Chronic kidney disease is a condition in which there is gradual and progressive loss of kidney function. It affects about 10% of the American population, with older people at much greater risk—for example, prevalence is only about 4% for people in their 30s compared to 47% for people over 70. The two main causes of chronic kidney disease are diabetes (see The Paleo Diet for Diabetes) and high blood pressure (see The Paleo Diet for Cardiovascular Disease), which are responsible for up to two-thirds of the cases. Choices that mitigate diabetes and normalize blood pressure will also help reduce risk of chronic kidney disease.
 What do the Kidneys Do?
What do the Kidneys Do?
Along with the liver, the kidneys play a vital role in removing toxins from the body. They’re constantly at work filtering blood (about 150 quarts every day!), regulating the body’s sodium and potassium balance, producing hormones, regulating blood pressure, controlling calcium metabolism, controlling red blood cell production, removing waste products and drugs from the body, and producing an active form of vitamin D.
Our two bean-shaped kidneys, each about the size of a fist, contain up to a million nephrons, which are functional units consisting of a glomerulus and a tubule. The glomerulus filters waste products out of the blood, and the remaining fluid passes through the tubule, where chemicals and water are either removed or added (the tubules also shuttle minerals back to the bloodstream as needed). The end product is urine, which flows from the kidneys to the bladder through ureters (two thin tubes of muscle) until we’re ready to excrete it.
For the kidneys to do their job, the body needs a sufficient volume of water to carry away waste products. Therefore, staying fully hydrated is paramount. Few substances are more “Paleo” than water itself, and it should come as no surprise that drinking enough of it is key for optimal health!
Hydration for Kidney Health
 How much water do we need? The classic recommendation of eight 8-ounce glasses (64 ounces total) per day is mostly a misconception. The latest research suggests that men should consume about 13 cups (, or 3 liters) of fluid per day, and women should consume about 9 cups (74 ounce, or 2.2 liters)—but this includes all beverages, as well as the water content of the food we eat. We get up to 20 percent of our daily water from food, particularly fruits, vegetables, and soups! In addition to supporting kidney health, staying hydrated helps optimize digestion, neurological function, circulation, body temperature regulation, and muscle contraction.
How much water do we need? The classic recommendation of eight 8-ounce glasses (64 ounces total) per day is mostly a misconception. The latest research suggests that men should consume about 13 cups (, or 3 liters) of fluid per day, and women should consume about 9 cups (74 ounce, or 2.2 liters)—but this includes all beverages, as well as the water content of the food we eat. We get up to 20 percent of our daily water from food, particularly fruits, vegetables, and soups! In addition to supporting kidney health, staying hydrated helps optimize digestion, neurological function, circulation, body temperature regulation, and muscle contraction.
The quality of the water we consume is also important. Although most tap water and bottled water has a low mineral content, there’s ample evidence that early humans consumed water containing non-trivial levels of sodium and high levels of other minerals. Most natural sources of water are slightly acidic, so minerals dissolve into the water from soil, sand and rocks that form stream and river beds, etc. Natural freshwater sources (lakes, rivers, streams, and so on) contain some salt, and some have as much as 0.4 percent—which is quite a lot, especially knowing that the ocean is only about 9 times higher at 3.5 percent salt! And, the electrolyte content of natural freshwater can be very impressive. While it varies from source to source, it’s relatively common to get about 20mg/L calcium, 12mg/L magnesium, and 1mg/L potassium in river and stream water. Groundwater can give 3 to 10 times more!
Adding mineral drops to water before drinking it is one way to recreate its natural mineral content. (Read more about the effect of sodium on kidney health in Is Salt Paleo?.) I use both ConcenTrace Trace Mineral Drops and Watermins EM Drops in my filtered water.
(A note on alkaline water [aka ionized water]: Alkaline means that a substance has a pH higher than 7.0 (neutral pH). Commercial alkaline water typically has a pH of 8.8 or higher with high dissolved mineral content, typically calcium, potassium, and magnesium. In contrast, natural water sources typically have a pH between 5.5 (fairly acidic) to 7.7 (weekly alkaline). Typically, the higher the salinity of the natural water, the higher the pH: seawater has a pH of 8.0. Alkaline water is known to neutralize stomach acid, which on the surface may sound like an awesome thing for anyone who suffers from acid reflux. However, because the acidity of chyme (the mixture of food and gastric juices as they leave the stomach and enter the first segment of the small intestine, the duodenum) is a key signal to the pancreas to secrete digestive enzymes and to the gall bladder to secrete bile, neutralizing stomach acid can hinder digestion in a big way! This can lead to bacterial overgrowth (see Modifying Paleo for Small Intestinal Bacterial Overgrowth (SIBO) ) and in fact, studies also confirm that drinking alkaline water causes a major shift in the gut microbiome. And while more research on this in definitely warranted, one study in mice showed that drinking alkaline water for 4 weeks caused a huge decrease in probiotic Clostridium species with smaller decreases in Bifidobacterium and Lactobacillus, and a rise in Prevotella (see The Link Between Meat and Cancer). The studies that do show some benefit to alkaline water do not determine if the benefits are attributable to the actual alkalinity of the water, or the fact that commercial alkaline water has a fairly high concentration of dissolved minerals. Given what we know about The Importance of Nutrient Density, and the fact that our gut bacteria prefer an acidic environment, and the fact that neutralizing stomach acid can hinder digestion, I conclude that it’s much better to consume a mineral-enriched water with a pH closer to neutral.)
Veggies for Chronic Kidney Disease
 High fiber diets, high vegetable and fruit consumption, a daily serving of nuts, and proper hydration have all been shown to decrease risk of kidney disease (see The Importance of Vegetables). As discussed in detail in Is Salt Paleo?, avoiding excess sodium consumption is also important for kidney health. Vitamin D deficiency increases risk of chronic kidney disease as well as all-cause mortality in chronic kidney disease sufferers (see Vitamin D).
High fiber diets, high vegetable and fruit consumption, a daily serving of nuts, and proper hydration have all been shown to decrease risk of kidney disease (see The Importance of Vegetables). As discussed in detail in Is Salt Paleo?, avoiding excess sodium consumption is also important for kidney health. Vitamin D deficiency increases risk of chronic kidney disease as well as all-cause mortality in chronic kidney disease sufferers (see Vitamin D).
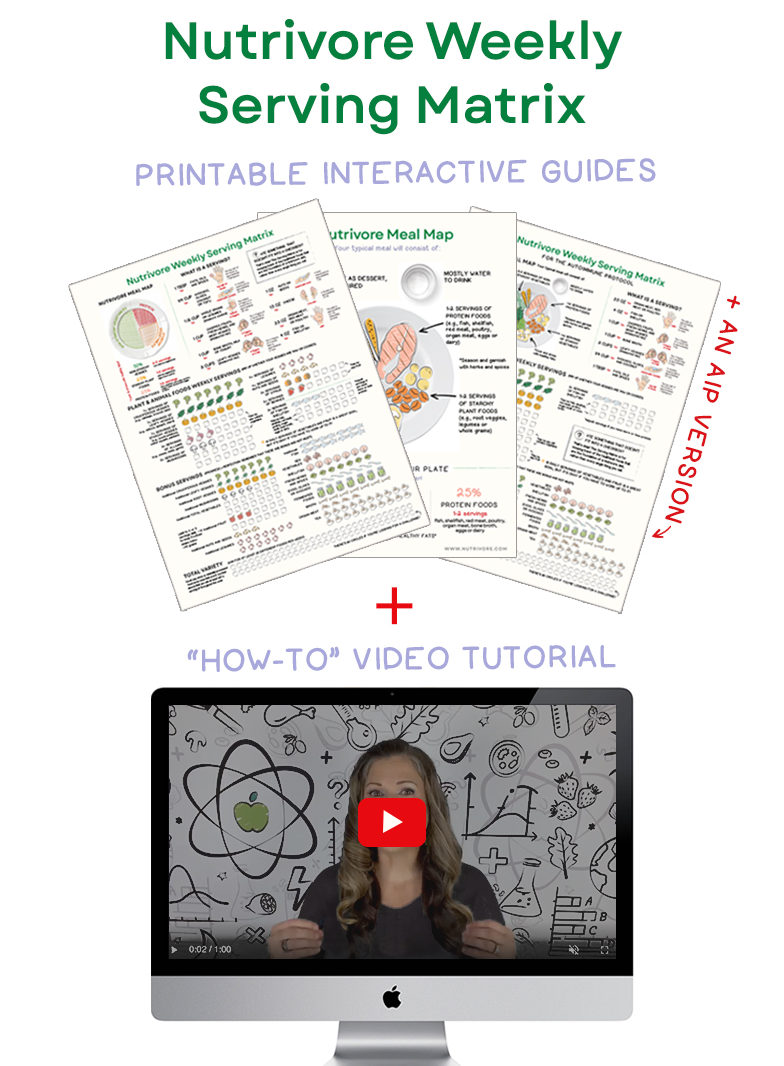
Nutrivore Weekly Serving Matrix
An easy-to-use and flexible weekly checklist
to help you maximize nutrient-density.
The Weekly Serving Matrix is very helpful! I’ve been eating along these lines but this really helps me know where to focus vs. which foods serve a more secondary role. It’s super helpful and has taken a lot of worry out of my meal planning. Thanks!
Jan
A veggie-rich diet may also help treat chronic kidney disease once diagnosed. Recent studies showed that simply adding more fresh vegetables and fruits to the diets of people with chronic kidney disease caused by hypertension could not only protect the kidneys from further deterioration but even improve kidney function. The less advanced the disease, the better the results. Fish oil supplementation has been shown to reduce markers of inflammation and cardiovascular disease risk factors in patients with chronic kidney disease—this is important because cardiovascular disease is the principle cause of death in chronic kidney disease sufferers.
Chronic kidney disease can also cause gout, which is discussed in The Paleo Diet for Gout.
 Kidney stones
Kidney stones
Kidney stones are another potential cause of chronic kidney disease, especially if recurrent. They can impact any part of the urinary tract, from kidneys to bladder. There are several types of kidney stones, the three most common of which are:
- Calcium oxalate stones are the most common type accounting for about 80 percent of all kidney stones. While oxalate is naturally-occurring in some vegetables, there doesn’t seem to be a direct relationship between the oxalate you eat and the formation of calcium oxalate stones (see Is Oxalate Sensitivity Real?)—oxalate is also produced by the liver. High dietary sodium, calcium deficiency, excessive calcium intake via supplementation (but not diet), high fructose intake, and insufficient fluid intake increase risk of calcium oxalate stones.
- Struvite stones account for 10 to 15 percent of all kidney stones and form in response to an infection, such as a urinary tract infection. While not directly linked to diet, people with gout as well as those with underlying metabolic disorders (like hyperparathyroidism) are at greater risk.
- Uric acid stones account for 5 to 10 percent of all kidney stones and form in people who don’t drink enough fluids or get dehydrated; those who eat a high-meat and low-veggie diet; those who consume too much fructose; and those who have gout. Certain genetic factors also may increase your risk of uric acid stones.
High vegetable and fruit consumption is the most important dietary factor to prevent kidney stones (except for stones related to infection or hereditary disorders). Maintaining a healthy weight also lowers kidney stone risk.
As an aside, gallstones are different in composition than kidney stones. While calcium is a common constituent of gallstones, they are composed of predominantly of cholesterol or of bilirubin (a product of heme breakdown that is normally excreted in the bile). Constipation, nutritional deficiency (especially vitamin B9, vitamin C, calcium and magnesium), insufficient fluid intake, high fructose intake, low fiber intake, consumption of fast food, and hypercaloric, high-carbohydrate diets all increase risk of gallstones. Consumption of plenty of vegetables and fruit, high-fiber intake, high intake of monounsaturated fats and omega-3 fatty acids, and vitamin C supplementation reduce risk of gallstones. See also The Link Between Gallbladder Disease and Gluten Sensitivity
Paleo for Kidney Disease
As discussed in The Diet We’re Meant to Eat, Part 3: How Much Meat versus Veggies?, the Paleo diet is truly a plant-based diet with two-thirds to three-quarters of every plate covered in fresh vegetables, fruit, nuts and seeds. Simply following this guideline will reduce risk of kidney stones (again, except for those caused by infection or hereditary disorders) and chronic kidney disease, also thanks to high-veggie consumption also reducing risk factors for chronic conditions that cause kidney disease (see The Importance of Vegetables).
Looking for more resources on eating veggies? Get food lists at Paleo Diet Foods.
Citations
Uribarri J, Oh MS. The key to halting progression of CKD might be in the produce market, not in the pharmacy. Kidney Int. 2012 Jan;81(1):7-9. doi: 10.1038/ki.2011.331.
Goraya N, Simoni J, Jo C, Wesson DE. Dietary acid reduction with fruits and vegetables or bicarbonate attenuates kidney injury in patients with a moderately reduced glomerular filtration rate due to hypertensive nephropathy. Kidney Int. 2012 Jan;81(1):86-93. doi: 10.1038/ki.2011.313. Epub 2011 Aug 31.
Goraya N, Simoni J, Jo CH, Wesson DE. A comparison of treating metabolic acidosis in CKD stage 4 hypertensive kidney disease with fruits and vegetables or sodium bicarbonate. Clin J Am Soc Nephrol. 2013 Mar;8(3):371-81. doi: 10.2215/CJN.02430312. Epub 2013 Feb 7.
Deike E, Bowden RG, Moreillon JJ, Griggs JO, Wilson RL, Cooke M, Shelmadine BD, Beaujean AA. The effects of fish oil supplementation on markers of inflammation in chronic kidney disease patients. J Ren Nutr. 2012 Nov;22(6):572-7. doi: 10.1053/j.jrn.2011.10.036. Epub 2012 Jan 27.
Guebre-Egziabher F, Debard C, Drai J, Denis L, Pesenti S, Bienvenu J, Vidal H, Laville M, Fouque D Differential dose effect of fish oil on inflammation and adipose tissue gene expression in chronic kidney disease patients. Nutrition. 2013 May;29(5):730-6. doi: 10.1016/j.nut.2012.10.011. Epub 2013 Jan 30.
Jayedi A, Soltani S, Shab-Bidar S. Vitamin D status and all-cause mortality in patients with chronic kidney disease: A systematic review and dose-response meta-analysis. J Clin Endocrinol Metab. 2017 Apr 27. doi: 10.1210/jc.2017-00105.
Frassetto L, Kohlstadt I. Treatment and prevention of kidney stones: an update. Am Fam Physician. 2011 Dec 1;84(11):1234-42.
Heilberg IP, Goldfarb DS. Optimum nutrition for kidney stone disease. Adv Chronic Kidney Dis. 2013 Mar;20(2):165-74. doi: 10.1053/j.ackd.2012.12.001.
Taylor EN, Curhan GC. Fructose consumption and the risk of kidney stones. Kidney Int. 2008 Jan;73(2):207-12. Epub 2007 Oct 10.
Tracy CR, Best S, Bagrodia A, Poindexter JR, Adams-Huet B, Sakhaee K, Maalouf N, Pak CY, Pearle MS. Animal protein and the risk of kidney stones: a comparative metabolic study of animal protein sources. J Urol. 2014 Jul;192(1):137-41. doi: 10.1016/j.juro.2014.01.093. Epub 2014 Feb 8.
Di Ciaula A, Garruti G, Frühbeck G, De Angelis M, De Bari O, Q-H Wang D, Lammert F, Portincasa P. The Role Of Diet In The Pathogenesis Of Cholesterol Gallstones. Curr Med Chem. 2017 May 29. doi: 10.2174/0929867324666170530080636.
Ortega RM, Fernández-Azuela M, Encinas-Sotillos A, Andrés P, López-Sobaler AM (1997). “Differences in diet and food habits between patients with gallstones and controls”. Journal of the American College of Nutrition. 16 (1): 88–95. PMID 9013440. doi:10.1080/07315724.1997.10718655. Archived from the original on 2008-07-20. Retrieved 2010-11-06.
http://www.waterencyclopedia.com/En-Ge/Fresh-Water-Natural-Composition-of.html
Kulthanan K, et al. The pH of water from various sources: an overview for recommendation for patients with atopic dermatitis. Asia Pac Allergy. 2013 Jul;3(3):155-60. doi: 10.5415/apallergy.2013.3.3.155. Epub 2013 Jul 30.
Higashimura Y, et al. Effects of molecular hydrogen-dissolved alkaline electrolyzed water on intestinal environment in mice. Med Gas Res. 2018 Apr 18;8(1):6-11. doi: 10.4103/2045-9912.229597. eCollection 2018 Jan-Mar.
Koufman JA, Johnston N. Potential benefits of pH 8.8 alkaline drinking water as an adjunct in the treatment of reflux disease. Ann Otol Rhinol Laryngol. 2012 Jul;121(7):431-4.



 TPV Podcast, Episode 305: Why Insulin Is Important & Awesome!
TPV Podcast, Episode 305: Why Insulin Is Important & Awesome!