Over the past century, few foods have overtaken our food supply quite like sugar and sweeteners. Yet despite decades of research, the relationship between added sugar and human health is still a controversial topic. Around the globe, public health guidelines—including the World Health Organization, the Dietary Guidelines for Americans, the Nordic Nutrition Recommendations, and Public Health England—recommend limiting added (or “free”) sugar intake to 10% of total calories or less, due to well-established effects on dental health, total caloric intake, obesity, inflammation, and related conditions. At the same time, some people question whether this upper limit is scientifically sound, leading to public confusion about how important it really is to avoid sugar.
Over the past century, few foods have overtaken our food supply quite like sugar and sweeteners. Yet despite decades of research, the relationship between added sugar and human health is still a controversial topic. Around the globe, public health guidelines—including the World Health Organization, the Dietary Guidelines for Americans, the Nordic Nutrition Recommendations, and Public Health England—recommend limiting added (or “free”) sugar intake to 10% of total calories or less, due to well-established effects on dental health, total caloric intake, obesity, inflammation, and related conditions. At the same time, some people question whether this upper limit is scientifically sound, leading to public confusion about how important it really is to avoid sugar.
Part of the confusion is due to aggressive action by the beverage industry (which relies on high-fructose corn syrup to sweeten drinks) to cast doubt on the validity of sugar research. For example, a systematic review published in December 2016 concluded that public health recommendations to reduce sugar intake were based on weak or inconclusive evidence, but this review was funded by the food and drink industry, which has a vested interest in neutralizing consumers’ negative perception of sugar and sugary foods.
In reality, the evidence for greatly reducing or avoiding consumption of processed sweeteners is compelling. Beginning with sucrose (table sugar) and continuing with high-fructose corn syrup and artificial and noncaloric sweeteners (like sucralose, aspartame, and stevia), these ingredients can be large contributors to chronic disease (see also Why is High Fructose Corn Syrup Bad For Us?, Is It Paleo? Fructose and Fructose-Based Sweeteners (I’m looking at you, Agave!), Is It Paleo? Splenda, Erythritol, Stevia and other low-calorie sweeteners, What’s the Next Superfood Sweetener? and The Trouble with Stevia). Even natural sweeteners like honey and maple syrup aren’t off the hook; although since they contain some redeeming nutritional features, they earn middle-ground status. See also Honey: The Sweet Truth About a Functional Food! and Blackstrap Molasses: The Sugar You Can Love!
 What Is Sugar and Why Is it Bad?
What Is Sugar and Why Is it Bad?
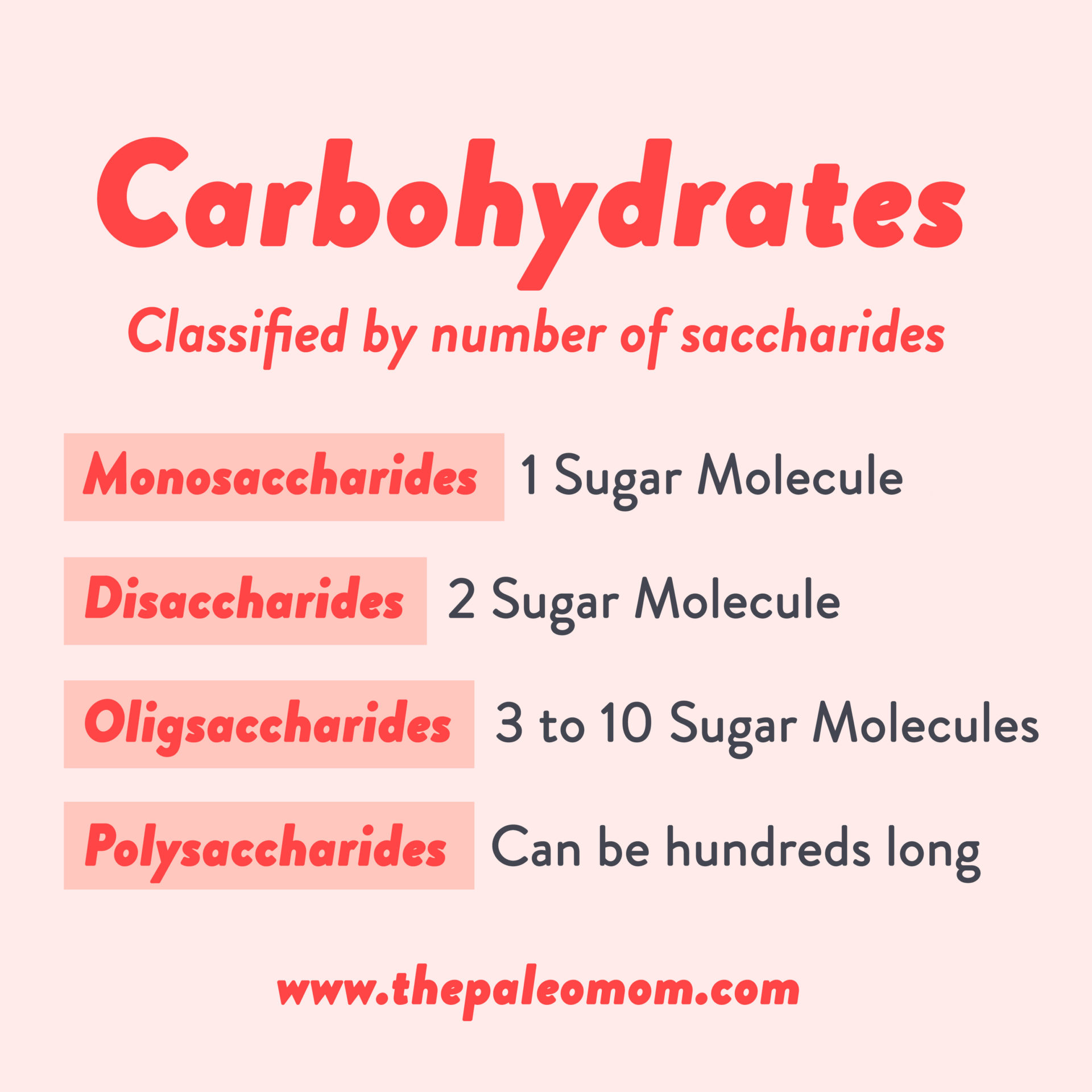
Carbohydrates are made up of sugar molecules, or saccharides, the most important and prevalent of which is glucose, the primary metabolic fuel for the human body and indeed most forms of life on Earth.
Chemically, carbohydrates are classified based on the number of saccharides they contain: monosaccharides are made up of a single sugar molecule, disaccharides contain two sugar molecules, oligosaccharides are medium-length chains of three to ten sugar molecules, and polysaccharides are long chains of sugar molecules that can be hundreds long.
From a dietary perspective however, it’s more relevant to classify carbohydrates based on how they’re digested and absorbed:
- Sugars, also called simple carbohydrates or simple sugars, include monosaccharides like glucose, fructose and galactose, and disaccharides like sucrose (one fructose and one glucose), lactose (one glucose and one galactose) and maltose (two glucoses). Sugars give food a sweet taste and are naturally found in fruit, dairy products and natural sweeteners like honey. They are digested and absorbed quickly and the glucose they contain has a rapid impact on blood sugar levels and insulin secretion. (Note that the presence of fiber in whole fruit helps to slow down the digestion of the sugars in fruit, see Why Fruit is a Good Source of Carbohydrates).
- Starches are complex carbohydrates, polysaccharides composed predominantly of glucose. Starch is produced by most plants as an energy storage molecule and is commonly found in grains, legumes, and root vegetables such as potatoes, sweet potatoes, and cassava. Starch takes longer to break down during digestion and has a more gradual impact on blood sugar levels. See also What is a Safe Starch?
- Fiber is also a complex carbohydrate, oligosaccharides and polysaccharides that don’t get fully broken down by our digestive enzymes and instead are fermented by the bacteria and other microorganisms that live in our digestive tracts. Fiber is discussed in detail starting in The Fiber Manifesto-Part 1 of 5: What Is Fiber and Why Is it Good?, The Fiber Manifesto-Part 2 of 5: The Many Types of Fiber, and The Fiber Manifesto-Part 3 of 5: Soluble vs. Insoluble Fiber.
Whole-food carbohydrates, like fruits and vegetables, contain a mix of simple and complex carbohydrates, including fiber which slows own digestion and blunts the blood sugar response. See Why Fruit is a Good Source of Carbohydrates, Why Root Veggies Are Great for the Gut Microbiome, and The Importance of Vegetables. Blood sugar regulation is further improved by ingesting fruits and vegetables as part of a complete meal that also includes protein and fats.
Refined carbohydrates refer to carbohydrates that have been processed. For example, when the bran and germ are milled away to make refined grain products, most of the fiber is removed. The resultant starches are digested and absorbed rapidly, sometimes raising blood glucose levels as quickly as simple sugars.
Simple sugars can also be refined. A prominent example of a processed sugar is high fructose corn syrup. In this case, corn syrup is treated with enzymes to turn a proportion of the syrup’s glucose into fructose. High fructose corn syrup is discussed further in Why is High Fructose Corn Syrup Bad For Us? , Is Fructose a Key Player in the Rise of Chronic Health Problems? and Fructose and Vitamin D Deficiency: The Perfect Storm?.
Nutrivore Weekly Serving Matrix
An easy-to-use and flexible weekly checklist
to help you maximize nutrient-density.
The Weekly Serving Matrix is very helpful! I’ve been eating along these lines but this really helps me know where to focus vs. which foods serve a more secondary role. It’s super helpful and has taken a lot of worry out of my meal planning. Thanks!
Jan
Sugar Metabolism, AKA the Krebs Cycle
Most of the digestible carbohydrates that we consume break down into glucose, which is absorbed into our blood stream and shuttled into our cells by insulin. Once in our cells, glucose is converted into adenosine triphosphate (ATP), the energy currency for all cells, in a series of chemical reactions, collectively referred to as cellular respiration (since the process uses oxygen and produces carbon dioxide). Many ATP molecules can be formed from a single glucose molecule. Glucose molecules are first converted into pyruvate via glycolysis which yields some ATP. Pyruvate then enters the mitochondria where it is oxidized into acetyl-CoA, which can also yield some ATP. Acetyl-CoA is then converted into more ATP in what is called the Krebs or citric acid cycle, an 8-step process involving 18 different enzymes and co-enzymes. Other high-energy products of the Krebs cycle (NADH and FADH2) are converted into yet more ATP in the last step of cellular respiration, oxidative phosphorylation in the electron transport chain.
This is complex biochemistry; the important part here is that there’s a whole lot of chemical reactions required to make sugar into a useable energy source for our cells!
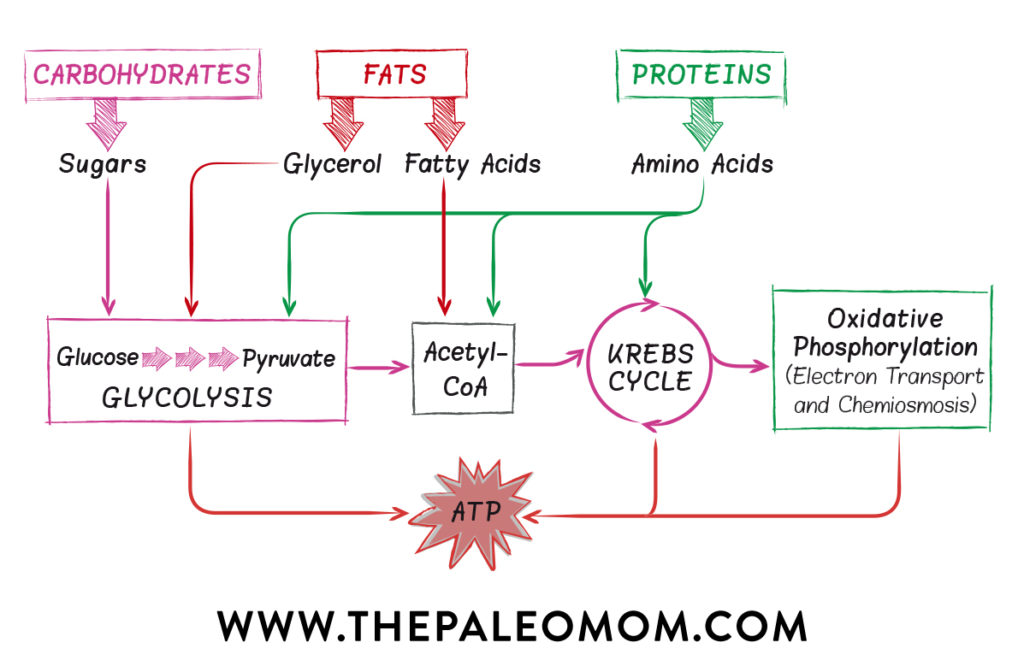
Glucose isn’t the only molecule that can be converted into ATP via cellular respiration. Protein (amino acids), fats (fatty acids and glycerol), and other carbohydrates (like fructose) can be converted to various intermediates of glycolysis, pyruvate oxidation and the Krebs cycle, allowing them to slip into the cellular respiration pathway at multiple points. However, glucose is the easiest to convert into ATP (it requires the least amount of oxygen and can even produce some ATP anaerobically) so it is the preferred fuel for cells. In between meals, once the glucose that enters the bloodstream has been used up, cells metabolize stored fat and glycogen (stored carbohydrates) for energy. A flexible metabolism is one that can easily switch between carbohydrates and fats, depending on what’s available. Although protein is not a preferred source of energy, it can be used if needed—this is why people lose muscle mass in addition to fat stores when they are too severely calorically restricted, fasting, or starving. See also Adverse Reactions to Ketogenic Diets: Caution Advised, Intermittent Fasting: Secret to Weight Loss or Dangerous Fad? and, Paleo for Weight Loss.
 Sugar, Insulin and Inflammation
Sugar, Insulin and Inflammation
Where does inflammation fit into this picture? A byproduct of cellular respiration is the production of reactive oxygen species (ROS), aka oxidants or free radicals. Reactive oxygen species (ROS) are a group of chemically reactive molecules that contain oxygen. ROS have important roles in cell signaling (the complex communication between and within cells) and in homeostasis (the maintenance of a stable environment inside and outside the cell). But ROS are also potent signals for inflammation and can damage cells and tissue. In fact, they are produced and secreted by the cells of the immune system as one weapon in its arsenal to defend us from pathogens.
In general, the more energy (food) consumed, the more ROS produced. This production of ROS after meals is called postprandial oxidative stress or postprandial inflammation, and it continues to be a topic of intense study. In this sense, all foods are inflammatory—it is the price we pay for being aerobic organisms, of course our use of oxygen in our metabolism is also what allows us to have such wonderfully complex biological structure (anaerobic organisms are almost all single cell). However, some eating patterns cause more oxidative stress and inflammation than others. Overeating in general is the biggest culprit, stimulating the production of ROS by flooding the body with energy, but so does high carbohydrate (especially refined carbohydrate) intake, even in the context of judicious caloric intake. High-carbohydrate diets cause more postprandial inflammation than low-carbohydrate diets do, everything else being equal. Put simply, the more glucose we eat, the more inflammation!
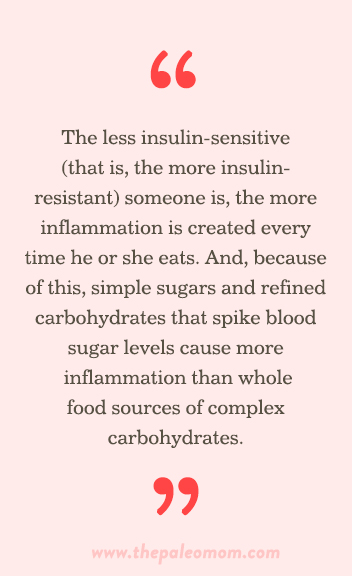
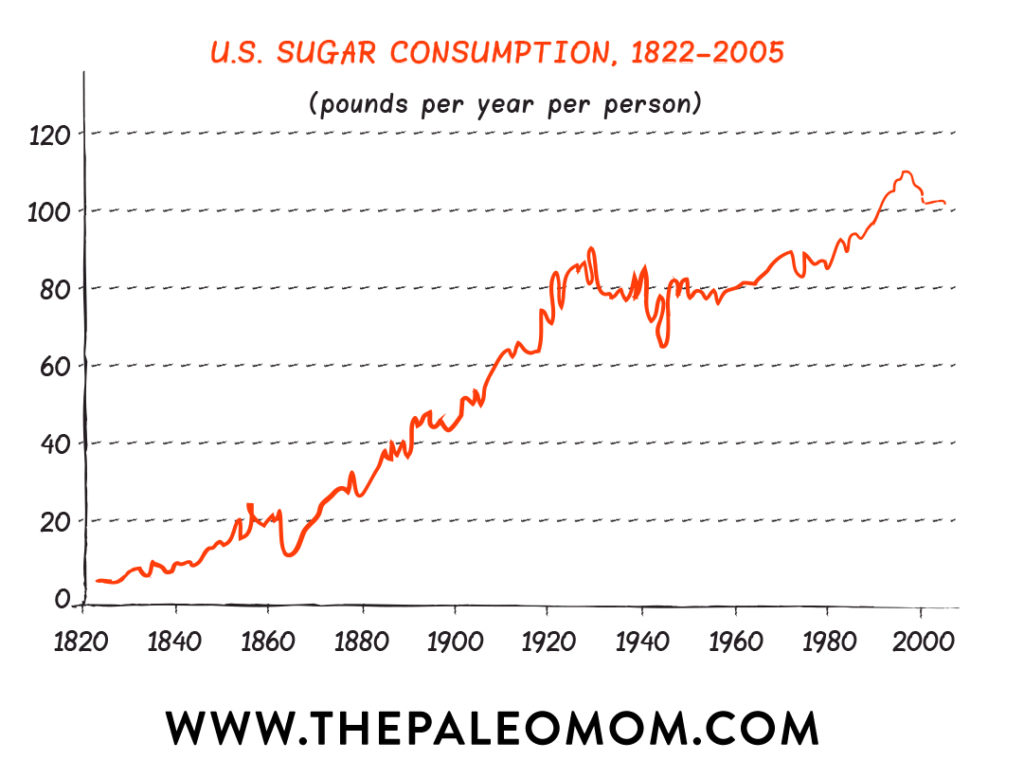
When it comes to sugar being inflammatory, dose matters. Today, the average American consumes almost 152 pounds of sugar each year, a staggering amount of refined simple carbohydrates equivalent to 6 cups of white sugar every week. This may be the single biggest dietary contributor to the rise in chronic disease. Consumption of glucose is associated with increased production of ROS and markers of inflammation, even in healthy people. However, it is exaggerated in people who are obese or have type 2 diabetes, high cholesterol, or metabolic syndrome. This is because postprandial inflammation is proportional to insulin sensitivity, or how effectively the body responds to insulin: the less insulin-sensitive (that is, the more insulin-resistant) someone is, the more inflammation is created every time he or she eats. And, because of this, simple sugars and refined carbohydrates that spike blood sugar levels cause more inflammation than whole food sources of complex carbohydrates.
A healthy body has the ability to control both the amount of and the damage caused by ROS. In normal circumstances, the deleterious effects of these highly reactive molecules are balanced out by antioxidants—certain vitamins, minerals, and most phytochemicals (see also The Importance of Vegetables, The Amazing World of Plant Phytochemicals: Why a diet rich in veggies is so important! and Polyphenols: Magic Bullet or Health Hype?). However, when the production of ROS exceeds the availability of antioxidants, the resulting imbalance causes problems. Specifically, the overproduction of ROS stimulates inflammation and damages cells and tissue; this is called oxidative stress.
There is evidence that insulin itself is pro-inflammatory. A study of healthy subjects with controlled (and normal) blood glucose who were intravenously infused with insulin and glucose to achieve hyperinsulinemia (elevated blood insulin) showed that hyperinsulinemia caused an exaggerated inflammatory response to endotoxin (a toxin from the cell wall of Gram-negative bacteria like E. coli). An exaggerated stress response was also observed, meaning that hyperinsulinemia also contributes to increased cortisol. Another study measured the levels of fasting insulin (the levels recorded first thing in the morning) in volunteers with normal blood sugar levels and found that those with higher fasting insulin levels also had more markers of inflammation, like C-reactive protein, or CRP. In a person who is insulin-resistant, the pancreas secretes more and more insulin to handle elevated blood sugar, which contributes to inflammation and insulin resistance. See also The Paleo Diet for Diabetes, The Hormones of Fat: Leptin and Insulin, The Hormones of Hunger, The Case for More Carbs: Insulin’s NonMetabolic Roles in the Human Body and 3 Ways to Regulate Insulin that Have Nothing to Do With Food.
We have been eating exponentially more sugar over the last century, especially in the last three or four decades. This increase is largely because whole food sources of carbohydrates have been replaced with refined carbohydrates and added sugars in processed and manufactured foods. It just so happens that while sugar consumption has increased so have obesity, diabetes, cardiovascular disease, cancer, and autoimmune disease. While the evidence for a causal relationship between sugar consumption and these diseases remains preliminary, there is ample evidence for a link between sugar consumption and inflammation.
Non-Caloric Sweeteners Are Even Worse
Humans have a sweet tooth, which means that as we learn the importance of limiting sugar intake, we are instinctively drawn to sugar substitutes. Unfortunately, there just isn’t any way to cheat sweet and all sugar substitutes, even natural ones like stevia, are riddled with problems. By swapping out sugar for sweeteners, we’re going from the frying pan into the fire.
These are discussed in more detail in:
- Is It Paleo? Fructose and Fructose-Based Sweeteners (I’m looking at you, Agave!),
- Is It Paleo? Splenda, Erythritol, Stevia and other low-calorie sweeteners,
- The Trouble with Stevia
- What’s the Next Superfood Sweetener?
From a health perspective, high-fructose corn syrup and artificial sweeteners should be eliminated completely along with natural non-caloric sweeteners like stevia. And the evidence clearly shows that sugar (in large quantities) should not be a staple in our diets (see How many carbs should you eat?).
What About Natural Sugars?
But what about natural sweeteners like honey, molasses, and maple syrup, or less-refined versions of cane sugar? The good news is that small amounts of natural sugars are unlikely to be harmful and can even contribute some valuable micronutrients to our diets (see The Importance of Nutrient Density). The bad news is that it’s still a case of “the dose makes the poison”: these foods become harmful when they start displacing more-nutritious items from the menu or when they increase our energy intake beyond what we need. Therefore, they’re conditionally allowed on a nutrient-focused health-promoting diet like the Paleo diet and the Autoimmune Protocol.
How do natural sugars differ from refined table sugar and high-fructose corn syrup?
In most cases, the ratio of glucose to fructose (after we’ve consumed and metabolized the sweetener) is actually very similar: about 50% glucose and 50% fructose (keeping in mind that sucrose is broken down into equal parts fructose and glucose in our bodies). The biggest exception is agave syrup, which is in the “avoid” list due to its extremely high fructose content (up to 85% or higher); see Is It Paleo? Fructose and Fructose-Based Sweeteners (I’m looking at you, Agave!).
The main reason natural sugars are considered superior to highly refined table sugar and high-fructose corn syrup has to do with micronutrients.
Raw honey contains small amounts of vitamins A, B1, B6, B9, B12, C, D, and E, as well as calcium, sodium, phosphorus, magnesium, silicon, iron, manganese, and copper. Honey also stands out from other sugars because it supports the gut microbiome and even has anti-diabetic effects (see also Honey: The Sweet Truth About a Functional Food!).
Maple syrup contains small amounts of manganese and zinc.
Unrefined cane sugar (sucanat, evaporated cane juice, muscovado/Barbados sugar, rapadura sugar, or jaggery) contains small amounts of vitamins A, B1, B2, B3, B5, and B6, along with calcium, iron, magnesium, zinc, copper, chromium, phosphorus, manganese, sodium, and potassium. By contrast, white sugar, brown sugar, and turbinado sugar (“raw sugar”) contain close to zero micronutrients. Date sugar and coconut sugar contain some fiber, slowing down the glycemic response.
Among the natural sweeteners, though, molasses is king (see Blackstrap Molasses: The Sugar You Can Love!). Its nutritional content is exceptional, and while it should be used in moderation like any sweetener, it can make some truly beneficial contributions to our diets.
However, all natural sweeteners can be used in moderation and occasionally. What does that mean? Well, the scientific evidence of staying below 10% of total calories from added sugars, even natural ones, is quite compelling. If you follow a 2,000 calorie per day, otherwise nutrient-dense, whole foods diet, up to about 3 tablespoons of honey would qualify. I recommend thinking of this as a maximum, and remembering that the primary criterion for whether or not a diet is health promoting is nutrient sufficiency (see also The Importance of Nutrient Density, 7 Nutrients You’re Probably Deficient In and 5 Nutrients You’re Deficient In… If You Eat Too Much Sugar).
The Best Natural Sugars to Choose
The trick with all natural sugars and sweeteners is to keep your intake moderate and occasional. When you do want a treat, a natural sugar with some micronutrient content is the best choice.
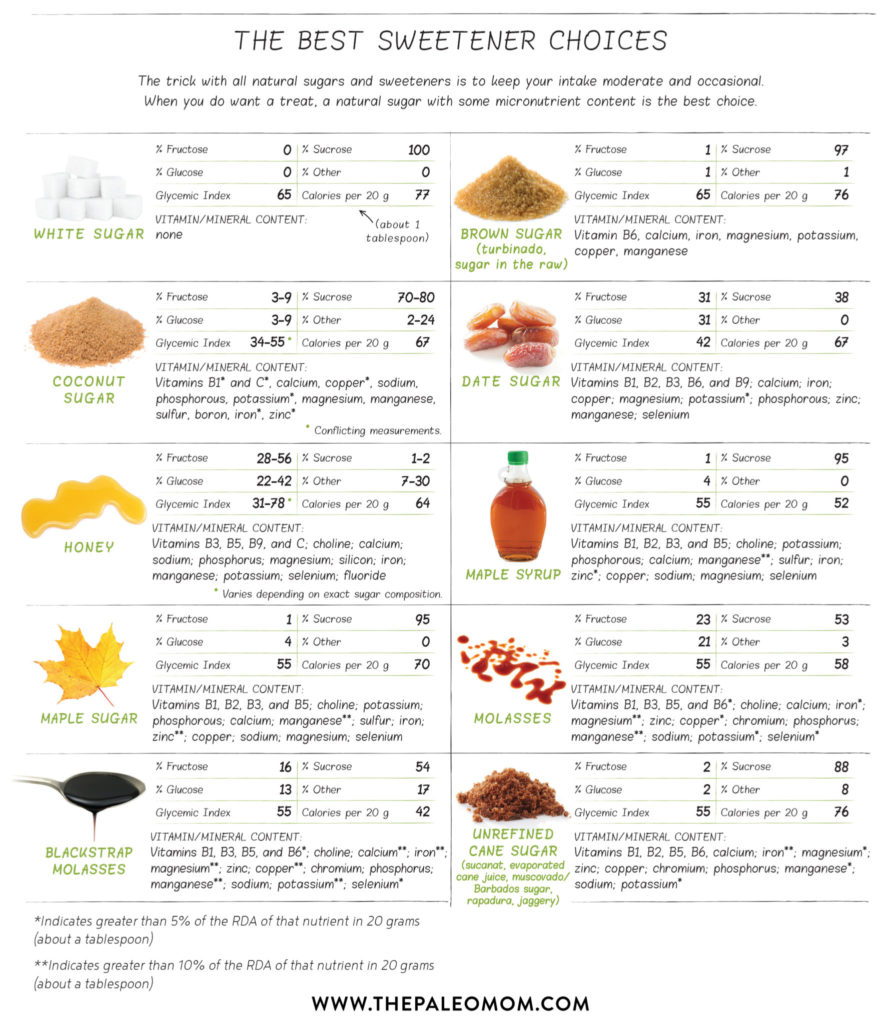
Note: Exact saccharide content can vary depending on exactly where and how these sugars are produced; the numbers in this table may not reflect the version you have purchased. Honey is especially variable in its glucose and fructose content. Also note that there is very limited and conflicting data on coconut sugar.
Now, don’t get excited at the long list of vitamins and minerals in some of these natural sugars. With the exception of molasses, especially blackstrap molasses, (see Blackstrap Molasses: The Sugar You Can Love!), the amounts that you would need to eat in order for the micronutrient content to contribute meaningfully to your diet would far exceed what could be classified as moderate.
How Many Carbohydrates Should We Eat?
The takeaway here is that blood sugar regulation is essential for controlling inflammation. The Western diet is typified by the excessive consumption of calorie-dense, nutrition-poor foods that cause abnormal surges in blood glucose with little in the way of dietary antioxidants to balance things out. But, avoiding excess sugars does not mean that we should aim to eat a “low-carb diet”. In fact, the current state of evidence is that whole food carbohydrates like fruit and root vegetables is a necessity for healthy hormones, improved body composition, cognitive and mental health, and the health of our gut microbiomes. (see The Case for More Carbs: Insulin’s NonMetabolic Roles in the Human Body, How many carbs should you eat?, Paleo, Resistant Starch, and TMAO: New Study Warning Worth Heeding and Carbs Vs. Protein Vs. Fat: Insight from Hunter-Gatherers). Somewhere around 200 – 250 grams of carbohydrates from whole vegetables and fruits is a good target for most people.
Citations
Akgun S & Ertel NH. “The effects of sucrose, fructose, and high-fructose corn syrup meals on plasma glucose and insulin in non-insulin-dependent diabetic subjects.” Diabetes Care. 1985 May-Jun;8(3):279-283.
Anderson RA. “Chromium, glucose intolerance and diabetes.” J Am Coll Nutr. 1998 Dec;17(6):548-55.
Anderson RA, et al. “Urinary chromium excretion and insulinogenic properties of carbohydrates.” Am J Clin Nutr. 51:864–868.
Basciano H, et al. “Fructose, insulin resistance, and metabolic dyslipidemia.” Nutr Metab (Lond). 2005 Feb 21;2(1):5.
Bray GA, et al. “Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity.” Am J Clin Nutr. 2004 Apr;79(4):537-43.
Djurhuus MS, et al. “Insulin increases renal magnesium excretion: a possible cause of magnesium depletion in hyperinsulinaemic states.” Diabet Med. 1995 Aug;12(8):664-9.
Johnson RJ, et al. “Potential role of sugar (fructose) in the epidemic of hypertension, obesity and the metabolic syndrome, diabetes, kidney disease, and cardiovascular disease.” Am J Clin Nutr. 2007 Oct;86(4):899-906.
Kozlovsky AS, et al. “Effects of diets high in simple sugars on urinary chromium losses.” Metabolism. 1986 Jun;35(6):515-8.
Lemann J, et al. “Evidence that glucose ingestion inhibits net renal tubular reabsorption of calcium and magnesium in man.” J. Clin Invest. 1970 Apr;75(4):578-85.
Lennon EJ & Piering WF. “A comparison of the effects of glucose ingestion and NH4Cl acidosis on urinary calcium and magnesium excretion in man.” J Clin Invest. 1970 Jul;49(7):1458-65.
Lennon EJ, et al. “The effect of glucose on urinary cation excretion during chronic extracellular volume expansion in normal man.” J Clin Invest. 1974 May;53(5):1424-33.
Rolls, B. J., Effects of intense sweeteners on hunger, food intake, and body weight: a review, Am J Clin Nutr. 1991;53(4):872-8
“US Consumption of Caloric Sweeteners: Table 52.” United States Department of Agriculture Economic Research Service. Accessed August 6, 2016.
“Blackstrap Molasses. In-Depth Nutritional Analysis.” World’s Healthiest Foods. Accessed November 5, 2015.
Ensminger ME & Ensminger AH. “Foods and Nutrition Encyclopedia, 2nd Edition.” CRC Press, 1993: page 83.
“Glycemic Index.” The University of Sydney. http://www.glycemicindex.com
Nath A, et al. “Review on recent advances in value addition of jaggery based products.” J Food Process Technol. 2015;6:4
Secretaria, et al. “Comparison of the Elemental Content of 3 Sources of Edible Sugar.” The Philippine Food and Nutrition Research Institute. Analyzed by PCA-TAL, Sept. 11, 2000. 2003. In parts per million (ppm or mg/li).
“USDA Food Composition Databases.” United States Department of Agriculture. Agricultural Research Service. https://ndb.nal.usda.gov/ndb/