO antibodies, although not all.
Thyroglobulin (Tg) acts as a substrate for the synthesis of thyroid hormones as well as the storage of the inactive forms of thyroid hormone and iodine. The presence of thyroglobulin antibodies in a hypothyroid individual is diagnostic for Hashimoto’s thyroiditis, although the production of Tg antibodies is less common that TPO antibodies.
In Grave’s disease, an autoantibody called thyroid stimulating immunoglobulin (TSI) is produced. TSI binds to receptors for thyroid stimulating hormone (TSH), a hormone produced by the pituitary gland that regulates T4 production by the thyroid gland. TSI mimics that action of TSH, which causes excess production of T4 and triiodothyronine (T3), the active form of thyroid hormone. [As an aside, T4 is converted into T3 by a group of selenium-containing enzymes called deiodinases (aka 5′-iodinase) that are found in multiple areas of the body. Type 1 deiodinase (D1) is present in the thyroid, liver and kidney. Type 2 deiodinase (D2) is present in the thyroid, central nervous system, pituitary (making its activity the most important for negative feedback on thyroid-stimulating hormone), pineal gland, brown adipose tissue (important in cold adaptation), placenta, skeletal muscle, and heart. Type 3 deiodinase (D3) is found in the placenta and central nervous system. ]
The impact of thyroid autoantibodies on pregnancy outcomes in euthyroid women has best been studied in the context of Hashimoto’s thyroiditis, i.e., antibodies against TPO and Tg. And, here’s where subclinical hypothyroidism comes in too. Approximately 10% to 15% of the general population are positive for either thyroid peroxidase (TPO) or thyroglobulin (Tg) antibodies. However, only about 10% of those with positive thyroid antibodies have hypothyroidism. It’s quite striking to compare the incidence of thyroid autoantibody production to the incidence of infertility in the USA. While it’s unlikely that there only one major explanation for infertility, given the information below, there’s a very strong case for thyroid autoantibody screening in all women of child-bearing age who are considering becoming pregnant.
Thyroid peroxidase (TPO) Antibodies
Even in euthyroid women, elevated TPO antibodies (anti-TPO) are strongly associated with a higher prevalence of infertility, gestational anemia, miscarriage and preterm delivery.
A pair of recent studies from two different regions of India showed that euthyroid women with elevated TPO antibodies had significantly higher rates of miscarriage (up to 6 times higher), low birth weight (up to 5 times higher) and preterm delivery (up to 4 times higher). An older meta-analysis concluded that anti-TPO positivity (regardless of thyroid function) increased risk of pre-term delivery by 69% in euthyroid women (that particular study did not evaluate other adverse pregnancy outcomes).
How can the presence of TPO antibodies have such a large effect on pregnancy outcomes even in the context of normal thyroid function? Anoter recent study showed that maternal TPO antibodies diffuse across the placental barrier easily and can then interfere with thyroid hormone production in the fetus.
Basically, maternal thyroid antibodies bind with essential thyroid enzymes in the fetus thereby blocking their actions in the production of fetal thyroid hormones. The ensuing shortage of thyroid hormone leads to developmental abnormalities which can result in pregnancy loss or complications.
Because maternal thyroid hormones are critical for very early embryonic development, it’s not surprising that there’s also a link between the presence of TPO antibodies prior to conception and pregnancy outcomes. A 2017 paper showed that the pre-conceptual TPO antibodies increased risk of miscarriage by 2.2 times and decreased probability of live birth by 42%.
Thyroglobulin (Tg) Antibodies
While there’s much more robust evidence linking anti-TPO to adverse pregnancy outcomes, there’s also evidence that Tg antibodies are culprits as well.
Many studies looking at links between thyroid antibodies and risk of miscarriage or pregnancy complications pool both anti-Tg and anti-TPO positive women into the same group (in large part because it is less common for a woman to have antibodies against Tg and not TPO), but there are handful of studies that do evaluate effects of anti-Tg independent of anti-TPO.
In particular, Tg antibodies increase risk of recurrent pregnancy loss (by nearly 3 times) and are strongly linked to unexplained infertility, implantation failure and recurrent spontaneous abortion. Animal models demonstrate that the presence of anti-Tg causes a high rate of fetal resorption and, similar to anti-TPO, confirm that Tg antibodies easily cross the placenta into the fetus.
Improving Fertility through Better Thyroid Disorder Management
The importance of lowering thyroid antibodies is often overlooked by practitioners but may be the missing link for women with hypothyroidism (up to 3% of the population), hyperthyroidism (up to 1% of the population) or subclinical hypothyroidism (up to 15% of the population) who are struggling with fertility problems. In fact, thyroid antibodies are also linked to failed IVF treatments so screening for these autoantibodies prior to investing in IVF seems like a smart idea! There may be additional benefits to lowering thyroid antibodies beyond pregnancy as well: a 2007 study demonstrated that thyroid antibodies are also passed onto the baby during lactation, at least in rodents.
 So, how do you lower thyroid antibodies? Currently, conventional medicine offers no treatment that can lower autoantibodies that is safe for use during pregnancy. That leaves us with functional medicine (which could include medication or supplements to help regulate the immune system; I recommend Dr. Izabella Wentz at ThyroidPharmacist.com as a resource) and the Autoimmune Protocol. There is an ongoing clinical trial evaluating to what degree thyroid antibodies can be lowered with the AIP as the sole intervention, however anecdotal evidence from the AIP community suggests that some people can see their antibodies go to zero on the AIP whereas others just don’t. It’s still unclear to me why some people can see such huge improvements in symptoms and quality of life that aren’t fully reflected on their bloodwork, but I am one of those people. While my Tg antibodies have decreased substantially with the AIP and functional medicine interventions, I’ve never been able to get them to zero. On the flip side, I’ve met eight babies at book signings and conferences with mothers sharing their experiences with me of how the AIP was the magic thing that helped them get (and stay!) pregnant. My co-author on The Healing Kitchen, Alaena Haber of GrazedandEnthused.com is one such success story, now expecting her second baby!
So, how do you lower thyroid antibodies? Currently, conventional medicine offers no treatment that can lower autoantibodies that is safe for use during pregnancy. That leaves us with functional medicine (which could include medication or supplements to help regulate the immune system; I recommend Dr. Izabella Wentz at ThyroidPharmacist.com as a resource) and the Autoimmune Protocol. There is an ongoing clinical trial evaluating to what degree thyroid antibodies can be lowered with the AIP as the sole intervention, however anecdotal evidence from the AIP community suggests that some people can see their antibodies go to zero on the AIP whereas others just don’t. It’s still unclear to me why some people can see such huge improvements in symptoms and quality of life that aren’t fully reflected on their bloodwork, but I am one of those people. While my Tg antibodies have decreased substantially with the AIP and functional medicine interventions, I’ve never been able to get them to zero. On the flip side, I’ve met eight babies at book signings and conferences with mothers sharing their experiences with me of how the AIP was the magic thing that helped them get (and stay!) pregnant. My co-author on The Healing Kitchen, Alaena Haber of GrazedandEnthused.com is one such success story, now expecting her second baby!
Understanding the link between thyroid antibodies and pregnancy outcomes is important for supporting women through fertility challenges, and emphasizes the importance of using the Autoimmune Protocol as part of a holistic approach to address infertility, recurrent pregnancy loss, and pregnancy complications.
 Expanding Options for Families
Expanding Options for Families
Understanding the link between thyroid antibodies and fertility can also provide women with valuable information for family planning, especially for those women for whom the AIP and functional medicine aren’t enough. In fact, it was my good friend (and social media manager!) Kiersten Peterson of Vibrant Life Army Wife whose struggles inspired this post.
I started researching this topic for Kiersten over a year ago, as she struggled with recurrent pregnancy loss. Kiersten was doing everything right, following the AIP, working with a functional medicine practitioner, taking pregnancy-safe supplements to help regulate the immune system. She did get her antibodies down, and had her thyroid levels well managed. And yet, Kiersten tragically suffered four late miscarriages (Ellis Ford, Baby Pea, Little Bean, and Faith). I scoured the medical literature for any clues, any missing links, anything I might have missed that would help. Testing after her fourth miscarriage revealed that Faith was 100% healthy, which meant no genetic diseases… and no explanations.
Kiersten is one of the most inspirational people in my life. Her faith has kept her grounded throughout this experience. Her dedication to motherhood and her perseverance through adversity led her (and her amazing husband) to reach for an alternative: adoption. Some little baby is going to be very, very lucky to be brought into their loving home.
 I want to share Kiersten’s experience, not just because I’ve had a front-row seat, but because I want other people struggling with infertility to know that they’re not alone. In fact, Kiersten has been very open about her experiences on her blog and social media accounts and I encourage you to reach out and connect.
I want to share Kiersten’s experience, not just because I’ve had a front-row seat, but because I want other people struggling with infertility to know that they’re not alone. In fact, Kiersten has been very open about her experiences on her blog and social media accounts and I encourage you to reach out and connect.
Kiersten is fundraising to help fund her adoption (I had no idea they were so expensive! Like $40k-$50k!), selling these beautifully-designed Warrior T-shirts on Bonfire. I hope you’ll consider purchasing a shirt (and tag #TeamPetersonBaby when you share it on social media!) to help support Kiersten. Plus, we’ll match!
Most of all, if you are having similar experiences to Kiersten, I want you to know that it isn’t because you aren’t “AIP-ing hard enough”. This falls under the same mindset banner as understanding that medication is not failure. The Autoimmune Protocol isn’t a substitute for medical intervention, but rather a complementary approach, and we’re allowed to use the best of both worlds (judicious and informed use of conventional medicine combined with optimal diet and lifestyle), especially for those things beyond our control and our ability to mitigate with diet and lifestyle.
Citations
Arbib N, Hadar E, Sneh-Arbib O, Chen R, Wiznitzer A, Gabbay-Benziv R. First trimester thyroid stimulating hormone as an independent risk factor for adverse pregnancy outcome. J Matern Fetal Neonatal Med. 2017 Sep;30(18):2174-2178. doi: 10.1080/14767058.2016.1242123.
Becker MI, De Ioannes AE, León C, Ebensperger LA. Females of the communally breeding rodent, Octodon degus, transfer antibodies to their offspring during pregnancy and lactation. J Reprod Immunol. 2007 Jun;74(1-2):68-77.
Bellver J, Soares SR, Alvarez C, Muñoz E, Ramírez A, Rubio C, Serra V, Remohí J, Pellicer A. The role of thrombophilia and thyroid autoimmunity in unexplained infertility, implantation failure and recurrent spontaneous abortion. Hum Reprod. 2008 Feb;23(2):278-84.
Bernal J. Thyroid hormones and brain development. Vitam Horm. 2005;71:95-122.
Bussen S, Steck T, Dietl J. Increased prevalence of thyroid antibodies in euthyroid women with a history of recurrent in-vitro fertilization failure. Hum Reprod. 2000 Mar;15(3):545-8.
Fröhlich E, Wahl R. Thyroid Autoimmunity: Role of Anti-thyroid Antibodies in Thyroid and Extra-Thyroidal Diseases. Front Immunol. 2017 May 9;8:521. doi: 10.3389/fimmu.2017.00521.
- E. Krassas, K. Poppe, D. Glinoer; Thyroid Function and Human Reproductive Health, Endocrine Reviews, Volume 31, Issue 5, 1 October 2010, Pages 702–755, https://doi.org/10.1210/er.2009-0041
He X, Wang P, Wang Z, He X, Xu D, Wang B. Thyroid antibodies and risk of preterm delivery: a meta-analysis of prospective cohort studies. Eur J Endocrinol. 2012 Oct;167(4):455-64. doi: 10.1530/EJE-12-0379.
King JR, Lachica R, Lee RH, Montoro M, Mestman J. Diagnosis and Management of Hyperthyroidism in Pregnancy: A Review. Obstet Gynecol Surv. 2016 Nov;71(11):675-685. doi: 10.1097/OGX.0000000000000367
Männistö T, Mendola P, Grewal J, Xie Y, Chen Z, Laughon SK. Thyroid diseases and adverse pregnancy outcomes in a contemporary US cohort. J Clin Endocrinol Metab. 2013 Jul;98(7):2725-33. doi: 10.1210/jc.2012-4233.
Matalon ST, Blank M, Levy Y, Carp HJ, Arad A, et al. The pathogenic role of anti-thyroglobulin antibody on pregnancy: evidence from an active immunization model in mice. Hum Reprod. 2003 May;18(5):1094-9.
Meena A, Nagar P. Pregnancy Outcome in Euthyroid Women with Anti-Thyroid Peroxidase Antibodies. J Obstet Gynaecol India. 2016 Jun;66(3):160-5. doi: 10.1007/s13224-014-0657-6.
Meena M, Chopra S, Jain V, Aggarwal N. The Effect of Anti-Thyroid Peroxidase Antibodies on Pregnancy Outcomes in Euthyroid Women. J Clin Diagn Res. 2016 Sep;10(9):QC04-QC07.
Mumusoglu S, Beksac MS, Ekiz A, Ozdemir P, Hascelik G. Does the presence of autoantibodies without autoimmune diseases and hereditary thrombophilia have an effect on recurrent pregnancy loss? J Matern Fetal Neonatal Med. 2016;29(14):2352-7. doi: 10.3109/14767058.2015.1085964.
Poppe K, Velkeniers B. Thyroid and infertility. Verh K Acad Geneeskd Belg. 2002;64(6):389-99; discussion 400-2.
Quintino-Moro A, Zantut-Wittmann DE, Tambascia M, Machado Hda C, Fernandes A. High Prevalence of Infertility among Women with Graves’ Disease and Hashimoto’s Thyroiditis. Int J Endocrinol. 2014;2014:982705. doi: 10.1155/2014/982705. Epub 2014 Feb 11.
Rajput R, Yadav T, Seth S, Nanda S. Prevalence of Thyroid Peroxidase Antibody and Pregnancy Outcome in Euthyroid Autoimmune Positive Pregnant Women from a Tertiary Care Center in Haryana. Indian J Endocrinol Metab. 2017 Jul-Aug;21(4):577-580. doi: 10.4103/ijem.IJEM_397_16.
Seror J, Amand G, Guibourdenche J, Ceccaldi PF, Luton D. Anti-TPO antibodies diffusion through the placental barrier during pregnancy. PLoS One. 2014 Jan 31;9(1):e84647. doi: 10.1371/journal.pone.0084647.
Seungdamrong A, Steiner AZ, Gracia CR, Legro RS, Diamond MP, et al. Preconceptional antithyroid peroxidase antibodies, but not thyroid-stimulating hormone, are associated with decreased live birth rates in infertile women. Fertil Steril. 2017 Oct 25. pii: S0015-0282(17)31748-X. doi: 10.1016/j.fertnstert.2017.08.026.
Trokoudes KM, Skordis N, Picolos MK. Infertility and thyroid disorders. Curr Opin Obstet Gynecol. 2006 Aug;18(4):446-51.
Velázquez EM, Bellabarba Arata G. Effects of thyroid status on pituitary gonadotropin and testicular reserve in men. Arch Androl. 1997 Jan-Feb;38(1):85-92.
Yamamoto J, Donovan LE. Managing thyroid disease in women planning pregnancy. CMAJ. 2017 Jul 17; 189(28):E940.