I get a lot of questions from people who are tackling the autoimmune protocol and are frustrated that they aren’t seeing results. When we examine diet and lifestyle factors to narrow in on the missing piece, one of the most common culprits is what I now think of as “veggiephobia”.
People think “well, I can’t eat legumes or nightshades on the AIP and I can’t have FODMAPS because I have IBS, and I have to do GAPS too for SIBO, and I guess since I have GI symptoms, I should also not eat leafy greens because of the insoluble fiber, and then I can’t have the goitrogenic veggies because of my thryoid, and my friend says I should cut out high histamine foods, and four vegetables came up on my ALCAT testing and…” there’s nothing “safe” left so people eat almost no vegetables. This causes deficiencies which slow healing.
You might have noticed that some of the above examples are areas I have specifically researched in order to show you that there is no rationale for avoiding these foods for most people. I have written very thorough posts addressing these topics:
- Avoiding insoluble fiber for GI symptoms/conditions is a myth (I busted a lot of fiber myths in my Fiber Manifesto series, see here, here, here, here, and especially here).
- Avoiding goitrogenic veggies for thyroid diseases is a myth (see here)
One thing I haven’t talked about is avoiding starchy vegetables for SIBO a la GAPS and SCD diets. It turns out that, as popular as these diets are, these approaches have not been validated in the scientific literature. Because of this, I have completely pulled away from my previous recommendations to combine GAPS- and SCD-style avoidance of starchy vegetables for gut dysbiosis. I think annecdotal evidence supports that these approaches can still be very beneficial over the short term (think 2-4 weeks) to quickly correct overgrowths (specifically overgrowths, but not other forms of dysbiosis); but that over longer timescales than that, the low starch and fiber content of these diets doesn’t support the growth of normal gut microorganisms… you basically trade overgrowth for undergrowth (which also has a variety of negative effects for gut and immune health). I won’t go so far as to say that these approaches are myths (because they have worked for many people, at least in the short term), but I think there are better, more well-researched approaches to try first.
The strategy that has been very well studied and clinically validated for dealing with SIBO and other GI complaints (like IBS) is removing or dramatically reducing FODMAPs from the diet. I definitely think that a low-FODMAP diet can be a useful approach in tandem with the autoimmune protocol. This post gives you more details (and of course, there is even more information coming in my book).
But often, health doesn’t come from what you take away, but rather what you add.
My first focus in The Paleo Approach is on adding nutrient-dense foods, especially organ meat, seafood, and large portions of vegetables. Many, many vitamins and minerals are required for the immune system to function normally (so deficiencies lead to immune dysfunction). You need the building blocks of your tissues in order to heal damage to your gut or other organs (so deficiencies slow healing). A huge variety of nutritional deficiencies increase risk of autoimmune disease and chronic illness in general, and it’s pretty easy to understand why: if you don’t have all the nutrients your body needs to be healthy, you won’t be healthy.
With regards to gut dysbiosis, the two diet factors with the most powerful corrective influences on gut microorganisms are high intake of long-chain omega-3 fatty acids (that’s DHA and EPA, which you mainly get from seafood but also from grass-fed meat) and insoluble fiber from vegetables. (Okay, two other diet factors are hugely important too and those are eliminating gluten and eliminating alcohol… but I assume you’re doing those on the autoimmune protocol.) If you are severely restricting your vegetable intake, you are hindering your gut microbiome from normalizing in diversity, numbers and location–i.e., you are slowing down your healing process. Also recall that my research into soluble versus insoluble fiber showed that the insoluble fiber from vegetables is more antiinflammatory than soluble and can actually help speed the healing of your gut (see here and here). Plus correcting your gut bacteria is one of the most important aspects of properly regulating the immune system–eating lots of fish and vegetables is the most expedient way to do that.
The other thing you are missing if you don’t eat enough vegetables is the tremendous diversity of vitamins, minerals and antioxidant phytochemicals within them. Research shows that chlorophyll (the green pigment in vegetables) completely inhibits the production of potentially cancer-causing byproducts from the digestion and metabolism of heme (an iron-containing molecule that is particularly rich in red meat). This is why all research showing that red meat causes cancer has the correlation completely disappear once you include vegetable intake in the calculations: it’s not high meat consumption that increases your risk of cancer, it’s low vegetable consumption. In addition, a variety of vitamins, minerals and antioxidants abundantly found in vegetables are required by the immune system for it to function normally–if you are deficient in these micronutrients, your immune system will stay in overdrive.
Vegetables are nutrient-dense foods that should be a large part of your diet.
Dr. Terry Wahls‘ original protocol for reversing multiple sclerosis with diet focused on eating 9 cups of vegetables per day; and, as defined in her initial clinical trials, this was far more important than cutting anything out. The newest version of her protocol being used in her current clinical trials and which Dr. Wahls explained beautifully in her upcoming book The Wahls Protocol (I had the pleasure of previewing this book and I highly recommend it!) includes 9 cups of vegetables plus a focus on nutrient-dense protein sources like seafood and organ meat (anecdotally, these are the other two most commonly omitted foods in the diets of people who are not seeing results on the autoimmune protocol).
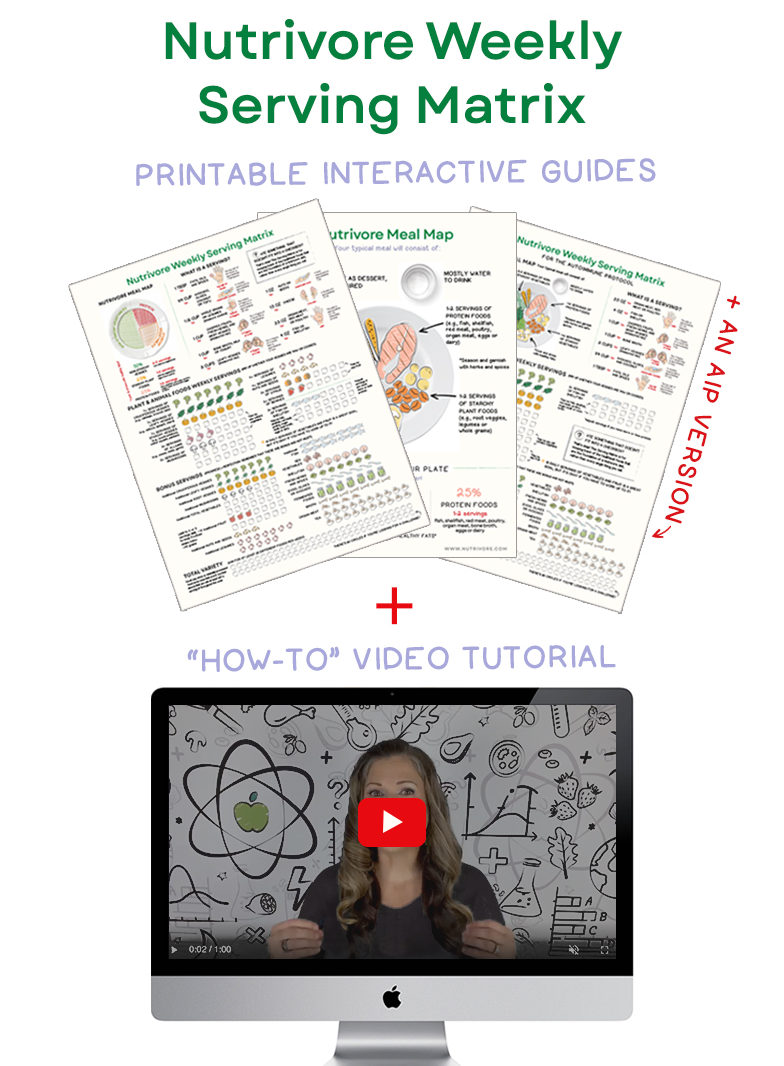
Nutrivore Weekly Serving Matrix
An easy-to-use and flexible weekly checklist
to help you maximize nutrient-density.
The Weekly Serving Matrix is very helpful! I’ve been eating along these lines but this really helps me know where to focus vs. which foods serve a more secondary role. It’s super helpful and has taken a lot of worry out of my meal planning. Thanks!
Jan
Overlimiting vegetables, especially if you are also limiting your fruit intake can lead to a very low carbohydrate diet. Let’s just follow this tangent for a minute, because fruitphobia is related to veggiephobia. Recall that one aspect of the autoimmune protocol is to keep fructose intake between 10g and 20g per day. Many people try to err on the safe side, which means they avoid fruit completely, but some fructose actually has health benefits. Not to mention that fruit are also rich in vitamins, minerals, antioxidants, and fiber. To stay between 10g and 20g, you can eat 2-5 servings of fruit per day depending on which fruit you choose. Another reason people tend to avoid fruit is concern that the sugars in fruit will cause problems, but really, as long as your blood sugar levels are well regulated (which they will be if you eat fruit in moderation with meals), fruit shouldn’t be a problem. It’s helpful to familiarize yourself with which fruits are lowest fructose and relatively low sugar (berries, citrus, melons) and which pack a fructose punch (apple family, tropical fruits). Okay, so the low carb thing: eating too low carb can be very hard on your thyroid and on your adrenal glands. Clinical trials in rheumatoid arthritis patients following a ketogenic diet showed worsening of symptoms and increased cortisol (see this post). Some people do great on very low carb diets (and it that’s you, you probably aren’t emailing me to find out why the autoimmune protocol isn’t working for you–if something is working for you, stick with it).
Eating large portions of a wide variety of vegetables is an important aspect of The Paleo Approach and the autoimmune protocol. You may heal faster by increasing your vegetable intake.
There are certainly additional food sensitivities that might be complicating your particular situation, including:
- FODMAP sensitivity (or a subset of FODMAPs like just sugar alcohols or just fructan fibers; see here)
- Histamine sensitivity (see here)
- Salicylate sensitivity (see here)
- Sulfate sensitivity
- Food intolerances or allergies
These are all discussed in the troubleshooting chapter of The Paleo Approach (along with a ton of other topics). But, I think that all of these (unless explicitly diagnosed by a healthcare professional) shouldn’t be assumed, and certainly shouldn’t be where you start. These are for troubleshooting, 3-4 months down the road. And, I would far rather see you try digestive support supplements first (plant enzymes are particularly helpful for digestive issues associated with eating vegetables and fruit, and I recommend either Enriching Gifts or Thorne Research) before you start severely limiting your vegetable variety. (Other digestive support supplements are discussed in great detail in my book but also more generally on my autoimmune protocol page.)
Also important to note: other than food allergies, all of the above sensitivities are caused by a damaged gut and/or gut dysbiosis, meaning they should go away when your gut heals, your gut bacteria normalize and your immune system is properly regulated. And including those foods in your diet, unless you have severe overt symptoms, may actually speed up your healing. If you aren’t sure, you should be working through this with a qualified healthcare professional.
If you do have a real food sensitivity that does limit your vegetable intake, then it’s important to work even harder within your restrictions to increase variety. You can do this by buying vegetables you aren’t familiar with when you see them in the store, shopping at Farmer’s Markets, natural/health food stores, cultural grocery stores and by checking out your local garden center for what unusual vegetables might grow in your backyard, or in a pot on your patio or in your kitchen window (you’d be surprised!).
Even when extra restrictions due to sensitivities constrain your choices, you can still eat variety (you just have to work a little harder and be a little more creative to source it).
Also, even if your choices are limited, your portions should still be large. Dr. Wahls’ 9 cups of vegetables per day (3 cups of greens, 3 cups colorful, and 3 cups cruciferous) has been shown to be therapeutic in clinical trials for multiple sclerosis (with gluten-free, dairy-free diets and no other diet changes). I personally aim for this as a bare minimum.
I delved into all of these issues in great detail in The Paleo Approach (complete with tons of references, which I apologize for not including in this post), but I thought this topic was important to discuss here. The important message is this: eating lots of veggies is an important part of the diet recommendations of The Paleo Approach and the autoimmune protocol. The only veggies you should be avoiding are legumes and nightshades (unless you have a diagnosed sensitivity, intolerance or allergy to other vegetables or fruit). It’s actually quite simply an important thing to do for health in general. And, the more variety you eat the better.