It is not an exaggeration to say that gut health is everything: the health of our guts has a profound effect on our overall health. As the connection between intestinal barrier function and health gains more recognition, the role that diet and lifestyle play in supporting gut health is being examined more intensively. Even more exciting, scientific studies can point to specific diet and lifestyle choices to heal a leaky gut.
What is a Leaky Gut?
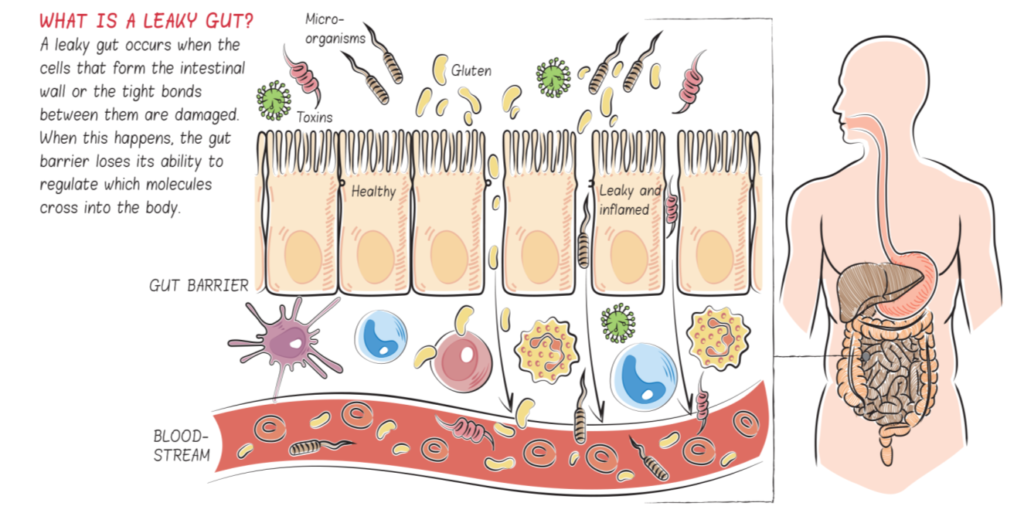
A leaky gut (more technically called increased intestinal permeability) occurs when the cells that form the intestinal wall of the small intestine (aka intestinal lining or intestinal barrier) or the tight bonds between them are damaged (see What Is A Leaky Gut? (And How Can It Cause So Many Health Issues?)). When this happens, the gut barrier loses its ability to regulate which molecules cross into the body. What leaks into the body is a variety of small substances—like incompletely digested proteins, other undigested food particles, bacteria or bacterial fragments, infectious organisms, and waste products—all of which stimulate the immune system.
Some substances cause generalized inflammation, where the signal to the immune system within the gut tissues spreads throughout the body. For example, when bacterial toxins such as lipopolysaccharide (also called endotoxin) leak into the body, systemic inflammation is triggered. Other substances stimulate targeted attacks by the immune system. For example, a food intolerance or allergy could result from incompletely digested food proteins leaking through the gut wall into the body. The many symptoms and health conditions related to leaky gut are caused by this stimulation of the immune system. Importantly, an immune system that’s chronically stimulated, as occurs in the context of a leaky gut, can end up attacking not just invaders like viruses and bacteria but also body tissues, which can contribute to chronic illnesses.
If you are concerned that you may have, or could develop, a leaky gut, then changing your diet to one that protects the gut is a natural next step for you. (Also see 5 Gut Health Tests You Can Do at Home)
What Causes a Leaky Gut?
It’s complicated. A perfect storm of food compounds, nutrient deficiencies, lifestyle factors, gut dysbiosis, infection and/or environmental factors collectively cause leaky gut.
Compounds in foods directly damage the gut barrier in two main ways: by adversely affecting the health of the cells that form the gut barrier or by interfering with how those cells bond together. Both cause the barrier to become permeable, or “leaky,” hence “leaky gut syndrome,” the umbrella term for chronic diseases associated with this problem.
Grains, legumes, dairy, and nightshades all contain substances that increase the permeability of the gut via direct damage both to enterocytes and to the junctions between them. These substances include prolamins (like gluten), agglutinins (like soy lectin), digestive enzyme inhibitors, glycoalkaloids, and phytic acid (see Are all lectins bad? (and what are lectins, anyway?), Why Grains Are Bad, Part 1, Lectins and the Gut, Wheat and Innate Immunity, How Do Grains, Legumes and Dairy Cause a Leaky Gut? Part 2: Saponins and Protease Inhibitors, and The WHYs behind the Autoimmune Protocol: Nightshades). Alcohol and sugar alcohols (like sucralose) also increase intestinal permeability via actions on the tight junctions. Some nutritional deficiencies are linked to leaky gut as well, including vitamins A and D.
Gut barrier integrity is also regulated by the gut microbiome, the collective community of microogranisms, their genes and their bioactive products that live within our gastrointestinal tracks. Various biotactive compounds produced by our gut bacteria regulate proteins that form the tight junction complexes. Thus, having a healthy, diverse and rich gut microbiome is a necessary precondition for a healthy gut barrier.
And, of course, the title of this article is a little misleading: food isn’t the only thing that affects gut barrier function. Both acute and chronic stress and overly strenuous activity are known to increase intestinal permeability (see How Stress Undermines Health and Why Exercising Too Much Hurts Your Gut).
Development of a Leaky Gut Summary:
- A healthy gut barrier is resilient to some stressors and toxins. It is normal for some large molecules to cross into the body, and it’s the immune system’s job to deal with them while remaining well regulated. This is called mucosal or immune tolerance.
- Minor intestinal permeability due to gut barrier defects results in an increased passage of large molecules into the body; however, (the maintenance of a stable environment inside and outside the cells) is maintained.
- Prolonged minor intestinal permeability results in an exaggerated immune response, causing damage to the gut barrier.
- The passage of more and more large molecules into the body leads to inflammation and immune system activation, which may result in the destruction of tight junctions and enterocyte cell death, leading to even greater passage of large molecules. This becomes a vicious cycle.
- Severe intestinal permeability develops and results in overactivation of the immune system, cell death, tissue damage, autoimmune disease, multi–organ system disorder, and chronic health problems.
If you are already battling health conditions related to having a leaky gut (again, see What Is A Leaky Gut? (And How Can It Cause So Many Health Issues?)), then you will have to be more strict with your dietary choices and also address other lifestyle factors like getting good quality sleep, managing stress, finding time for low-strain exercise, and getting outside.
How Do I Know If I Have a Leaky Gut?
A huge collection of health problems have been conclusively linked to leaky gut, including: ankylosing spondylitis, asthma, atopic dermatitis, cardiovascular disease, celiac disease, chronic fatigue syndrome, chronic heart failure, chronic inflammation, Crohn’s disease, depression, eczema, food allergy, HIV/AIDS, insulin resistance, irritable bowel syndrome, multiple organ failure, multiple sclerosis, non-alcoholic fatty liver disease, obesity, psoriatic arthritis, psychological conditions, rheumatoid arthritis, stroke, type 1 diabetes, type 2 diabetes, and ulcerative colitis.
However, a variety of less distinct symptoms or diagnoses can also point to the presence of a leaky gut, including: abdominal pain, bloating, burping, gas, irregular stools (constipation or diarrhea), nausea/vomiting, reflux/heartburn, acne, dry skin, eczema, hives, itchy skin, psoriasis, rashes, rosacea, ADD/ADHD, anxiety, brain fog, depression, fatigue, especially after eating, headaches, migraine, insomnia, aches and pains, autoimmune disease, difficulty maintaining a healthy weight, food sensitivities/allergies, joint pain, and symptoms of malnutrition.
In terms of testing, a lactulose mannitol ratio test is the only standard test available for intestinal permeability, but it’s not good at detecting what might be called mild leaky gut. Otherwise, a healthcare provider will evaluate a a combination of general inflammation, which you could measure with C-reactive protein, GI symptoms, disease symptoms, etc..
Healing Leaky Gut
Diet and lifestyle choices can be sufficient to completely correct gut health, but it’s important to know that certain underlying conditions (like persistent infections) can be a barrier to healing. This article summarizes important diet and lifestyle factors to support the healing process, but make sure you consult with a healthcare provider to pursue diagnosis and adjunct therapies, if required.
Supporting a healthy gut barrier requires the following:
- Avoiding food compounds that damage the gut barrier
- Focusing on nutrients important for gut barrier health
- Dialing in lifestyle factors that impact the gut barrier
- Supporting a healthy gut microbiome through diet and lifestyle
So, let’s dive into each of these in more detail.
Foods to Avoid to Heal Leaky Gut
The first and most important thing to do to heal a leaky gut is to stop eating foods that damage and inflame the gut lining! It can take six months or more for the gut to fully heal depending on the extent of the damage, the health of the gut microflora and your individual genetics. The food compounds that contribute to leaky gut can be quickly summarized:
Compounds in food that open tight junctions:
- Agglutinins (see Are all lectins bad? (and what are lectins, anyway?)
- Prolamins (via zonulin)
- Alcohols (see The WHYs behind the Autoimmune Protocol: Alcohol)
Compounds in food that can damage epithelial cells:
- Agglutinins
- Prolamins
- Saponins (glycoalkaloids, see The WHYs behind the Autoimmune Protocol: Nightshades)
Compounds in food that feed gut dysbiosis:
- Prolamins
- Agglutinins
- Alcohols
- Excess sugars and starch
- High omega-6 fatty acids
- Digestive enzyme inhibitors (see How Do Grains, Legumes and Dairy Cause a Leaky Gut? Part 2: Saponins and Protease Inhibitors)
- Emulsifiers (see Is It Paleo? Guar Gum, Xanthan Gum and Lecithin, Oh My!)
Until the gut is completely healthy, it is important to abstain from foods that contain the above compounds, which includes: grains, legumes (see The Green Bean Controversy and Pea-Gate), pseudograins, dairy products (some people may grass-fed dairy or A2 dairy), vegetables of the nightshade family (see What Are Nightshades?), additives in processed foods (many of which irritate the gut), vegetable oils, and refined sugars (which promote inflammation). Some people will also need to eliminate egg whites (see The WHYs behind the Autoimmune Protocol: Eggs) and limit nut consumption (see Nuts and the Paleo Diet: Moderation is Key). Changing your diet to avoid gut-irritating foods is critical. But, it is also important to include foods that can reduce inflammation and help heal the damaged gut.
Nutrients for Gut Health
Choosing nutrient-rich foods that support gut barrier and microbiota health in our digestive tract is an important tenet of the Paleo template. And for those with a confirmed or suspected leaky gut, focusing on specific nutrients known to be vital for gut health is necessary for healing. In fact, leaky gut can be caused by some nutrient deficiencies!. Specific nutrients important for gut barrier health are discussed in more detail in 8 Nutrients for Leaky Gut and in detail in Paleo Principles. The following is a summary of the most important nutrients for gut healing and the best food sources.
- Vitamin A: abundant in fish, liver, shellfish
- Vitamin D: abundant in fish, liver, mushrooms
- Zinc: abundant in oysters, red meat, poultry
- DHA and EPA (long-chain omega-3 fatty acids): abundant in fish, shellfish, sea vegetables
- Medium chain triglyceriedes (MCTs): abundant in coconut oil, palm oil
- Glycine: an amino acid abundant in bone broth, fish, red meat
- Glutamine: an amino acid abundant in fish, poultry, red meat (L-glutamine supplements are also available, see 8 Nutrients for Leaky Gut)
- Tryptophan: an amino acid abundant in shellfish, poultry, fish
- CoQ10: abundant in fatty fish, heart, red meat
- Soluble fiber: abundant in root vegetables, fruit, cruciferous vegetables
- Insoluble fiber: abundant in celery, cruciferous vegetables, leafy greens
- Flavonoids: abundant in berries, cruciferous vegetables, leafy greens
It’s also useful simply to eat foods that help reduce inflammation. It’s very important to be mindful of both your omega-6 and your omega-3 polyunsaturatedfatty acid intake. Omega-6 polyunsaturated fats, which are found in large quantities in modern vegetable oils, meat from grain-fed animals, and many nuts and seeds, increase inflammation. Omega-3 fatty acids, which are found in large quantities in wild-caught fish, pastured/free-range eggs, and meat from pastured animals, decrease inflammation. To help reduce overall inflammation and heal the gut, aim for a 1:1 ratio of omega-3 to omega-6 fatty acid intake in your diet. There are several ways of doing this: you can make sure that all of the meat in your diet is exclusively from grass-fed animals (beef, bison, goat or lamb); you can eat plenty of wild-caught seafood; and/or you can supplement with a good quality fish oil (note this is only advisable for a short-term intervention, say 4 to 6 weeks). Omega-3 fats are also extremely important for supporting a healthy gut microbiome.
Vegetables are rich in anti-oxidants, vitamins and minerals which help control inflammation (and help with just about every other normal function of the body!). Eating a variety of differently colored vegetables, a variety of dark green leafy vegetables, and a variety cruciferous vegetables (broccoli, cauliflower, cabbage, turnip greens, kale, Brussels sprouts, etc.) every day will provide all of the essential vitamins and minerals in a way that is easy for the body to absorb (no more need for a multivitamin!). Fruits, especially berries, are also a good source of antioxidants, vitamins and minerals.
It is also important to make sure you are getting enough Vitamin D. You can achieve this by spending some time outside in the sun every day and eating vitamin-D-rich foods regularly (like liver and seafood), or from taking high quality Vitamin D3 supplements. Read more about Vitamin D here.
Lifestyle Factors for Gut Health
When it comes to supporting gut health with lifestyle factors, the impacts are both on gut barrier and gut microbiome. Chronic stress increases intestinal permeability through CRH (see How Stress Undermines Health) and overtraining can increase intestinal permeability too (see Why Exercising Too Much Hurts Your Gut). Regular exercise and getting adequate sleep are well-known to increase biodiversity of gut microorganisms, supporting the growth of probiotic, beneficial strains (see Sleep and Disease Risk: Scarier than Zombies!.)
When it comes to supporting gut health, it’s also important to get 8+ hours of sleep on a consistent schedule every single night, live an active lifestyle (while avoiding overtraining), and manage stress.
Supporting a Healthy Gut Microbiome
Diet is the single biggest influence on gut microbiota composition. In fact, diet is directly responsible for more than 60% of the variation in bacterial species in the gut. So, eating the right foods can support the growth of good bacteria, while suppressing the growth of bad bacteria.
We know that inadequate fiber intake, high intake of omega-6 polyunsaturated fats (relative to omega-3s), high intake of saturated fat and low levels of vitamin D all cause a shift in the gut microbiota from probiotic to commensal, opportunitistic and pathogenic strains. In particular, inadequate fiber tends to shift the population of gut bacteria from majority Gram-positive strains (mainly those in the Firmucutes phylum) to more Gram-negative strains (mainly those in the Bacteroidetes phylum). High omega-6 fat intake depletes growth of both Firmicutes and Bacteroidetes phyla. And, high saturated fat intake skews microbiota unfavorably towards more Bilophila, Turicibacter, and Bacteroides. Vitamin D deficiency leads to shift toward pathogenic bacteria (Helicobacter, Veillonella and Erysipelotrichaceae), whereas supplementation restores levels of probiotic bacteria (Lactococcus, Akkermansia).
Some individual food compounds can also promote the growth of the wrong kinds of bacteria. Grains, dairy, legumes, nightshades, and alcohol are all known to contain compounds that can hinder the growth of beneficial strains of bacteria while supporting the growth of undesirable strains, like E. coli. These include agglutinins, prolamins, digestive enzyme inhibitors and alochols (including sugar alcohols). See Are all lectins bad? (and what are lectins, anyway?), Why Grains Are Bad-Part 1, Lectins and the Gut, Wheat and Innate Immunity, Is It Paleo? Splenda, Erythritol, Stevia and other low-calorie sweeteners and The WHYs behind the Autoimmune Protocol: Alcohol. Some emulsifiers also preferentially feed undesirable strains of bacteria (see Is It Paleo? Guar Gum, Xanthan Gum and Lecithin, Oh My!).
It’s not just a question of which kinds of bacteria our diet nourishes but also a question of bacterial metabolism (yep, the metabolome). Just as a high-sugar diet causes oxidative stress in our bodies (see Why Is Sugar Bad?), a high-sugar diet causes oxidative stress in our gut bacteria. Those bacteria adapt by altering their metabolism, which greatly affects our health.
The good news here is that the population of microbes in the gut (types, total and relative quantities, and location) adapts quite rapidly to changes in diet, in a matter of a few days to a few weeks.
- Dramatically increasing intake of fresh vegetables and fruit restores levels and diversity of probiotic species in as little as 3 to 4 days.
- Fish oil supplementation can restore levels of probiotic bacteria in about two weeks.
In fact, these are the two most important dietary factors for supporting healthy and diverse gut microbiota: eat plenty of whole vegetables and fruits, eat plenty of seafood, don’t go crazy on saturated fat. (Also see Saturated Fat: Healthful, Harmful, or Somewhere In Between?)
Lifestyle also plays a role here. Inadequate sleep, high chronic stress, living a sedentary lifestyle, and overtraining all negatively impact the microbial diversity and proportion of probiotic species in the gut. Living an active lifestyle, getting adequate sleep, and managing stress all support a healthy and diverse gut microbial community.
Exposure to probiotic organisms to inoculate the gut flora is also important. This is discussed in The Benefits of Probiotics and The Health Benefits of Fermented Foods. Natural sources of probiotics, include:
- Kombucha
- Kvass
- Milk kefir (can be made with coconut milk)
- Organic soil
- Raw lactofermented condiments (relishes, salsa)
- Raw lactofermented fruits (green papaya, chutney)
- Raw lactofermented vegetables (carrots, turnips, beets, pickles, kimchi)
- Raw sauerkraut
- Water kefir
- Yogurt (can be made with coconut milk or nut or seed milk)
Take-Home Message
 Really, the Paleo diet and the Autoimmune Protocol have gut health built right in! While these dietary changes may seem overwhelming, it is important to remember that making them will keep you healthy, put many diseases into remission, and prevent dozens of other diseases from developing. For the vast majority of people, using diet to prioritize gut health will mean a lifetime of good health.
Really, the Paleo diet and the Autoimmune Protocol have gut health built right in! While these dietary changes may seem overwhelming, it is important to remember that making them will keep you healthy, put many diseases into remission, and prevent dozens of other diseases from developing. For the vast majority of people, using diet to prioritize gut health will mean a lifetime of good health.
For more information, check out the Gut Health Fundamentals online course
Citations
Comprehensive references in The Paleo Approach and Paleo Principles
Johnston SD, Smye M, Watson RG, McMillan SA, Trimble ER, Love AH. Lactulose-mannitol intestinal permeability test: a useful screening test for adult coeliac disease. Ann Clin Biochem. 2000 Jul;37 ( Pt 4):512-9.
Fasano A. Leaky gut and autoimmune diseases. Clin Rev Allergy Immunol. 2012 Feb;42(1):71-8. doi: 10.1007/s12016-011-8291-x.
Mu Q, Kirby J, Reilly CM, Luo XM. Leaky Gut As a Danger Signal for Autoimmune Diseases.Front Immunol. 2017 May 23;8:598. doi: 10.3389/fimmu.2017.00598. eCollection 2017.
Ahmad R, Sorrell MF, Batra SK, Dhawan P, Singh AB. Gut permeability and mucosal inflammation: bad, good or context dependent. Mucosal Immunol. 2017 Mar;10(2):307-317. doi: 10.1038/mi.2016.128. Epub 2017 Jan 25.